Summary
Rev Bras Ginecol Obstet. 2023;45(3):149-159
This article aims to review the literature regarding the use of technologies to promote mental health for pregnant women. We seek to: understand the strategies that pregnant women use for mental health care. Also, we investigate the existence of scientific evidence that validates such practices.
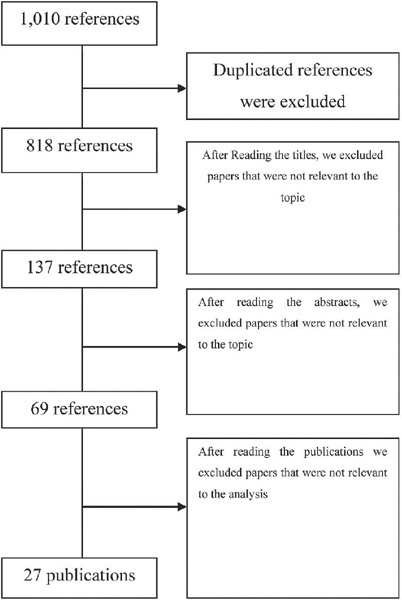
This study follows the PRISMA guidelines for systematic reviews. We analyze 27 studies published between 2012 and 2019. We include publications in Portuguese, English, and Spanish.
The results revealed several different possibilities to use technology, including the use of text messages and mobile applications on smartphones. Mobile applications are the most commonly used approaches (22.5%). Regarding the strategies used, cognitive-behavioral approaches, including mood checks, relaxation exercises, and psychoeducation comprised 44.12% of the content.
There is a need for further investigation and research and development efforts in this field to better understand the possibilities of intervention in mental health in the digital age.
Summary
Rev Bras Ginecol Obstet. 2022;44(9):845-853
To develop a protocol for hybrid low-risk prenatal care adapted to Brazilian guidelines, merging reduced face-to-face consultations and remote monitoring.
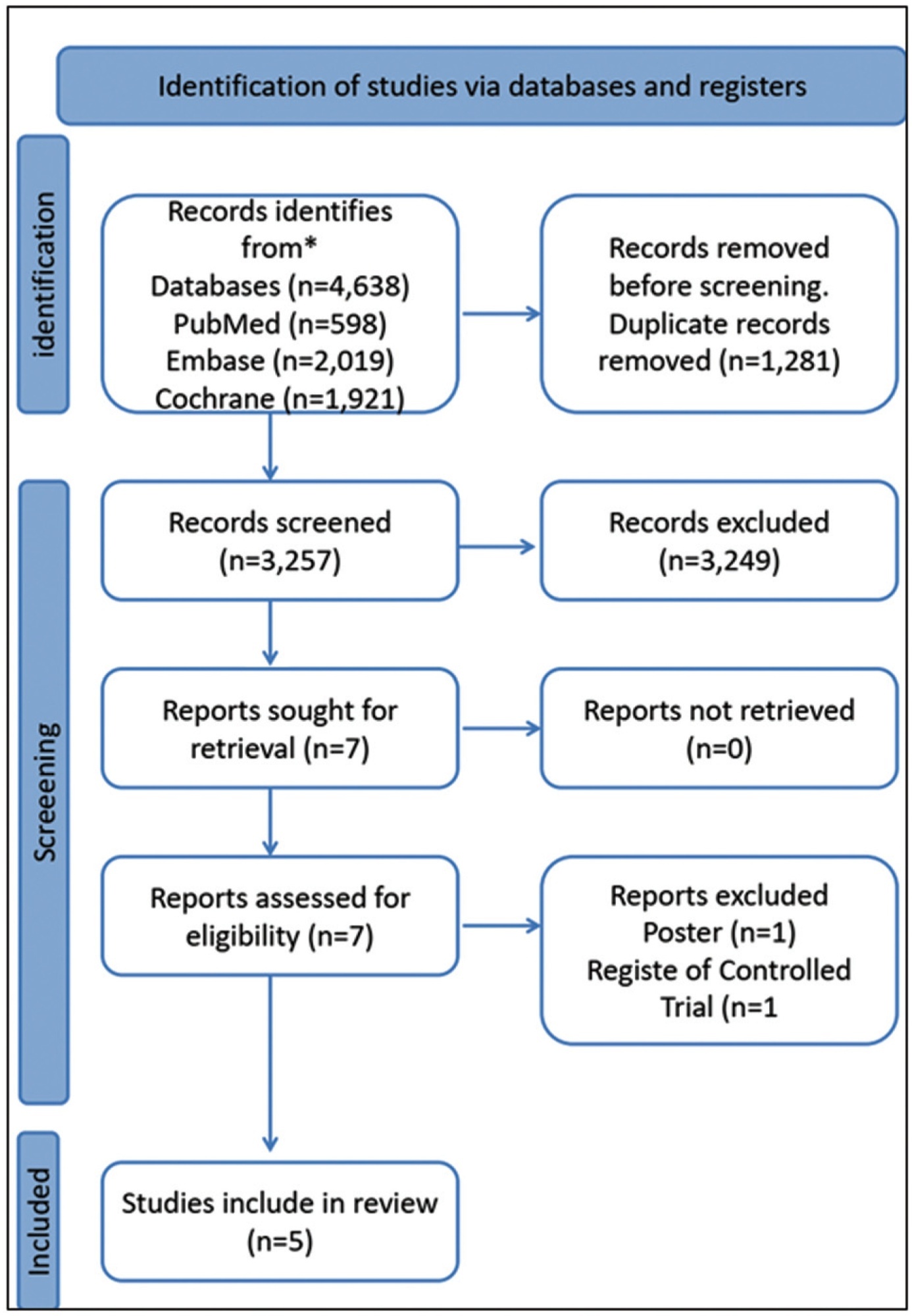
The PubMed, Embase, and Cochrane Library databases were systematically searched on telemedicine and antenatal care perspectives and adaptation of the low-risk prenatal care protocols recommended by the Ministry of Health and by the Brazilian Federation of Gynecology and Obstetrics Associations.
Five relevant articles and three manuals were included in the review, for presented criteria to develop this clinical guideline. We identified, in these studies, that the schedule of consultations is unevenly distributed among the gestational trimesters, and ranges from 7 to 14 appointments. In general, the authors propose one to two appointments in the first trimester, two to three appointments