Summary
Rev Bras Ginecol Obstet. 2023;45(12):790-795
To compare cytological and histological results from women > 64 years old who followed the Brazilian national cervical cancer screening guidelines with those who did not.
The present observational retrospective study analyzed 207 abnormal cervical smear results from women > 64 years old in a mid-sized city in Brazil over 14 years. All results were reported according to the Bethesda System. The women were divided into those who followed the screening guidelines and those who did not.
Atypical squamous cells of undetermined significance and low-grade squamous intraepithelial lesion cytology results were found in 128 (62.2%) cases. Of these, 112 (87.5%) had repeated cytology with positive results. The other 79 (38.1%) with abnormal results should have been referred to colposcopy and biopsy. Out of 41 (51.9%) biopsied women, 23 (29.1%) had a confirmed diagnosis of neoplasia or precursor lesion. In contrast, among the 78 (37.7%) biopsied patients, 40 (51.3%) followed the guideline recommendations, with 9 (22.5%) positive biopsies. Of the 38 (48.7%) women who did not follow the guidelines, there were 24 (63.1%) positive results. Women who did not follow the guidelines demonstrated higher chances of cancer and precursor lesions (odds ratio [OR]: 5.904; 95% confidence interval [CI]: 2.188–15.932; p = 0.0002).
Women > 64 years old who did not follow the national screening protocol showed significant differences in the frequency of abnormal results and severity of diagnosis compared with those who followed the protocol.
Summary
Rev Bras Ginecol Obstet. 2023;45(11):724-728
To determine if the use of lubricating gel on the speculum during the cervicovaginal cytology examination interferes with the results obtained, as well as whether it reduces reported discomfort in patients.
A systematic review was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations, with a search in the Pubmed/Medline, Scielo, Cochrane Library, Embase databases of articles published between January 2011 and May 2022. The keywords used were cytology, speculum, lubricant, result, and pain.
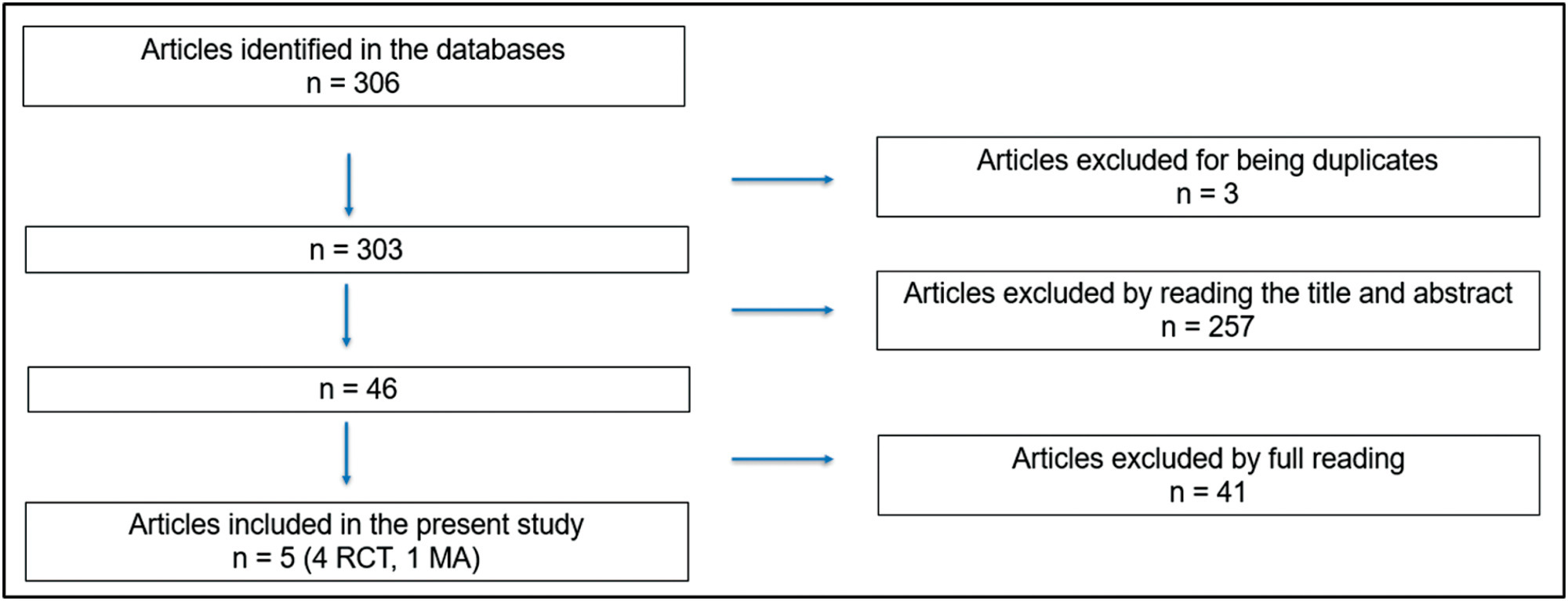
The initial search resulted in 306 articles, of which were excluded three because they were duplicates, 257 after reading the title and abstract and 41 after reading the full text. Thus, five articles were selected for the study: four randomized clinical trials and one metanalysis.
