Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(1):24-31
DOI 10.1590/S0100-72032006000100005
PURPOSE: to verify the coverage and factors associated with Papanicolaou (Pap) testing in Londrina (PR), Brazil. METHODS: this is a cross-sectional study, carried out in 2004, in microareas of five Basic Health Units (BHU) of Londrina. One or two microareas from each BHU were selected and a list of all women aged 20-59 years resident in these places, was made through search in the Basic Attention Information System, the women being then visited and interviewed. Those with a Pap test in the last three years were considered as having an updated examination, and the remaining as delayed. The association of some factors with the examination situation was investigated. Data analysis was performed using Epi-Info 6.04d. RESULTS: Pap smear coverage among the 513 participants of the study was 80.7%, ranging from 71.5% to 88.4%. Delay in taking the test was higher (p<0.05) among women who worked only at home (22.4% as compared with 14.3% among those who worked outside), and among those who belonged to D/E social classes (24.9%) as compared to C (17.5%) and A/B (8.3%) classes. The proportion who ignored the next test date was higher (p<0.01) among those who had the last Papanicolaou testing at a BHU (14.7%), as compared to those who had been attended privately or by a health insurance company (5.8%). CONCLUSION: the coverage of Pap smear in the studied areas can be considered satisfactory, although there is a need of improving compliance with Pap test, mainly among women who are the poorest and who work only at home.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):619-626
DOI 10.1590/S0100-72032005001000009
PURPOSE: to evaluate the prevalence of cytologic, colposcopic and histopathologic alterations observed in the uterine cervix of adolescents with suspected cervical neoplasia and to compare it with young adult women. METHODS: a cross-sectional, retrospective study that analyzed 366 medical records of females referred to clarify diagnosis of the suspected cervical neoplasia. The patients had been classified into two groups defined by age. The Adolescent group was composed of 129 females between 13 and 19 years and the Adult group was composed of 237 females between 20 and 24 years. Data were analyzed statistically by the prevalence ratio (PR), respective confidence intervals (CI) at 95% for each variable, chi2 test, or Fisher exact test used to compare proportion. RESULTS: the first sexual intercourse coitarche occurred on average at 15.0 years in the Adolescent group and 16.6 years in the Adult group. The possibility of diagnosis of cytological alterations in the first Papanicolaou smears (PR=2.61; CI 95%: 2.0-3,4), the condition of non-clarified cervical intraepithelial neoplasia (CIN) (PR=1.78; CI 95%: 1.26-2,52), and the colposcopic impressions of low grade (PR=1.42; CI 95%: 1.08-1.86) were statistically significant in the Adolescent group. The histopathologic analysis did not show differences at any grade of CIN. However, two cases of microinvasive carcinoma, one in each group, and three cases of clinical invasive carcinoma in the Adult group were identified. CONCLUSION: our study suggests that cervical cancer is rare among adolescents, but we verified that alterations associated with it occurred even in younger women. The evaluation of cervical intraepithelial neoplasia with the careful application of the same tools used for adult women was appropriate also in adolescence.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(3):129-134
DOI 10.1590/S0100-72032000000300002
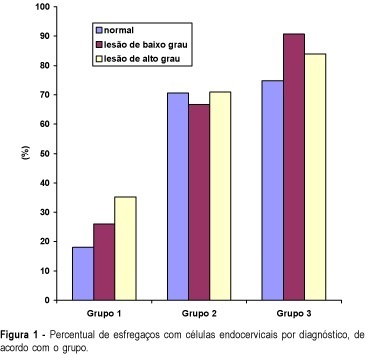
Purpose: to compare the performance of cervical canal and vaginal cul-de-sac samples for colpocytology testing, in order to diagnose cervical neoplasia. Methods: three sequential groups were constituted: group 1 - 10,048 women with ectocervix and cul-de-sac samples collected with the use of an Ayre spatula; group 2 - 3,847 women with ectocervix, cul-de-sac and cervical canal samples taken with an Ayre spatula and a cytobrush, and group 3 -- 4,059 women with ectocervix and cervical canal samples, using an Ayre spatula and a cytobrush. ANOVA (analysis of variance) and comparison of proportions were utilized for the statistical analysis. Results: the rates of abnormal tests in groups 2 (2.6%) and 3 (2.4%), including all squamous and glandular lesions, were significantly higher than in group 1 (2.0%). The diagnosis rates of low-grade squamous intraepithelial lesion (LGSIL) were not statistically different between the three groups (1.27, 1.25 and 1.07%). On the other hand, the diagnosis rates of high-grade squamous intraepithelial lesion (HGSIL) were statistically higher in groups 2 (0.81%) and 3 (0.77%) than in group 1 (0.54%). The difference between the rates of the second and the third groups did not present any statistical significance. Conclusions: the cervical canal sampling improves the performance of cytologic testing for the diagnosis of HGSIL, while cul-de-sac sampling does not change significantly the performance in diagnosing cervical neoplasia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(5):248-256
DOI 10.1590/S0100-72032005000500004