in the second trimester, and two to six appointments in the third trimester. Only three studies included puerperal evaluations. The routine exams recommended show minimal variations among authors. To date, there are no validated Brazilian protocols for prenatal care by telemedicine. The included studies showed that pregnant women were satisfied with this form of care, and the outcomes of interest, except for hypertensive diseases, were similar between the groups exposed to traditional and hybrid prenatal care.
The presented guideline comprises the Ministry of Health recommendations for low-risk prenatal care and reduces exposure to the hospital environment and care costs. A randomized clinical trial, to be developed by this group, will provide real-world data on safety, effectiveness, satisfaction, and costs.
Summary
Rev Bras Ginecol Obstet. 2022;44(5):452-457
To detect depression during pregnancy and in the immediate postpartum period using the Edinburgh postpartum depression scale (EPDS).
Cross sectional study of 315 women, aged between 14 and 44 years, who received perinatal care at the Leonor Mendes de Barros Hospital, in São Paulo, between July 1st, 2019 and October 30th, 2020. The cutoff point suggesting depression was ≥ 12.
The screening indicated 62 (19.7%) patients experiencing depression. Low family income, multiparity, fewer prenatal appointments, antecedents of emotional disorders, dissatisfaction with the pregnancy, poor relationship with the partner, and psychological aggression were all risk factors associated with depression in pregnancy or in the immediate postpartum period. Antecedents of depression and psychology aggression during pregnancy were significant variables for predicting perinatal depression in the multivariate analysis.
There is a significant association between the occurrence of perinatal depression and the aforementioned psychosocial factors. Screening patients with the EPDS during perinatal and postpartum care could facilitate establishing a line of care to improve the wellbeing of mother and infant.