The selection of articles was performed by two investigators. The 5 selected articles were read in full and submitted to a comparative analysis.
Screening through cervicovaginal cytology allows for early diagnosis and reduction of associated mortality, but the procedure can be associated with pain. A small amount of aqueous lubricating gel in the speculum can be used to reduce the discomfort associated with performing cervicovaginal cytology.
The use of lubricating gel in the speculum does not seem to be associated with a change in the cytology result and reduces the discomfort associated with its insertion into the vagina.
Summary
Rev Bras Ginecol Obstet. 2023;45(5):235-241
To evaluate the accuracy and patient acceptability toward self-sampling using a new device - SelfCervix® - for detecting HPV-DNA.
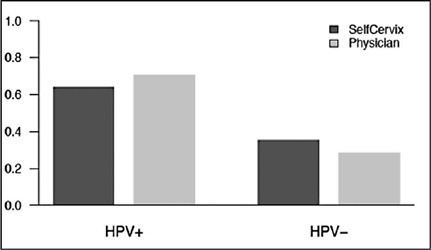
A total of 73 women aged 25–65 who underwent regular cervical cancer screening from March to October 2016 were included. Women performed self-sampling followed by a physician-sampling, and the samples were analyzed for HPV-DNA. After that, patients were surveyed about their acceptability of self-sampling.
HPV-DNA detection rate of self-sampling presented high accuracy and was similar to physician-collection. Sixty-four (87.7%) patients answered the acceptability survey. Most patients (89%) considered the self-sampling comfortable, and 82.5% preferred self-sampling to physician-sampling. The reasons cited were time-saving and convenience. Fifty-one (79.7%) reported that they would recommend self-sampling.
Self-sampling using the new Brazilian device SelfCervix® is not inferior in HPV-DNA detection rate compared with physician-collection, and patients are supportive of the method. Therefore, it might be an option to reach under-screened populations in Brazil.
Summary
Rev Bras Ginecol Obstet. 2022;44(5):483-488
To determine the prevalence of the atypical glandular cells (AGCs) cytology and to analyze its clinical significance in different age ranges.
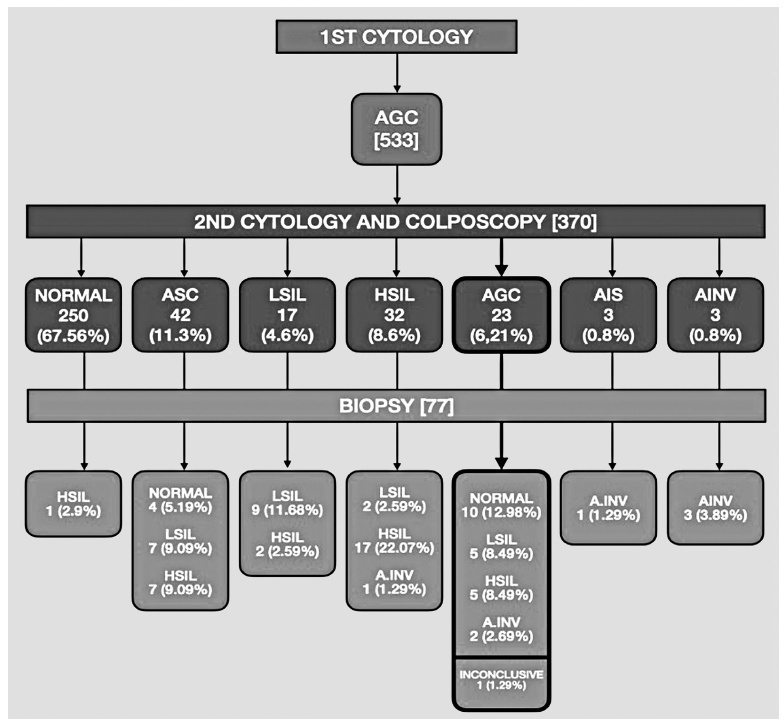
Retrospective observational study using computerized data from the Brazilian National Cancer Institute, including women screened between January 2002 and December 2008. The women included were those with an AGC result who were properly followed-up with colposcopy and a second cytology.