PURPOSE: to estimate the prevalence of HPV and its genotypes in HIV-infected and non-infected women, using the Polymerase Chain Reaction (PCR) technique. METHODS: a sectional study with 79 enrolled women: a study group, with 41 HIV-infected women, and a control group, with 38 non-infected women attended at a Basic Health Unit. All were submitted to a serologic test for the detection of HIV and spontaneously looked for gynecological attendance at those units, for the first time. They answered a standard questionnaire and were submitted to a gynecological examination with a cervical swab and specimen for the detection of DNA-HPV and its genotypes. Statistical analysis was performed using Kruskal-Wallis, chi2 or Fisher's exact tests. Statistical significance was considered at p<0.05. RESULTS: the demographic characteristics, obstetric and gynecological previous history were similar in both groups except for previous STD, but different as to the gynecological examination and cervical cytological analysis. The presence of DNA-HPV was significantly different (p<0.05) in the two groups. Among HIV-infected patients, 73.2% presented DNA-HPV positive results, as compared with 23.8% of non-infected women (OR=8.79; 95% IC: 2.83 28.37). Concerning HPV genotypes, there was no clear predominance of a specific HPV subtype in the HIV-infected or in the HIV non-infected groups, and the frequency of unidentified types was similar in both groups. Non-significant predominance of HPV multiple infections (p>0.05) was detected in the HIV-infected women (50.0%) and the most frequently found combination was of types 6, 11 and 16. HPV simple infection occurred in 66.6% of HIV-non-infected patients. The most frequent type found in both groups was 16, representing 44% of all the simple infections in both groups. CONCLUSIONS: HIV-infected women showed higher DNA-HPV prevalence in the uterine cervix, as compared to non-infected women. There was no difference in the predominance of specific types of HPV when both groups were compared. There was a tendency to HPV multiple infections in the HIV-infected women, whereas simple infection predominated in the non-infected patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(2):51-57
DOI 10.1590/S0100-72032005000200002
PURPOSE: to estimate the validity of visual inspection of cervical intraepithelial neoplasia (CIN) and HPV-induced lesion screening, after acetic acid application (VIA), and to compare its performance with that of colpocytology and colposcopy. METHODS: a diagnostic test validation study involving 893 women aged 18 to 65 years, simultaneously screened with colpocytology, VIA and colposcopy was carried out at a public health unit in Recife, PE. VIA was performed by applying 5% acetic acid onto the cervix and observing it with the help of a clinical spotlight. The finding of any aceto-white lesion on the cervix was considered positive. The gold standard was the histopathology of cervical biopsy, carried out whenever any of the three test results was abnormal. Validity indicators were estimated for each test, within 95% confidence intervals. The analysis of agreement between test results was done by the kappa coefficient. RESULTS: of 303 women submitted to biopsy, the histopathological study was abnormal in 24. Among this total, VIA was positive in 22, yielding an estimated 91.7% sensibility, 68.9% specificity, and 7.5% positive predictive value and 99.7% negative predictive value. Comparing 95% confidence intervals, VIA was more sensitive than colpocytology, despite a lower specificity and positive predictive value. There was poor agreement between VIA and colpocytology (k=0.02) and excellent agreement with colposcopy (k=0.93). CONCLUSION: VIA was much more sensitive than colpocytology in the screening of CIN and HPV-induced lesions and presented a performance similar to colposcopy. Its low specificity determined a high number of false-positive results.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(6):457-462
DOI 10.1590/S0100-72032004000600006
OBJECTIVE: to assess the ability of Pap smear and hybrid capture II (HCII) to detect clinically significant cervical lesions (CIN2/3) in women referred to hospital due to atypical squamous cells of unknown significance (ASCUS) or low-grade squamous intraepithelial lesions (LSIL). METHODS: a cross-sectional study comprising 161 women referred to the Taubaté University Hospital due to ASCUS/LSIL, between August 2000 and September 2002. All women responded to a questionnaire regarding sociodemographic and reproductive characteristics and were subjected to gynecological examination with specimen collection for Pap test and HCII, along with colposcopy and eventual cervical biopsy. The relationship between HCII results and age, use of condom, oral hormonal contraception, and smoking were evaluated by the chi-square test. The sensitivity, specificity, positive and negative predictive values of both Pap test and HCII were calculated. All calculations were performed within 95% confidence intervals. RESULTS: sixty-seven percent of the women that tested positive for HPV were less than 30 years old. Pap smear and HCII showed the same 82% sensitivity in detecting CIN2/3 when the threshold for a positive Pap result was ASCUS, LSIL or HSIL. Pap smear specificity and positive predictive values were substantially increased when only HSIL results were considered as positive (from 29 to 95% and 12 to 50%, respectively). These figures were superior to those of HCII, but at the expense of an expressive loss of sensitivity (from 82% to 41%). CONCLUSIONS: our results substantiate the potential of HCII in detecting CIN2/3 among women referred due to ASCUS/LSIL.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(4):269-275
DOI 10.1590/S0100-72032004000400002
OBJECTIVE: to evaluate the performance of Pap smear, hybrid capture II (HC II), and visual inspection with acetic acid in the detection of pre-invasive and invasive cervical lesions. METHODS: a total of 2281 women were submitted to a clinical exam, including Pap smear, HC II for HPV DNA detection and visual inspection with 5% acetic acid (VIA). When at least one of the tests was positive, colposcopy was performed and targeted biopsies were taken from suspicious lesions. Colposcopy was also performed in 420 women with negative results. Test performance was evaluated, using colposcopy as the gold standard, with or without biopsy. RESULTS: Pap smear, VIA and HC II were positive in 9.2, 10.9 and 17.5% of all women screened, respectively. Although at least one positive test was found in 671 women (29.4%), only 82 (3.6%) presented histologically confirmed disease (50 NIC1, 20 NIC2, 7 NIC3, and 5 invasive carcinoma). VIA and HC II sensitivities were similar and significantly higher than Pap smear. Pap smear showed better specificity than VIA and than HC II. In women with a negative Pap smear result, VIA showed better performance than HC II. CONCLUSION: Pap smear combined with VIA performed better than Pap smear combined with HC II or than Pap smear alone.