Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo18
Despite the literature on dydrogesterone, studies on dydrogesterone utilization patterns are largely lacking in Indian patients.
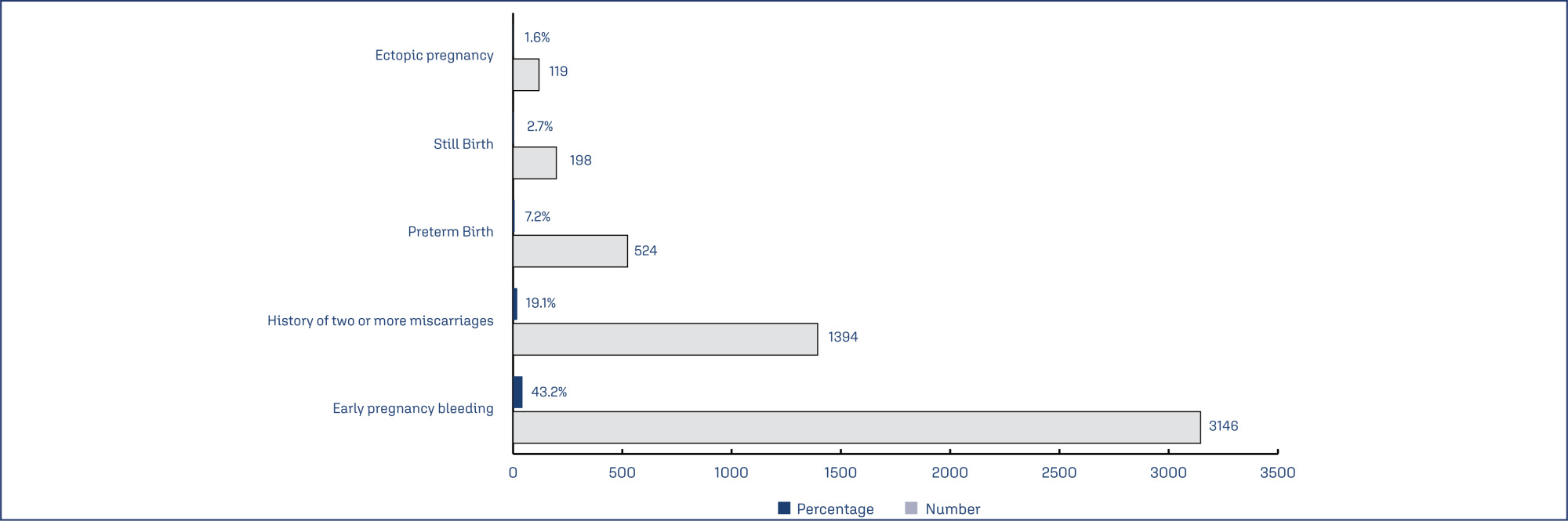
This was a multi-center, retrospective, observational, cross-sectional, and descriptive study across 817 centers in India. Data of patients who received dydrogesterone in past and provided consent for future use of their medical record for research purpose was were retrieved and analyzed.
Data of 7287 subjects (aged 29.55±4.84 years) was analyzed. Threatened abortion was the most common indication for which the subjects received dydrogesterone (46.9%) followed by recurrent pregnancy loss. Polycystic ovary syndrome (PCOS), thyroid disorders and anemia were the most common comorbid conditions and prior pregnancy loss, advanced maternal age and obesity were the most common risk factors seen in subjects who received dydrogesterone. Total 27.5% of subjects received a loading dose of dydrogesterone, and majority (64%) received 40 mg as loading dose. 10 mg dose was used as maintenance or regular dose in 81.4% of the subjects. Twice daily (BID) was the most common dosing frequency (66.6%). The most common concomitant medications being taken by the subjects on dydrogesterone included folic acid (45.1%), iron supplements (30.3%) and calcium and vitamin D3 supplements (25.5%). Another progesterone preparation (oral, injection, vaginal, tubal) other than dydrogesterone was used concurrently in 7.8% of subjects.
The study helped to identify the patient population that is benefitted by dydrogesterone and the preferred indications, risk factors, comorbid conditions and concomitant medication used in this patient population at real-life scenario.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo19
To examine whether the DDAH2 promoter polymorphisms -1415G/A (rs2272592), -1151A/C (rs805304) and -449G/C (rs805305), and their haplotypes, are associated with PE compared with normotensive pregnant women, and whether they affect ADMA levels in these groups.