A total of 132,147 cytopathological exams were performed during the study period. Five-hundred and thirty-three (0.4%) women with AGC cytology were identified and, of these, 69.41% (370/533) were properly referred for colposcopy and a new cytology. Most of the women (79.2%) with a 1st or 2nd AGC cytology were between the ages of 25 and 54 years. The 2nd cytology demonstrated 67.6% (250/370) of normality, 24.5% (91/370) of squamous atypia, and 6.2% (23/370) of AGC, 0.8% (3/370) adenocarcinoma in situ and 0.8% (3/370) adenocarcinoma invasor. On biopsy of the women with a second AGC cytology, 43.4% (10/23) had normal histology, 43.4% (10/23) had squamous lesions, 8.7% (2/23) had invasive adenocarcinoma, and 1.2% (1/23) had an inconclusive report. All of the women with high-grade squamous intraepithelial lesion (HSIL) or invasive adenocarcinoma (respectively 5 and 2 patients), after a 2nd AGC cytology were 25 years old or older.
The prevalence of the AGC cytology was low in the studied population. Most of the AGC cytology cases occurred in adult women between the ages of 25 and 54. Although most of the patients had normal histology after follow-up, several of them presented with squamous intraepithelial lesions or invasive adenocarcinoma.
Summary
Rev Bras Ginecol Obstet. 2022;44(3):280-286
The purpose of this study was to compare the frequency of the occurrence of high-risk human papillomavirus (HPV) and abnormal anal cytology in immunocompetent women with and without HPV-induced genital lesions.
This analytical cross-sectional, observational study was conducted between July 2017 and December 2018 in a specialized outpatient clinic of a tertiary hospital in Fortaleza, CE. Fifty-seven immunocompetent women with and without genital intraepithelial lesions were assessed; they were divided into two groups: group 1 was comprised of women with HPV-associated genital lesions (n=26), and group 2 was comprised of those without HPV-associated genital lesions (n=31). Samples for liquidbased cytology and high-risk DNA-HPV polymerase chain reaction real-time tests were collected from the cervix and anus. All cases were evaluated using high-resolution anoscopy; biopsies were performed when required. The Fisher exact and chi-squared tests were applied for consolidated data in the contingency table, and the Student ttest and Mann-Whitney U-test for independent variables.
Anal high-risk HPV infections were more frequent in group 1 (odds ratio [OR], 4.95; 95% confidence interval [CI], 1.34-18.3; p=0.012), along with concomitant highrisk HPV infections in the uterine cervix and the anus (OR 18.8; 95% CI, 2.20-160; p<0.001). The incidence of high-risk cervical HPV infection was associated with highrisk anal HPV infection (OR, 4.95; 95% CI, 1.34-18.3; p=0.012). There was no statistical difference concerning abnormal anal cytology or anoscopy between the groups, and no anal intraepithelial lesion was found in either group.
Immunocompetent women with HPV-associated genital lesions and high-risk cervical HPV were more likely to have high-risk anal HPV.
