-
Original Article
Association between Hormonal Contraception and Injuries Induced by Human Papillomavirus in the Uterine Cervix
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):196-202
04-01-2018
Summary
Original ArticleAssociation between Hormonal Contraception and Injuries Induced by Human Papillomavirus in the Uterine Cervix
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):196-202
04-01-2018Views120See moreAbstract
Objective
To evaluate the association between hormonal contraception and the appearance of human papillomavirus HPV-induced lesions in the uterine cervix of patients assisted at a school outpatient clinic - ObGyn outpatient service of the Universidade do Sul de Santa Catarina.
Methods
A case-control study, with women in fertile age, performed between 2012 and 2015. A total of 101 patients with cervical lesions secondary to HPV were included in the case group, and 101 patients with normal oncotic colpocytology, in the control group. The data were analyzed through the Statistical Package for the Social Sciences (SPSS, IBM Corp. Armonk, NY, US) software, version 24.0, using the 95% confidence interval. To test the homogeneity of the proportions, the chi-square (χ2) test was used for the qualitative variables, and the Student t-test, for the quantitative variables.
Results
When comparing the occurrence of HPV lesions in users and non-users of combined oral contraceptives (COCs), the association with doses of 0.03 mg or higher of ethinylestradiol (EE) was observed. Thus, a higher probability of developing cervical lesions induced by HPV was identified (odds ratio [OR]: 1.9 p = 0.039); and when these cases were separated by the degree of the lesion, the probability of these patients presentingwith lowgrade squamous intraepithelial lesion was 2.1 times higher (p = 0.036), but with no impact on high-grade squamous intraepithelial lesions and the occurrence of invasive cancer. No significant differences were found in the other variables analyzed.
Conclusion
Although the results found in the present study suggest a higher probability of the users of combined hormonal contraceptives with a concentration higher than 0.03 mg of EE to develop low-grade intraepithelial lesions, more studies are needed to conclude causality.
-
Original Article
Management of Atypical Squamous Cell Cases: A Prospective Study of Women seen at a Private Health Service in Northeastern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(3):121-126
03-01-2018
Summary
Original ArticleManagement of Atypical Squamous Cell Cases: A Prospective Study of Women seen at a Private Health Service in Northeastern Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(3):121-126
03-01-2018Views134Abstract
Objective
To assess the management chosen by gynecologists after atypical squamous cells (ASCs) cytology results, and to evaluate the outcomes of these cases in Brazilian women.
Methods
A prospective observational study evaluated the initial management offered by the gynecologist in the case of 2,458 ASCs cytology results collected between January of 2010 and July of 2016. The outcomes of the cytology, high-risk human papilloma virus (HR-HPV) test and histology were compared in two subgroups: atypical squamous cells of undetermined significance (ASC-US) and atypical squamous cells-cannot exclude high-grade squamous intraepithelial lesion (ASC-H).
Results
In many cases of ASC-US (36.97%) and ASC-H (40.50%), no clinical actions were taken. Cytology was the most frequent follow-up chosen, including for cases of ASC-H, which goes against the conduct recommended in the national guideline. In women over 30 years of age, the period of time elapsed between an ASC-US result and a new cytology was in 13.03 months, in disagreement with the national guideline recommendations (p< 0.0001). Negative for intraepithelial lesions or malignancy (NILM) cytologic (p = 0.0026) and histologic (p = 0.0017) results in the follow-up were associated with prior ASC-US, while negative results for ASC-H were cytologically (p< 0.0001) and histologically associated with high-grade squamous intraepithelial lesion (HSIL) (p< 0.0001). Two invasive cervical carcinomas (ICCs) were found in the follow-up for ASC-H, and there was a statistically significant association (p = 0.0341). A positive HR-HPV test was associated with ASC-H (p = 0.0075).
Conclusion
The data suggest that even for a population of Brazilian women assisted at private clinics, the national guidelines recommendations for ASCs results are not followed.
