Summary
Rev Bras Ginecol Obstet. 2023;45(12):818-823
Cervical cancer (CC) is caused by persistent infection of human papillomavirus of high oncogenic risk (hr-HPV); however, several cofactors are important in its carcinogenesis, such as smoking, multiparity, and prolonged use of oral hormonal contraceptives (COCs). Worldwide, 16% of women use COCs, whereas in Brazil this rate is of ~ 30%. The safety and adverse effects of COCs are widely discussed in the literature, including the increase in carcinogenic risk. Due to the existence of several drugs, combinations, and dosages of COCs, it is hard to have uniform information in epidemiological studies. Our objective was to perform a narrative review on the role of COCs use in the carcinogenesis of cervical cancer. Several populational studies have suggested an increase in the incidence of cervical cancer for those who have used COCs for > 5 years, but other available studies reach controversial and contradictory results regarding the action of COCs in the development of CC.
Summary
Rev Bras Ginecol Obstet. 2023;45(8):474-479
Similar to Human Papillomavirus (HPV) genotypes, different lineages of a genotype also have different carcinogenic capabilities. Studies have shown that specific genotype lineages of oncogenic HPV are associated with variable risks for the development of cervical intraepithelial neoplasia (CIN2/CIN3) and cervical cancer. The present study aimed to analyze the genetic diversity of the HPV16 genotype in women with CIN2/CIN3 and cervical cancer, from the northeast region of Brazil.
A cross-sectional multicenter study was conducted in the northeast region of Brazil, from 2014 to 2016. This study included 196 cases of HPV16 variants (59 and 137 cases of CIN2/CIN3 and cervical cancer, respectively). The difference of proportion test was used to compare patients with CIN2/CIN3 and cervical cancer, based on the prevalent HPV16 lineage (p < 0.05).
According to the histopathological diagnosis, the percentage of lineage frequencies revealed a marginal difference in the prevalence of lineage A in CIN2/CIN3, compared with that in cervical cancer (p = 0.053). For lineage D, the proportion was higher in cancer cases (32.8%), than in CIN2/CIN3 cases (16.9%), with p = 0.023.
HPV16 lineage A was the most frequent lineage in both CIN2/CIN3 and cervical cancer samples, while lineage D was predominant in cervical cancer, suggesting a possible association between HPV16 lineage D and cervical cancer.
Summary
Rev Bras Ginecol Obstet. 2023;45(1):21-30
To evaluate the rates of precancerous lesions, colposcopy referral, and positive predictive value (PPV) by age groups of a population-based screening with DNA-HPV testing.
The present demonstration study compared 16,384 HPV tests performed in the first 30 months of the program with 19,992 women tested in the cytology screening. The colposcopy referral rate and PPV for CIN2+ and CIN3+ by age group and screening program were compared. The statistical analysis used the chi-squared test and odds ratio (OR) with 95% confidence interval (95%CI).
The HPV tests were 3.26% positive for HPV16-HPV18 and 9.92% positive for 12 other HPVs with a 3.7 times higher colposcopy referral rate than the cytology program, which had 1.68% abnormalities. Human Papillomavirus testing detected 103 CIN2, 89 CIN3, and one AIS, compared with 24 CIN2 and 54 CIN3 detected by cytology (p < 0.0001). The age group between 25 and 29 years old screened by HPV testing had 2.4 to 3.0 times more positivity, 13.0% colposcopy referral, twice more than women aged 30 to 39 years old (7.7%; p < 0.0001), and detected 20 CIN3 and 3 early-stage cancer versus 9 CIN3 and no cancer by cytology screening (CIN3 OR= 2.10; 95%CI: 0.91 -5.25; p = 0.043). The PPV of colposcopy for CIN2+ ranged from 29.5 to 41.0% in the HPV testing program.
There was a significant increase in detections of cervix precancerous lesions in a short period of screening with HPV testing. In women < 30 years old, the HPV testing exhibited more positivity, high colposcopy referral rate, similar colposcopy PPV to older women, and more detection of HSIL and early-stage cervical cancer.
Summary
Rev Bras Ginecol Obstet. 2022;44(3):272-279
To evaluate whether colposcopy-directed biopsy is necessary to increase the accuracy of diagnosing cervical intraepithelial lesions in relation to colposcopy.
We performed a retrospective, observational study by analyzing medical records obtained fromHospital de Clínicas do Paraná fromFebruary 2008 to February 2018. Patients with results of Pap tests, colposcopy, colposcopy-directed biopsy, and surgical procedures (high-frequency surgery or cold conization) were included. Data such as quadrants involved during colposcopy and age differences were also analyzed.
A total of 299 women were included. Colposcopy was found to have an accuracy rate of 76.25% (95% confidence interval [CI], 71.4-81.1). Among the highest-grade lesions, the accuracy rate was 80.5% (95% CI, 75.7-85.3). The accuracy rates for biopsy were 79.6% (95% CI, 75-84.2) and 84.6% (95% CI, 80-89.1) for the highest-grade lesions. High-grade lesions were accurately confirmed in 76.9% and 85% of patients with 1 and 2 or more affected quadrants, respectively. For women younger than 40 years, the accuracy rates were 77.6% and 80.8% for colposcopy and biopsy, respectively. For women 40 years or older, the accuracy rates were 72.5% and 76.3% for colposcopy and biopsy, respectively.