Summary
Rev Bras Ginecol Obstet. 2018;40(6):360-368
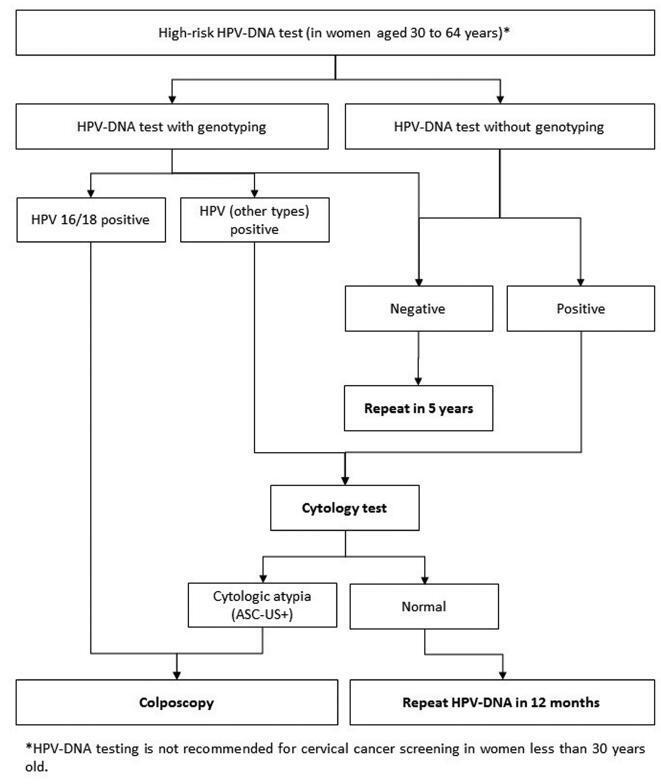
Evidence-based clinical guidelines ensure best practice protocols are available in health care. There is a widespread use of human papillomavirus deoxyribonucleic acid (HPVDNA) tests in Brazil, regardless of the lack of official guidelines. On behalf of the Brazilian Association for the Lower Genital Tract Pathology and Colposcopy (ABPTGIC, in the Portuguese acronym), a team of reviewers searched for published evidence and developed a set of recommendations for the use of HPV-DNA tests in cervical cancer screening in Brazil. The product of this process was debated and consensus was sought by the participants. One concern of the authors was the inclusion of these tests in the assessment of women with cytologic atypia and women treated for cervical intraepithelial neoplasia (CIN). Testing for HPV is recommended in an organized screening scenario to identify women with precursor lesions or asymptomatic cervical cancer older than 30 years of age, and it can be performed every 5 years. It also has value after the cytology showing atypical squamous cells of undetermined significance (ASC-US) or low-grade squamous intraepithelial lesions (LSILs) as a triage test for colposcopy, in the investigation of other cytological alterations when no abnormal findings are observed at colposcopy, seeking to exclude disease, or, further, after treatment of high-grade cervical intraepithelial neoplasia, to rule out residual disease.
Summary
Rev Bras Ginecol Obstet. 2017;39(2):80-85
To evaluate the association of age at first sexual intercourse with the results of the cervicovaginal cytology.
Observational analytical study about the prevalence of altered cervicovaginal cytology results in women aged between 18 and 34 years from a densely populated area in Brazil, during 10 years. The patients were stratified into 2 categories according to their age at first sexual intercourse (13-16 years and 17-24 years).
From the total of 2,505,154 exams, 898,921 tests were in accordance with the inclusion criteria. Considering women with 4 years or less from the first sexual intercourse as a reference, those with 5 to 9 years and 10 years or more showed a higher prevalence of high-grade squamous intraepithelial lesions (HSILs). Women with an earlier onset of sexual intercourse (13-16 years) showed higher prevalence ratios for atypical squamous cells (ASC), low-grade squamous intraepithelial lesion (LSIL) and HSIL. The prevalence ratio for HSIL adjusted by age at diagnosis and by age at first sexual intercourse was higher only for women with an earlier onset of sexual intercourse.
The age of first sexual intercourse could be a variable that might qualify the selection among young women who are really at a higher risk for HSIL.