A total of 208 pregnant women were included in the study and classified as early-onset (N=57) or late-onset PE (N =49), and as normotensive pregnant women (N = 102).
Pregnant with early-onset PE carrying the GC and GG genotypes for the DDAH2 -449G/C polymorphism had increased ADMA levels (P=0.01). No association of DDAH2 polymorphisms with PE in single-locus analysis was found. However, the G-C-G haplotype was associated with the risk for late-onset PE.
It is suggested that DDAH2 polymorphisms could affect ADMA levels in PE, and that DDAH2 haplotypes may affect the risk for PE.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo2
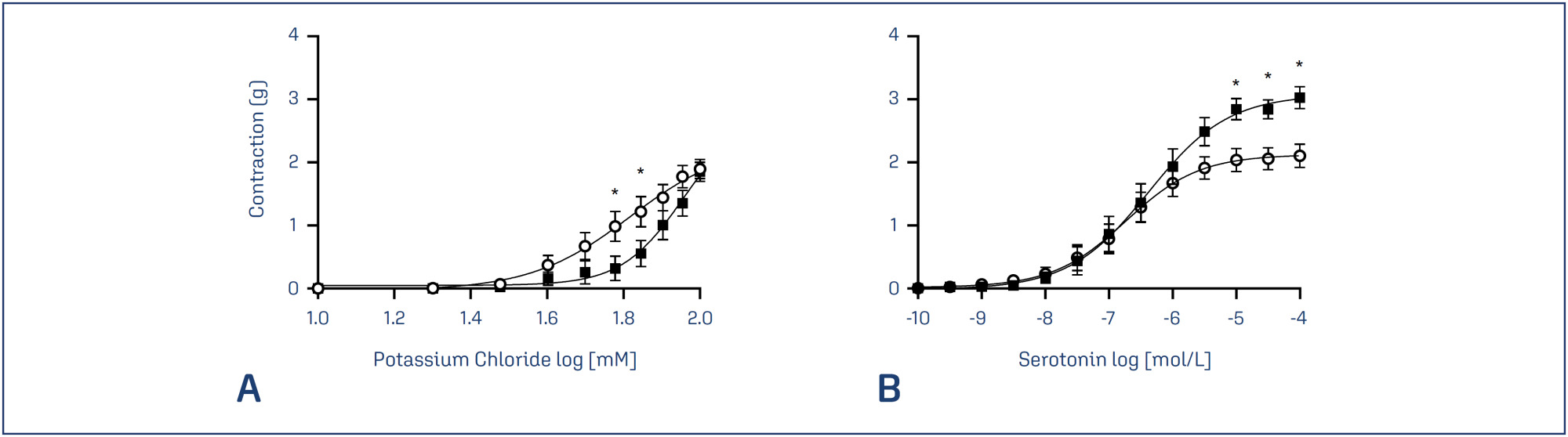
Potassium channels have an important role in the vascular adaptation during pregnancy and a reduction in the expression of adenosine triphosphate-sensitive potassium channels (Katp) has been linked to preeclampsia. Activation of Katp induces vasodilation; however, no previous study has been conducted to evaluate the effects of the inhibition of these channels in the contractility of preeclamptic arteries. Glibenclamide is an oral antihyperglycemic agent that inhibits Katp and has been widely used in vascular studies.
To investigate the effects of the inhibition of Katp, umbilical arteries of preeclamptic women and women with healthy pregnancies were assessed by vascular contractility experiments, in the presence or absence of glibenclamide. The umbilical arteries were challenged with cumulative concentrations of potassium chloride (KCl) and serotonin.
There were no differences between the groups concerning the maternal age and gestational age of the patients. The percentage of smokers, caucasians and primiparae per group was also similar. On the other hand, blood pressure parameters were elevated in the preeclamptic group. In addition, the preeclamptic group presented a significantly higher body mass index. The newborns of both groups presented similar APGAR scores and weights.