There is no difference between the accuracy of colposcopy and that of biopsy in diagnosing cervical intraepithelial lesions in relation with the result of conization. The patients who received the greatest benefit when biopsy was not performed were those with high-grade lesions at colposcopy, a lesion involving 2 or more quadrants, and those younger than 40 years.
Summary
Rev Bras Ginecol Obstet. 2022;44(2):178-186
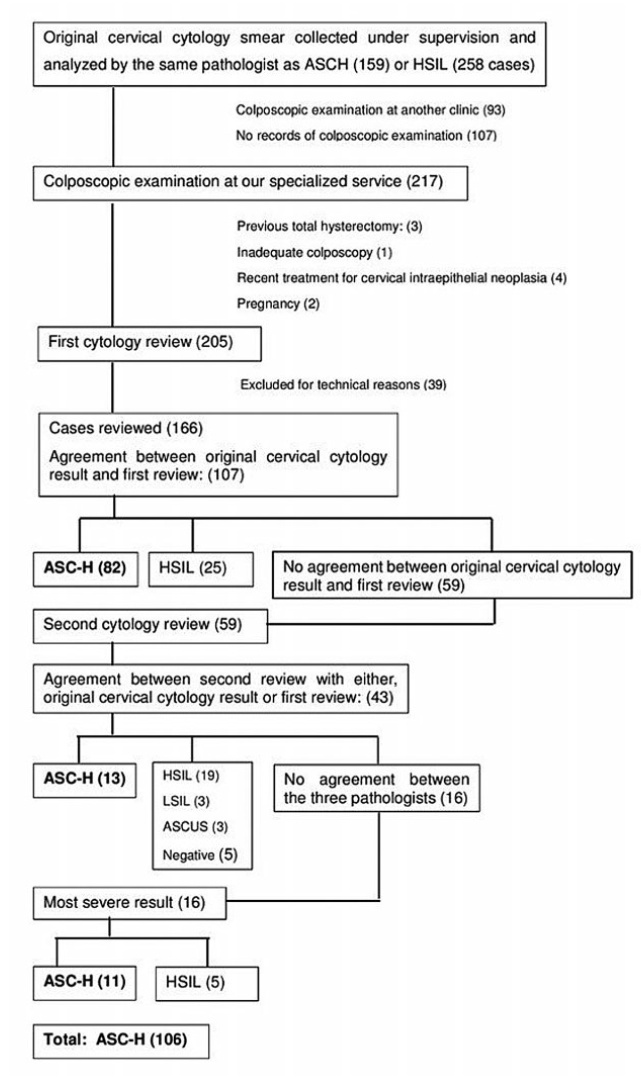
To determine the accuracy of colposcopy findings in diagnosing cervical intraepithelial neoplasia (CIN) in women with an atypical squamous cells, cannot exclude high-grade squamous intraepithelial lesion (ASC-H) pap smear result and analyze whether the prevalence of HSIL and cancer correlates with sociodemographic risk factors and specific colposcopic findings.
Colposcopic findings and sociodemographic risk factors were analyzed as possible predictors of a CIN 2 or worse diagnosis in women with an ASC-H pap smear result.
Accuracy of the colposcopic impression was 92%, sensitivity was 91.6%, and specificity was 93.1%, with a positive predictive value of 96.4% and negative predictive value of 84.3%. Diagnosis of CIN 2 or worse was more frequent in patients with a previous history of cervical dysplasia and pre-menopausal patients. Identification of major colposcopic findings, dense acetowhite epithelium, coarse mosaicism, and punctuation correlated significantly with CIN 2 or worse.
Colposcopy performed by an experienced examiner can accurately differentiate patients with CIN 1 or less from patients with CIN 2 or worse. Diagnosis of CIN 2 or worse was more frequent in patients with a previous history of cervical dysplasia and pre-menopausal patients. The degree of acetowhite changes was the best colposcopic feature to predict CIN2 or worse.
Summary
Rev Bras Ginecol Obstet. 2020;42(6):340-348
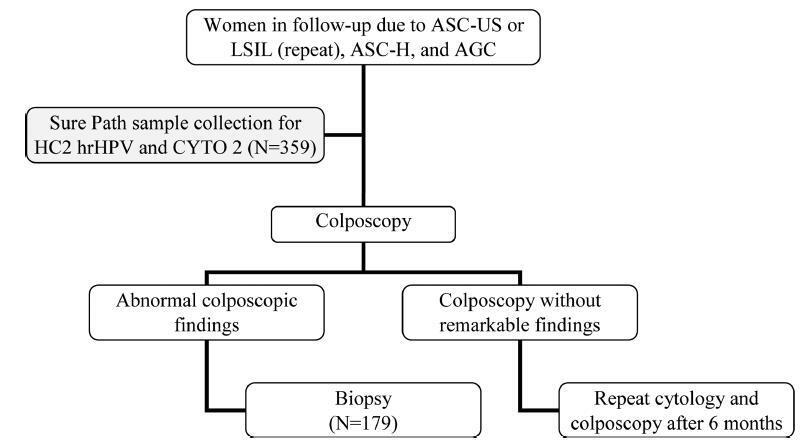
To evaluate the performance of the hybrid capture 2 (HC2) high-risk papillomavirus (hrHPV) assay and cytological test in women with previous abnormalities, to detect cervical intraepithelial neoplasia grade 2 or worse (≥ CIN 2).