Key-words atypical squamous cells of the cervixdisease managementHuman papillomavirusPapanicolaou testUterine cervical neoplasmSee more -
Original Article
Detection of High-Risk Human Papillomavirus in Cervix Sample in an 11.3-year Follow-Up after Vaccination against HPV 16/18
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(8):408-414
08-01-2017
Summary
Original ArticleDetection of High-Risk Human Papillomavirus in Cervix Sample in an 11.3-year Follow-Up after Vaccination against HPV 16/18
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(8):408-414
08-01-2017Views171Abstract
Purpose
the aim of this study was to evaluate the pattern of human papillomavirus (HPV) detection in an 11.3-year post-vaccination period in a cohort of adolescent and young women vaccinated or not against HPV 16/18.
Methods
a subset of 91 women from a single center participating in a randomized clinical trial (2001-2010, NCT00689741/00120848/00518336) with HPV 16/18 AS04- adjuvanted vaccine was evaluated. All women received three doses of the HPV vaccine (n = 48) or a placebo (n = 43), and cervical samples were collected at 6-month intervals. Only in this center, one additional evaluation was performed in 2012. Up to 1,492 cervical samples were tested for HPV-DNA and genotyped with polymerase chain reaction (PCR). The vaccine group characteristics were compared by Chi-square or Fisher exact or Mann-Whitney test. The high-risk (HR)-HPV 6-month-persistent infection rate was calculated. The cumulative infection by HPV group was evaluated by the Kaplan-Meier method and the log-rank test.
Results
the cumulative infection with any type of HPV in an 11.3-year period was 67% in the HPV vaccine group and 72% in the placebo group (p = 0.408). The longitudinal analysis showed an increase of 4% per year at risk for detection of HR-HPV (non-HPV 16/ 18) over time (p = 0.015), unrelated to vaccination. The cumulative infection with HPV 16/18 was 4% for the HPV vaccine group and 29% for the placebo group (p = 0.003). There were 43 episodes of HR-HPV 6-month persistent infection, unrelated to vaccination.
Conclusions
this study showed themaintenance of viral detection rate accumulating HR-HPV (non-HPV-16-18) positive tests during a long period post-vaccination, regardless of prior vaccination. This signalizes that the high number of HPV-positive testsmay be maintained after vaccination.
Key-words Cervix uteriHPV DNA testsHuman papillomavirushuman papillomavirus vaccine 16 and 18 L1 VLPpapillomavirus vaccinesPolymerase chain reactionSee more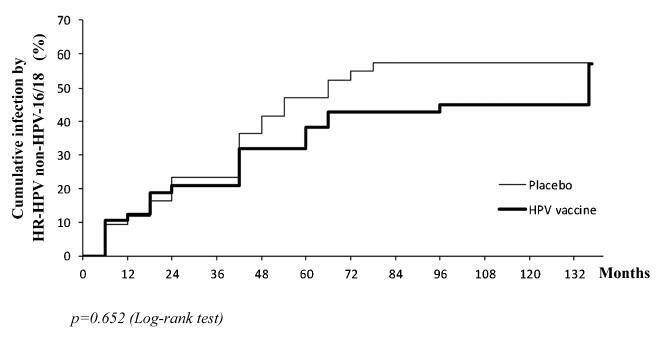
-
Case Report
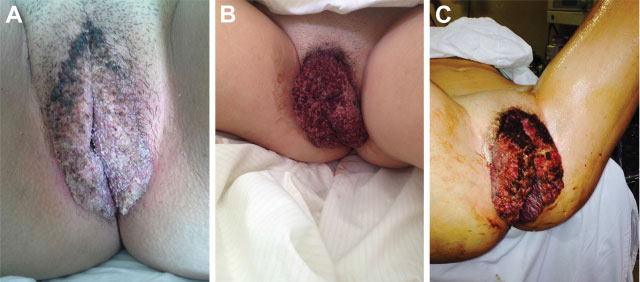
Giant Condyloma (Buschke-Loewenstein Tumor) in a 16-year-old Patient: Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):471-476
09-01-2016
Summary
Case ReportGiant Condyloma (Buschke-Loewenstein Tumor) in a 16-year-old Patient: Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):471-476
09-01-2016Views172See moreAbstract
The Buschke-Loewenstein tumor is characterized by excessive growth of verrucous lesions on the genitals and/or perianal region. It is considered benign despite the high rate of recurrence and the possibility of malignant transformation. It is commonly associated with subtypes 6 and 11 of the human papillomavirus (HPV), and host 's immunity plays an important role in the development of the disease. Surgical excision is the recommended treatment in most cases. We present the case of a 16 years old female patient with extensive vulvar lesions successfully treated surgically.