In the presence of glibenclamide, there was an increase in the KCl-induced contractions only in vessels from the PE group, showing a possible involvement of these channels in the disorder.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo3
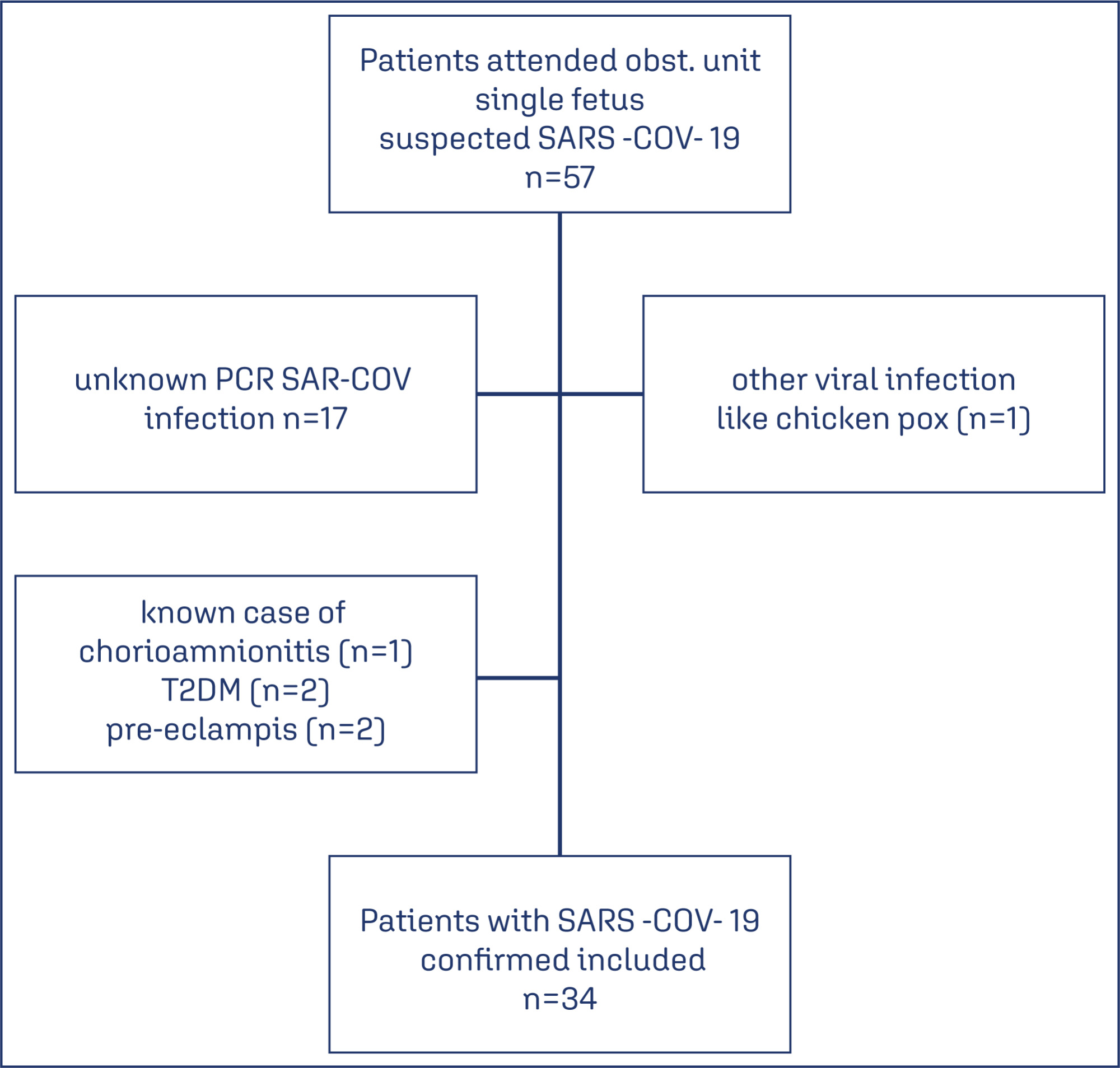
The aims of the study are to describe the association of coronavirus disease (COVID-19) with the abnormal histopathological findings in human placenta and to highlight the potential predictors of these histopathological findings.
A retrospective cohort study, held in two obstetric units from January 2021- 2022, 34 patients who were confirmed cases of COVID- 19 were followed up till the time of delivery as their placenta were sent for histopathology. Patients diagnosed with other viral infections, chorioamnionitis, or were known case of as pre-term or term pre labour rupture of membrans (PROM) were excluded as well as pre exisiting diabetes mellitus or pre-eclampsia. Data analysis were performed using STATA software version 16.