Summary
Rev Bras Ginecol Obstet. 2022;44(4):398-408
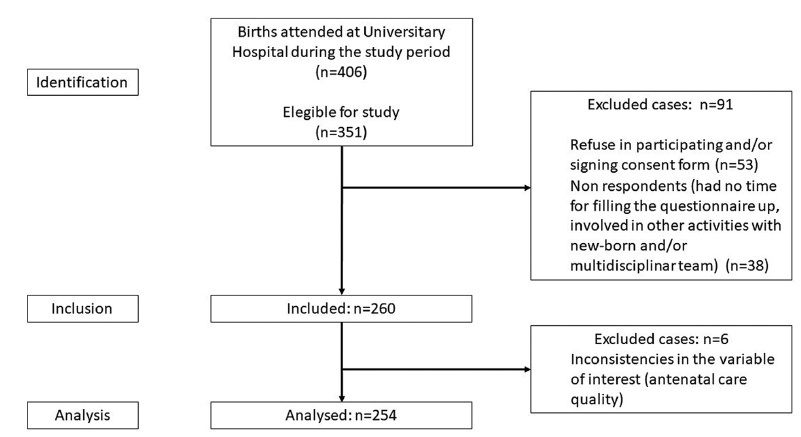
The present study aimed to evaluate the antenatal care adequacy for women who gave birth at the University Hospital of Santa Catarina in Florianopolis (Brazil) during the COVID-19 pandemic, and to evaluate the association of adequacy with sociodemographic, clinical, and access characteristics.
Data were collected between October and December 2020, including 254 patients who delivered in the University Hospital from Federal University of Santa Catarina and answered our questionnaires. Additional data were obtained from patients’ antenatal booklets. Antenatal care was classified as adequate, intermediate, or inadequate according to the number of appointments, gestational age at the beginning of follow-up, and tests results. We carried out a descriptive statistical analysis and a bivariate/with odds ratio analysis onmaternal sociodemographic, clinical and health access variables that were compared with antenatal adequacy.
Antenatal care was considered adequate in 35.8% of cases, intermediate in 46.8%, and inadequate in 17.4%. The followingmaternal variables were associated with inadequate prenatal care (intermediate or inadequate prenatal care): having black or brown skin colour, having two or more children, being of foreign nationality, not being fluent in Portuguese, and using illicit drugs during pregnancy; the clinical variables were more than 6 weeks between appointments, and not attending high-risk antenatal care; as for access, the variables were difficulties in attending or scheduling appointments, and attending virtual appointments only.
In a sample of pregnant women from a teaching hospital in Florianópolis during the COVID-19 pandemic, antenatal care was considered adequate in 35.8%, intermediate in 46.8%, and inadequate in 17.4% of cases.
Summary
Rev Bras Ginecol Obstet. 2022;44(3):220-230
To evaluate the effect of the carbohydrate counting method (CCM) on glycemic control,maternal, and perinatal outcomes of pregnant women with pregestational diabetes mellitus (DM).
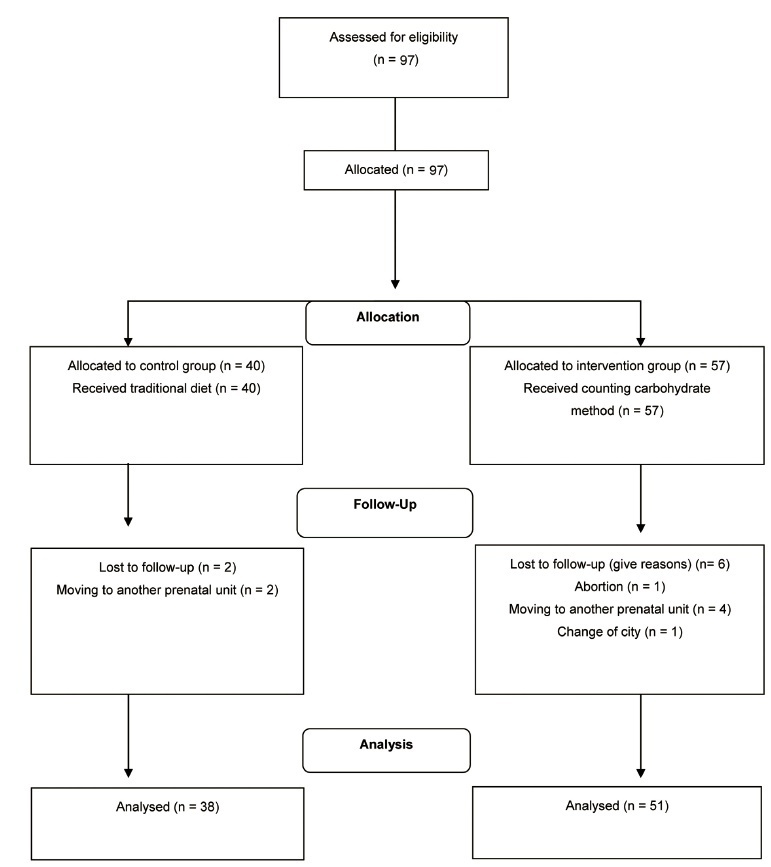
Nonrandomized controlled clinical trial performed with 89 pregnant women who had pregestational DMand received prenatal care in a public hospital in Rio de Janeiro, state of Rio de Janeiro, Brazil, between 2009 and 2014, subdivided into historic control group and intervention group, not simultaneous. The intervention group (n=51) received nutritional guidance from the carbohydrate counting method (CCM), and the historical control group (n=38), was guided by the traditionalmethod (TM). The Mann-Whitney test or the Wilcoxon test were used to compare intra- and intergroup outcomes andanalysis of variance (ANOVA) for repeated measures, corrected by the Bonferroni post-hoc test,was used to assess postprandial blood glucose.