-
Artigos Originais
Genotype distribution of human papillomavirus in women from the state of Bahia, Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(9):416-422
09-01-2014
Summary
Artigos OriginaisGenotype distribution of human papillomavirus in women from the state of Bahia, Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(9):416-422
09-01-2014DOI 10.1590/SO100-720320140004995
Views69See morePURPOSE:
The aim of this study was to evaluate the human papillomavirus genotypes and the frequency of multiple human papillomavirus infections, as well as to assess the association between human papillomavirus genotype, cyto-histopathological abnormalities and age range.
METHODS:
A retrospective cross-sectional study was carried out between June 2010 and October 2013 in Salvador, Bahia, Brazil. We analyzed 351 results of positive human papillomavirus genotyping performed using the PapilloCheck(r) test, designed to detect 24 human papillomavirus types. The cyto-histopathological abnormalities were classified as negative (negative cytology and histopathology), low-grade lesions (cytologic low-grade squamous intraepithelial lesion diagnosis or histopathologic cervical intraepithelial neoplasia 1 or vaginal intraepithelial neoplasia 1 diagnosis) and high-grade lesions (cytologic high-grade squamous intraepithelial lesion diagnosis or histopathologic cervical intraepithelial neoplasia 2+ or vaginal intraepithelial neoplasia 2+ diagnosis).
RESULTS:
The most frequently detected high risk human papillomavirus genotype was HPBV 16, with 18.5%, 95% confidence interval (95%CI) 14.6-23.0, followed by HPV 56 (14%; 95%CI 10.5-18.0) and HPV 39 (13.4%; 95%CI 9.5-16.8). HPV 18 (5.4%; 95%CI 3.3-8.3) was among the least frequent types. Among the low risk types, HPV 42 (15.7%; 95%CI 12.0-20.0), HPV 6 (11.4%; 95%CI 8.3-15.2) and HPV 44/55 (11.1%; 95%CI 8.0-14.9) were the most frequent, while HPV 11 (2.8%; 95%CI 1.4-5.2) was the least common. The proportion of HPV 16-positive women increased with severity of cyto-histopathological abnormalities: 13.8% (12/87) in low-grade lesion and 42.4% (14/33) in high-grade lesion. There was association between low- or high-grade cyto-histopathological lesion and the high risk genotypes, HPV16, HPV 52, HPV 73 and HPV 82, and the low risk type, HPV 43. Women under 30 years showed a significantly higher frequency of HPV 16 (22.2 versus 12.9%, p =0.01), HPV 42 (19.7 versus 10.9%, p=0.01) and HPV 45 (6.6 versus 1.4%, p=0.01), and multiple human papillomavirus infections (58.1 versus 47.4%, p=0.04).
CONCLUSIONS:
We observed variability of human papillomavirus genotype distribution in women from the state of Bahia. HPV 16 was the most frequently detected high risk human papillomavirus, as also reported for other geographic areas of Brazil and for the world in general. HPV 56 and HPV 39 were the second and the third most common genotypes, whereas HPV 18 was among the least frequent types. HPV 42, 6 and 44/55 were the most frequently detected low risk human papillomavirus, and HPV 11 was the least common.
-
Revisão
Cervical intraepithelial neoplasia: diagnosis and treatment
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):425-433
11-16-2005
Summary
RevisãoCervical intraepithelial neoplasia: diagnosis and treatment
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(7):425-433
11-16-2005DOI 10.1590/S0100-72032005000700010
Views69Cervical cancer is nowadays a disease amenable to secondary prevention. Methods for the detection of its precursor lesions and human papillomavirus infection, such as cervical cytology and molecular biology, achieved widespread use worldwide. However, there is still too much controversy regarding the use of these methods in gynecological practice. Which is the best examination or the best association of examinations, and the most adequate time intervals to proceed with screening, are still pending questions, generating anxiety in patients and doctors. On the other hand, the management of women who have been diagnosed with viral infection and/or cervical intraepithelial neoplasia is not yet consensual, and several factors may affect the clinical decision on how to treat them. Therapeutic options are dependent upon the type of viral infection, severity of the cervical intraepithelial neoplasia and its histological type. The aim of the present article was to review the several aspects of cervical cancer screening and its viable treatment.