Specific histopatological findings (fetal vascular malperfusion, maternal vascular malperfusion, inflammatory pathology and thrombotic finding) were significantly high among 13 (38.2%) of the study group who got infected earlier in pregnancy (P<0.001). The period between the diagnosis of COVID-19 and the delivery significantly increases the odds of the presence of pathological findings by 2.75 times for each week the patients getting infected earlier.
Association of abnormal placental histopathological findings with COVID-19 infection in pregnancy and the potential predictor for the occurrence of placental findings is the longer duration between the diagnosis of the infection and the delivery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo7
To validate the 10-item Cervantes Scale (CS-10) among Brazilian women.
This is a cross-sectional observational study involving women in the community aged 40–55 years in the Southern region of Brazil. They completed a general health, habits and socio-demographic questionnaire, the CS-10 and the Women’s Health Questionnaire (WHQ). Women unable to understand the survey, not consenting to participate, or having incapacity imposing difficulties during the completion of the questionnaire were excluded. A Confirmatory Factor Analysis (CFA) was conducted with the AMOS 16.0 software. Chi-square of degrees of freedom (χ2/df), the Comparative Fit Index (CFI), the Tucker-Lewis Index (TLI) and the Root-Mean-Square Error of Approximation (RMSEA) were used as indices of goodness of fit. Cronbach’s alpha coefficient was used for internal consistency.
A total of 422 women were included (premenopausal n=35, perimenopausal n=172, postmenopausal n=215). The CFA for the CS-10 showed a good fit (χ²/df=1.454, CFI=0.989; TLI=0.985; RMSEA=0.033; CI 90%=0.002-0.052; PCLOSE=0.921; Model p=0.049). Good reliability was established in CS-10 and WHQ (Cronbach’s