A cytological test and HC2 (Qiagen, Gaithersburg, Maryland, EUA) for hrHPV were conducted in 359 liquid-based (Sure Path, Becton Dickinson, TriPath Imaging, Burlington, NC, USA) samples collected from women from the Vale do Ribeira Region, during July 2013 and September 2015 with previous cytology classified as atypical squamous cells of undetermined significance (ASC-US), low-grade squamous intraepithelial lesion (LSIL), atypical squamous cells, cannot exclude high-grade squamous intraepithelial lesions (ASC-H), and atypical glandular cells (AGC). The histopathological examination was conducted in 179 women. The performance evaluations were calculated using the “exact” Clopper-Pearson 95% confidence interval (CI) test by MEDCALC (Medcalc Software Ltd, Ostend, Belgium).
The ≥ CIN 2 frequency was 11.7% (21/179). The HC2 for hrHPV and repeat cytology to detect ≥ CIN 2 obtained, respectively, a sensitivity of 90.5% (95% CI = 69.6-98.8) and 90.5%, (95%CI = 69.6-98.8), a specificity of 65.8% (95% CI = 57.9-73.2) and 43.7% (95%CI = 35.8-51.8), a positive predictive value of 26.0% (95% CI = 21.4-31.3) and 17.6%, (95%CI = 14.9-20.6), and a negative predictive value of 98.1% (95%CI = 93.3-99.5) and 97.2% (95% CI = 90.1-99.2).
Hybrid capture 2 for hrHPV improves the performance of the detection of ≥ CIN 2, without compromising sensitivity, and provides a greater safety margin to return to the triennial screening of women undergoing follow-up due to previous abnormalities, without underlying ≥ CIN 2.
Summary
Rev Bras Ginecol Obstet. 2019;41(6):387-393
Themain objective of the present study was to estimate the annual treatment costs of invasive cervical cancer (ICC) per patient at an oncology center in Brazil from a societal perspective by considering direct medical, direct nonmedical, and indirect costs.
A cost analysis descriptive study, in which direct medical, direct nonmedical, and indirect costs were collected using a microcosting approach, was conducted between May 2014 and July 2016 from a societal perspective. The study population consisted of women diagnosed with ICC admitted to a tertiary hospital in Recife, state of Pernambuco, Brazil. The annual cost per patient was estimated in terms of the value of American Dollars (US$) in 2016.
From a societal perspective, the annual ICC treatment cost per patient was US $ 2,219.73. Direct medical costs were responsible for 81.2% of the total value, of which radiotherapy and outpatient chemotherapy had the largest share. Under the base-case assumption, the estimated cost to the national budget of a year of ICC treatment in the Brazilian population was US$ 25,954,195.04.
We found a high economic impact of health care systems treating ICC in a poor region of Brazil. These estimates could be applicable to further evaluations of the cost-effectiveness of preventing and treating ICC.
Summary
Rev Bras Ginecol Obstet. 2019;41(4):249-255
The present study aimed to examine which development indicators are correlated with cervical cancer (CC) mortality rates in Brazil.
This was an ecological study that correlatedmortality rates and indicators, such as human development index (HDI), gross domestic product (GDP) per capita, illiteracy rate, fertility rate, screening coverage, proportion of private health insurance use, density of physicians, and density of radiotherapy centers. Themortality rateswere obtained fromthe Brazilian national registry, while the indicators were based on official reports from the Ministry of Health. Univariate and multivariate linear regression was used.
Among the states of Brazil, the average age-specific CC mortality rate from 2008 to 2012 varied from 4.6 to 22.9 per 100,000 women/year. In the univariate analysis, HDI, proportion of private health insurance use, density of physicians, and density of radiotherapy centers were inversely correlated with the mortality rates. Fertility rate was positively correlated with the mortality rates. In the multivariate analysis, only fertility rate was significantly associated with the CC mortality rate (coefficient of correlation: 9.38; 95% confidence interval [CI]: 5.16-13.59).
A decrease in the fertility rate, as expected when the level of development of the regions increases, is related to a decrease in the mortality rate of CC. The results of the present study can help to better monitor the quality assessment of CC programs both among and within countries.
Search
Search in:
breast (42) breast cancer (42) breast neoplasms (95) Cesarean section (72) endometriosis (66) infertility (56) Maternal mortality (43) menopause (82) obesity (58) postpartum period (40) pregnancy (225) Pregnancy complications (99) Prenatal care (68) prenatal diagnosis (50) Prevalence (41) Quality of life (51) risk factors (94) ultrasonography (79) urinary incontinence (40) women's health (48)