Only the CCM group showed a reduction in fasting blood glucose. Postprandial blood glucose decreased in the 2nd (p=0.00) and 3rd (p=0.00) gestational trimester in the CCM group, while in the TM group the reduction occurred only in the 2nd trimester (p=0.015). For perinatal outcomes and hypertensive disorders of pregnancy, there were no differences between groups. Cesarean delivery was performed in 82% of the pregnant women and was associated with hypertensive disorders (gestational hypertension or pre-eclampsia; p=0.047).
Both methods of nutritional guidance contributed to the reduction of postprandial glycemia of women and no differences were observed for maternal and perinatal outcomes. However, CCM had a better effect on postprandial glycemia and only this method contributed to reducing fasting blood glucose throughout the intervention. ReBEC Clinical Trials Database The present study was registered in the ReBEC Clinical Trials Database (Registro Brasileiro de Ensaios Clínicos, number RBR-524z9n).
Summary
Rev Bras Ginecol Obstet. 2021;43(6):442-451
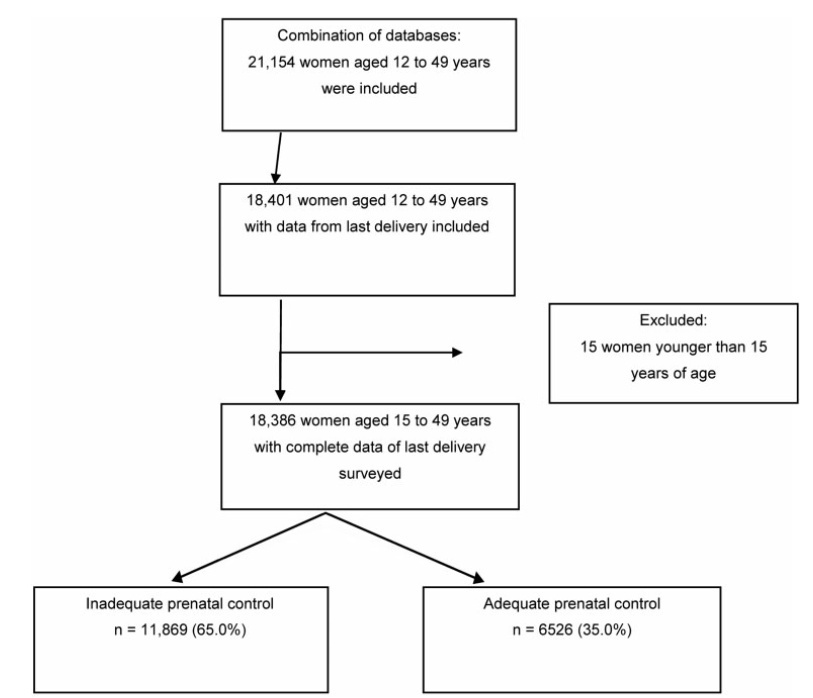
To determine the adequacy of compliance with antenatal care (ANC) by pregnant women in Peru and to identify the associated factors.
An analytical cross-sectional study of data from the 2019 Peruvian Demographic and Family Health Survey (Encuesta Demográfica y de Salud Familiar, ENDES, in Spanish) was conducted. The dependent variable was adequate compliance with ANC (provided by skilled health care professionals; first ANC visit during the first trimester of pregnancy; six or more ANC visits during pregnancy; ANC visits with appropriate content) by women aged 15 to 49 years in their last delivery within the five years prior to the survey. Crude and adjusted prevalence ratios and their 95% confidence intervals were calculated using a log-binomial regression model.