Key-words Cervical intraepithelial neoplasia/diagnosisCervical intraepithelial neoplasia/prevention & controlCervical intraepithelial neoplasia/therapyHuman papillomavirusSee more -
Trabalhos Originais
Histological results and HPV detection in women with pap smear showing atypical squamous cells of undetermined significance and low-grade squamous intraepithelial lesion
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(6):457-462
09-02-2004
Summary
Trabalhos OriginaisHistological results and HPV detection in women with pap smear showing atypical squamous cells of undetermined significance and low-grade squamous intraepithelial lesion
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(6):457-462
09-02-2004DOI 10.1590/S0100-72032004000600006
Views121See moreOBJECTIVE: to assess the ability of Pap smear and hybrid capture II (HCII) to detect clinically significant cervical lesions (CIN2/3) in women referred to hospital due to atypical squamous cells of unknown significance (ASCUS) or low-grade squamous intraepithelial lesions (LSIL). METHODS: a cross-sectional study comprising 161 women referred to the Taubaté University Hospital due to ASCUS/LSIL, between August 2000 and September 2002. All women responded to a questionnaire regarding sociodemographic and reproductive characteristics and were subjected to gynecological examination with specimen collection for Pap test and HCII, along with colposcopy and eventual cervical biopsy. The relationship between HCII results and age, use of condom, oral hormonal contraception, and smoking were evaluated by the chi-square test. The sensitivity, specificity, positive and negative predictive values of both Pap test and HCII were calculated. All calculations were performed within 95% confidence intervals. RESULTS: sixty-seven percent of the women that tested positive for HPV were less than 30 years old. Pap smear and HCII showed the same 82% sensitivity in detecting CIN2/3 when the threshold for a positive Pap result was ASCUS, LSIL or HSIL. Pap smear specificity and positive predictive values were substantially increased when only HSIL results were considered as positive (from 29 to 95% and 12 to 50%, respectively). These figures were superior to those of HCII, but at the expense of an expressive loss of sensitivity (from 82% to 41%). CONCLUSIONS: our results substantiate the potential of HCII in detecting CIN2/3 among women referred due to ASCUS/LSIL.
-
Trabalhos Originais
Behavioral factors and changes in the number of Langerhans’ cells
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(4):289-294
07-20-2004
Summary
Trabalhos OriginaisBehavioral factors and changes in the number of Langerhans’ cells
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(4):289-294
07-20-2004DOI 10.1590/S0100-72032004000400004
Views95OBJECTIVE: to study the relationship of biobehavioral factors, such as age, menarche, number of gestations, and age of first sexual intercourse, with changes in Langerhans'cells in women with negative hybrid capture for HPV. METHODS: thirty women referred due to abnormal cervical cytology or premalignant cervical lesions were studied and underwent colposcopy, guided biopsy and histopathological exams. The Langerhans' cells were identified by immunohistochemical (S100+) exams. Langerhans' cells visualized in brown color were counted using the software Cytoviewer. The nonparametric Wilcoxon rank-sum test was employed for statistical analysis. RESULTS: the number of Langerhans' cells in women who had menarche after 13 years old presented statistically significant difference (173.34 cell/mm²) compared to the group whose menarche occurred before 13 (271.41 cell/mm²). The age at the first sexual intercourse was associated with the low number of Langerhans' cells, 127.15 cell/mm² and 250.14 cell/mm², respectively, for the beginning of the sexual activity up to 17 years old and after 17 (p=0.03). Previous cauterizations of the uterine cervix have been related to a lower number of Langerhans' cells in the epithelium, with the average 120.30 cell/mm² as compared to 236.06 cell/mm² for those women who never underwent that procedure (p=0.05). Other factors such as the patient's age and the number of gestations showed no statistically significant differences in the density of Langerhans' cells. CONCLUSIONS: the present study reports the association of biobehavioral factors with decrease in the number of Langerhans' cell.
Key-words Celular immunizationCervical cauterizationsCervixHuman papillomavirusLangerhans' cellsSexual activitySee more