Summary
Rev Bras Ginecol Obstet. 2008;30(11):573-582
DOI 10.1590/S0100-72032008001100008
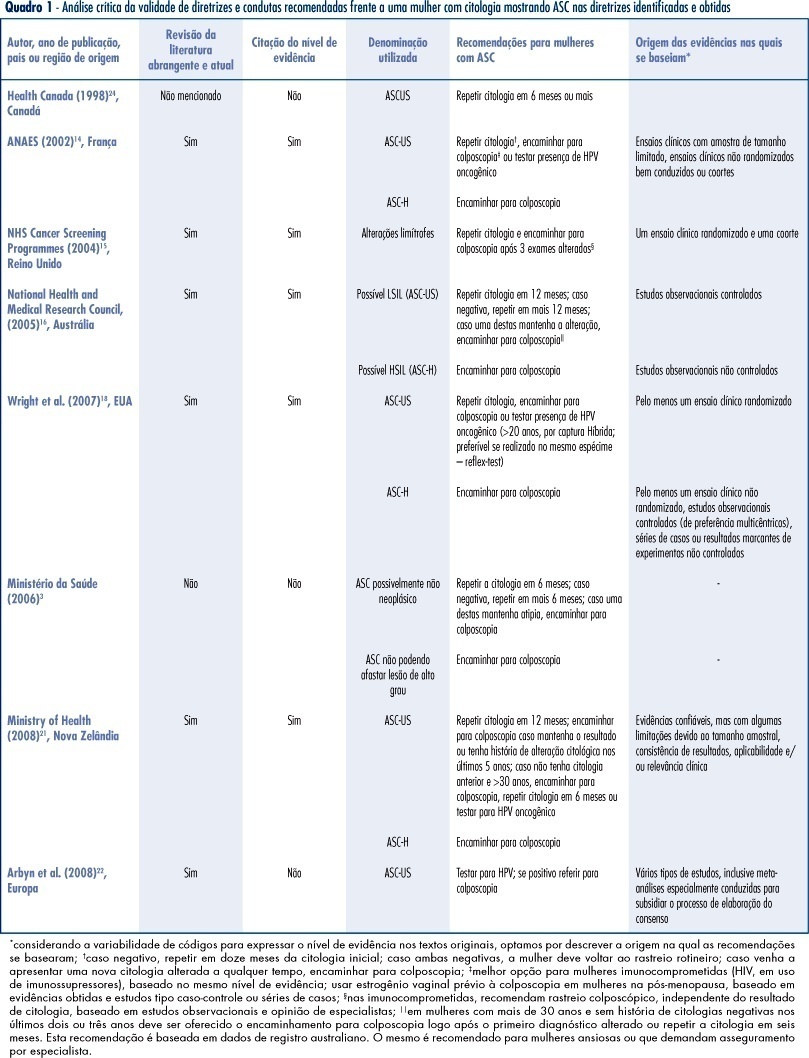
PURPOSE: to identify valid guidelines for the approach of women with cytopathological diagnosis of undetermined significance atypias in squamous cells (ASC), discussing its applicability to the Brazilian scenario. METHODS: an electronic search of publications at PubMed, National Guidelines Clearinghouse and Scholar Google was carried out, as well as a manual search of references from the texts found. The guidelines identified, and specifically related to the theme, were evaluated according to its validity and the recommendations were criticized and summarized. RESULTS: guidelines for the United Kingdom, France, Australia, the USA and New Zealand have been considered as valid. These documents recommend repeating the cytology in six or twelve months, in ASCs of undetermined significance (ASC-US) before referring to colposcopy, and immediate referral to colposcopy in ASCs, when it is not possible to disregard high degree lesions (ASC-H). We have also found valid colposcopy recommendations for women with ASC-US in special situations (immune deficient women requiring specialist assistance) and the use of oncogenic HPV test, which, when present in women over 20, should motivate referral to colposcopy. CONCLUSIONS: the clinical guidelines recommended for the Programa Nacional de Controle do Cancer do Colo do Útero in Brazil can be improved with the referral to colposcopy in special situations (immune deficient women requiring specialist assistance), the use of test for the detection of oncogenic HPV in women over 20 (when present, refer to colposcopy), the investigation of vaginal lesions, the use of estrogens before the colposcopy in post-menopausal women, and disregard biopsia in case of slighter alterations.
Search
Search in:
breast (42) breast cancer (42) breast neoplasms (95) Cesarean section (72) endometriosis (66) infertility (56) Maternal mortality (43) menopause (82) obesity (58) postpartum period (40) pregnancy (225) Pregnancy complications (99) Prenatal care (68) prenatal diagnosis (50) Prevalence (41) Quality of life (51) risk factors (94) ultrasonography (79) urinary incontinence (40) women's health (48)