A total of 18,386 women were analyzed, 35.0% of whom adequately complied with ANC. The lowest proportion of compliance was found with the content of ANC (42.6%). Sociodemographic factors and those related to pregnancy, such as being in the age groups of 20 to 34 years and 35 to 49 years, havingsecondaryor higher education, belonging to a wealth quintile of the population other than the poorest, being from the Amazon region, not being of native ethnicity, having a second or third pregnancy, and having a desired pregnancy, increased the probability of presenting adequate compliance with ANC.
Only 3 out of 10women in Peru showed adequate compliancewith ANC. Compliance with the content of ANC must be improved, and strategies must be developed to increase the proportion of adequate compliance with ANC.
Summary
Rev Bras Ginecol Obstet. 2021;43(5):351-356
Most prenatal screening programs for toxoplasmosis use immunoassays in serum samples of pregnant women. Few studies assess the accuracy of screening tests in dried blood spots, which are of easy collection, storage, and transportation. The goals of the present study are to determine the performance and evaluate the agreement between an immunoassay of dried blood spots and a reference test in the serum of pregnant women from a population-based prenatal screening program for toxoplasmosis in Brazil.
A cross-sectional study was performed to compare the immunoassays Imunoscreen Toxoplasmose IgM and Imunoscreen Toxoplasmose IgG (Mbiolog Diagnósticos, Ltda., Contagem, Minas Gerais, Brazil)in dried blood spots with the enzymelinked fluorescent assay (ELFA, BioMérieux S.A., Lyon, France) reference standard in the serum of pregnant women from Minas Gerais Congenital Toxoplasmosis Control Program.
The dried blood spot test was able to discriminate positive and negative results of pregnant women when comparedwith the reference test, with an accuracy of 98.2% for immunoglobulin G (IgG), and of 95.8% for immunoglobulin M (IgM).
Dried blood samples are easy to collect, store, and transport, and they have a good performance,making this a promisingmethod for prenatal toxoplasmosis screening programs in countries with continental dimensions, limited resources, and a high prevalence of toxoplasmosis, as is the case of Brazil.
Summary
Rev Bras Ginecol Obstet. 2021;43(4):256-263
To investigate the association between prenatal care (PNC) adequacy indexes and the low birth weigth (LBW) outcome.
A total of 368,093 live term singleton births in the state of Rio de Janeiro (Brazil) from 2015 to 2016 were investigated using data from the Brazilian Live Birth Information System (Sistema de Informações sobre Nascidos Vivos, SINASC, in Portuguese). Seven PNC adequacy indexes were evaluated: four developed by Brazilian authors (Ciari Jr. et al., Coutinho et al., Takeda, and an index developed and used by the Brazilian Ministry of Health - MS) and three by authors from other countries (Kessner et al., the Adequacy of Prenatal Care Utilization index - APNCU, and the Graduated Prenatal Care Utilization Index - GINDEX). Adjusted odds ratios were estimated for the PNC adequacy indexes by means of multivariate logistic regression models using maternal, gestational and newborn characteristics as covariates.
When the PNC is classified as “inadequate”, the adjusted odds ratios to the LBWoutcome increase between 42% and 132%, depending on which adequacy index is evaluated. Younger (15 to 17 years old) and older (35 to 45 years old) mothers, those not married, of black or brown ethnicity, with low schooling (who did not finish Elementary School), primiparous, with preterm births, as well as female newborns had increasing odds for LBW. The models presented areas under the receiver operating characteristic (ROC) curve between 80.4% and 81.0%, and sensitivity and specificity that varied, respectively, between 57.7% and 58.6% and 94.3% and 94.5%.
Considering all PNC adequacy indexes evaluated, the APNCU had the best discriminatory power and the best ability to predict the LBW outcome.
Search
Search in:
breast (42) breast cancer (42) breast neoplasms (95) Cesarean section (72) endometriosis (66) infertility (56) Maternal mortality (43) menopause (82) obesity (58) postpartum period (40) pregnancy (225) Pregnancy complications (99) Prenatal care (68) prenatal diagnosis (50) Prevalence (41) Quality of life (51) risk factors (94) ultrasonography (79) urinary incontinence (40) women's health (48)