alpha=0.724). Postmenopausal women had higher total CS-10 scores (p≤0.0001), reflecting worse quality of life (QoL) related to menopause symptoms and confirming the greater symptomatology evaluated by high total scores for WHQ found in this population when compared to those in the premenopausal period (p=0.041).
The CS-10 is a consistent tool for health-related QoL in Brazilian mid-aged women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo9
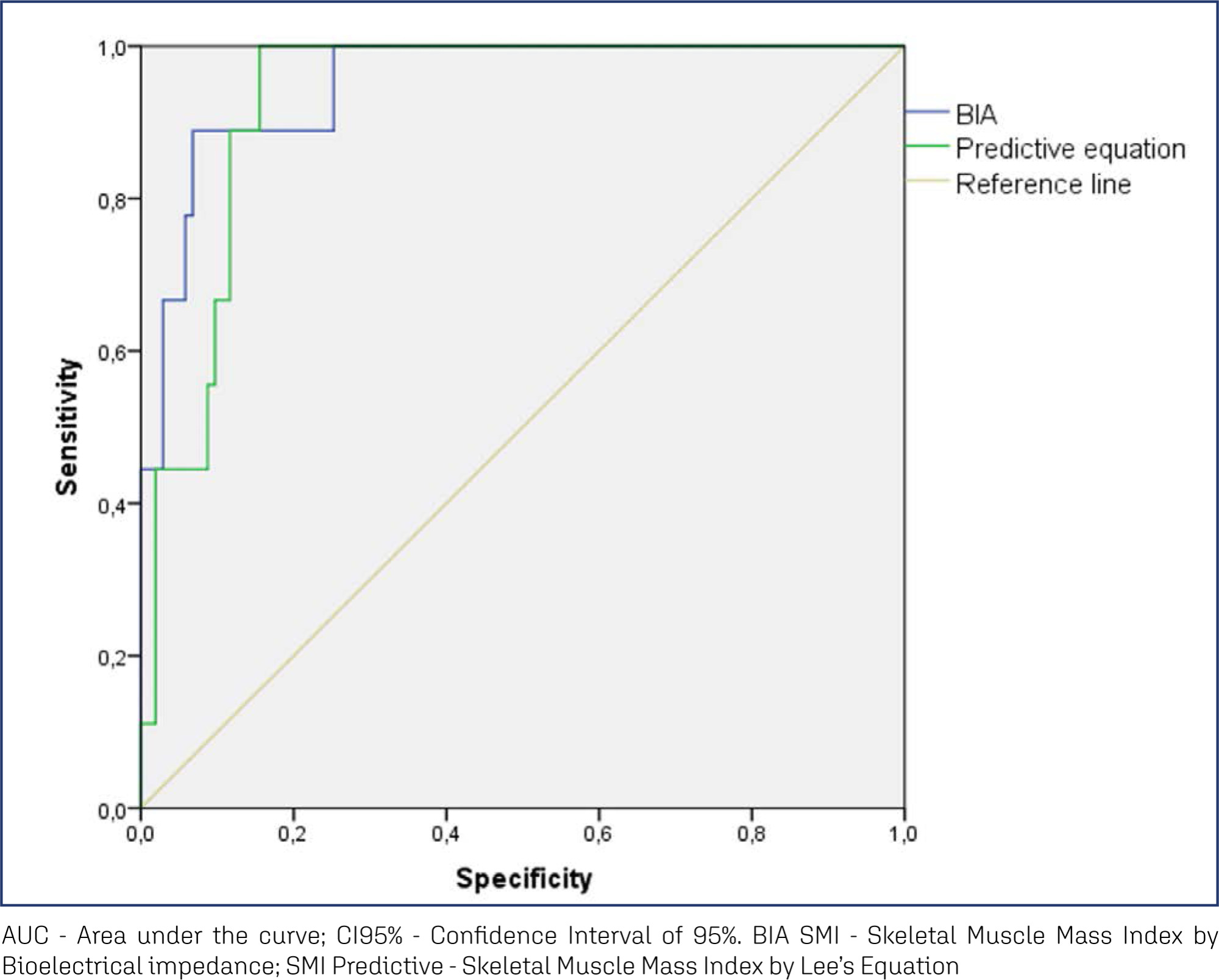
To analyze the amount of muscle and the presence of sarcopenia in postmenopausal women using different methods, verifying the agreement between them as to skeletal muscle mass (SMM).
This cross-sectional observational study was conducted with postmenopausal women aged ≥ 50 years. SMM was obtained from a predictive equation, Bioelectrical Impedance (BIA), and Dual Energy X-Ray Absorptiometry (DXA). The skeletal muscle mass index (SMI) and the appendicular skeletal muscle mass index (ASMI) were calculated. The cut-off point of SMI was determined for the population itself. The agreement between the SMI obtained using the different methods was verified. Sarcopenia was diagnosed according to the criteria proposed by the European Working Group on Sarcopenia in Older People 2 (EWGSOP2). The significance level adopted for all tests was 5.0%.
A total of 112 women were evaluated, with an average age of 66.1 ± 5.65 years. Among them, 51.8% were sufficiently active and 43.8% were overweight and obese. The SMI cut-offs were 6.46 kg/m2 for the predictive equation and 7.66 kg/m2 for BIA, with high sensitivity and specificity. There was an excellent agreement in the identification of SMM by the predictive equation (0.89 [0.824-0.917], p < 0.001) and BIA (0.92 [0.883-0.945], p < 0.001), in reference to DXA. The prevalence of sarcopenia was 0.9%, 1.8%, and 2.7% according to BIA, DXA, and the predictive equation, respectively.
The predictive equation showed the expected agreement in estimating skeletal muscle mass in postmenopausal women, offering a viable and accurate alternative.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo29
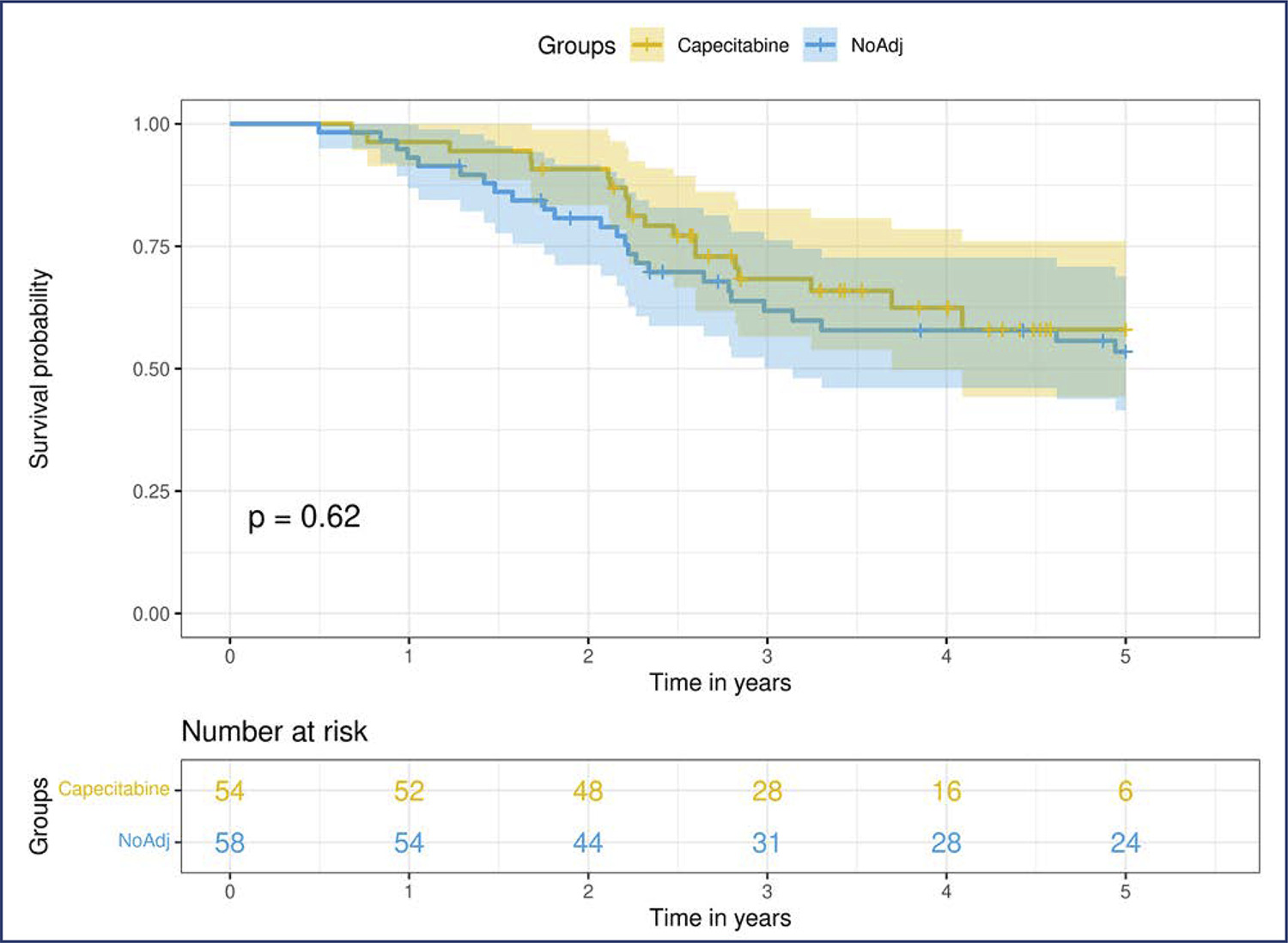
Neoadjuvant chemotherapy (NACT) has become the standard of care for patients with triple-negative breast cancer (TNBC) with tumors > 1 cm or positive axillary nodes. Pathologic complete response (pCR) has been used as an endpoint to select patients for treatment scaling. This study aimed to examine the benefit of adding adjuvant capecitabine for TNBC patients who did not achieve pCR after standard NACT in a real-world scenario.
This retrospective cohort study included all patients with TNBC who underwent NACT between 2010 and 2020. Clinicopathological data were obtained from the patient records. Univariate and multivariate analyses were conducted at the 5 years follow-up period.
We included 153 patients, more than half of whom had stage III (58.2%) and high-grade tumors (60.8%). The overall pCR rate was 34.6%, and 41% of the patients with residual disease received adjuvant capecitabine. Disease-specific survival (DSS) among the patients who achieved pCR was significantly higher (p<0.0001). Residual disease after NACT was associated with detrimental effects on DSS. In this cohort, we did not observe any survival benefit of adding adjuvant capecitabine for patients with TNBC subjected to NACT who did not achieve pCR (p=0.52).
Our study failed to demonstrate a survival benefit of extended capecitabine therapy in patients with TNBC with residual disease after NACT. More studies are warranted to better understand the indication of systemic treatment escalation in this scenario.