Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo19
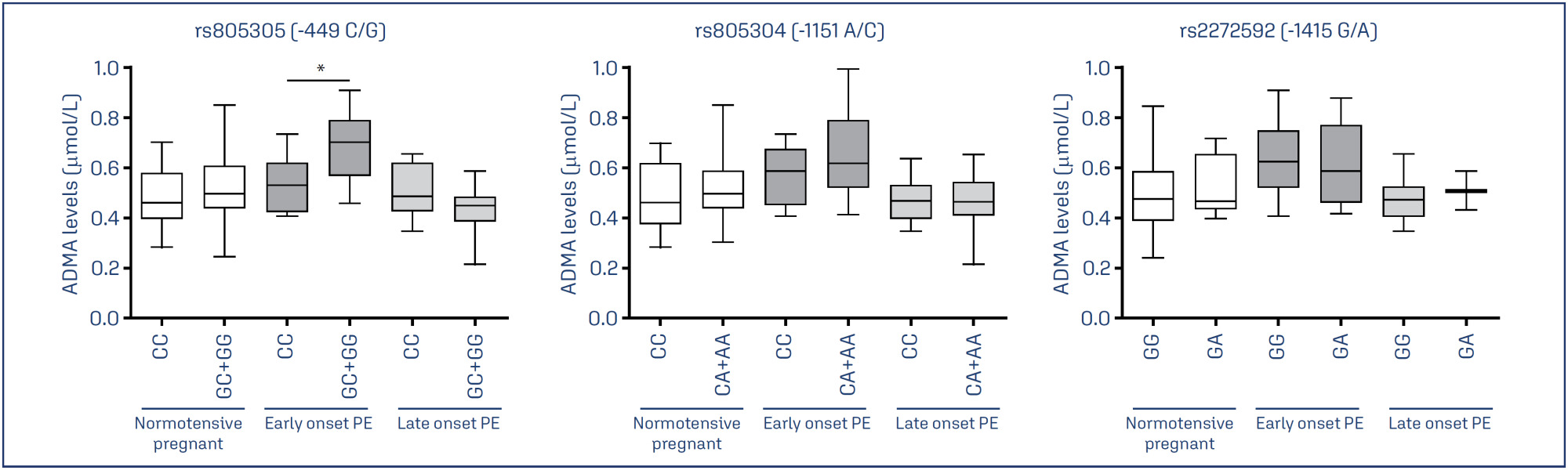
To examine whether the DDAH2 promoter polymorphisms -1415G/A (rs2272592), -1151A/C (rs805304) and -449G/C (rs805305), and their haplotypes, are associated with PE compared with normotensive pregnant women, and whether they affect ADMA levels in these groups.
A total of 208 pregnant women were included in the study and classified as early-onset (N=57) or late-onset PE (N =49), and as normotensive pregnant women (N = 102).
Pregnant with early-onset PE carrying the GC and GG genotypes for the DDAH2 -449G/C polymorphism had increased ADMA levels (P=0.01). No association of DDAH2 polymorphisms with PE in single-locus analysis was found. However, the G-C-G haplotype was associated with the risk for late-onset PE.
It is suggested that DDAH2 polymorphisms could affect ADMA levels in PE, and that DDAH2 haplotypes may affect the risk for PE.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo43
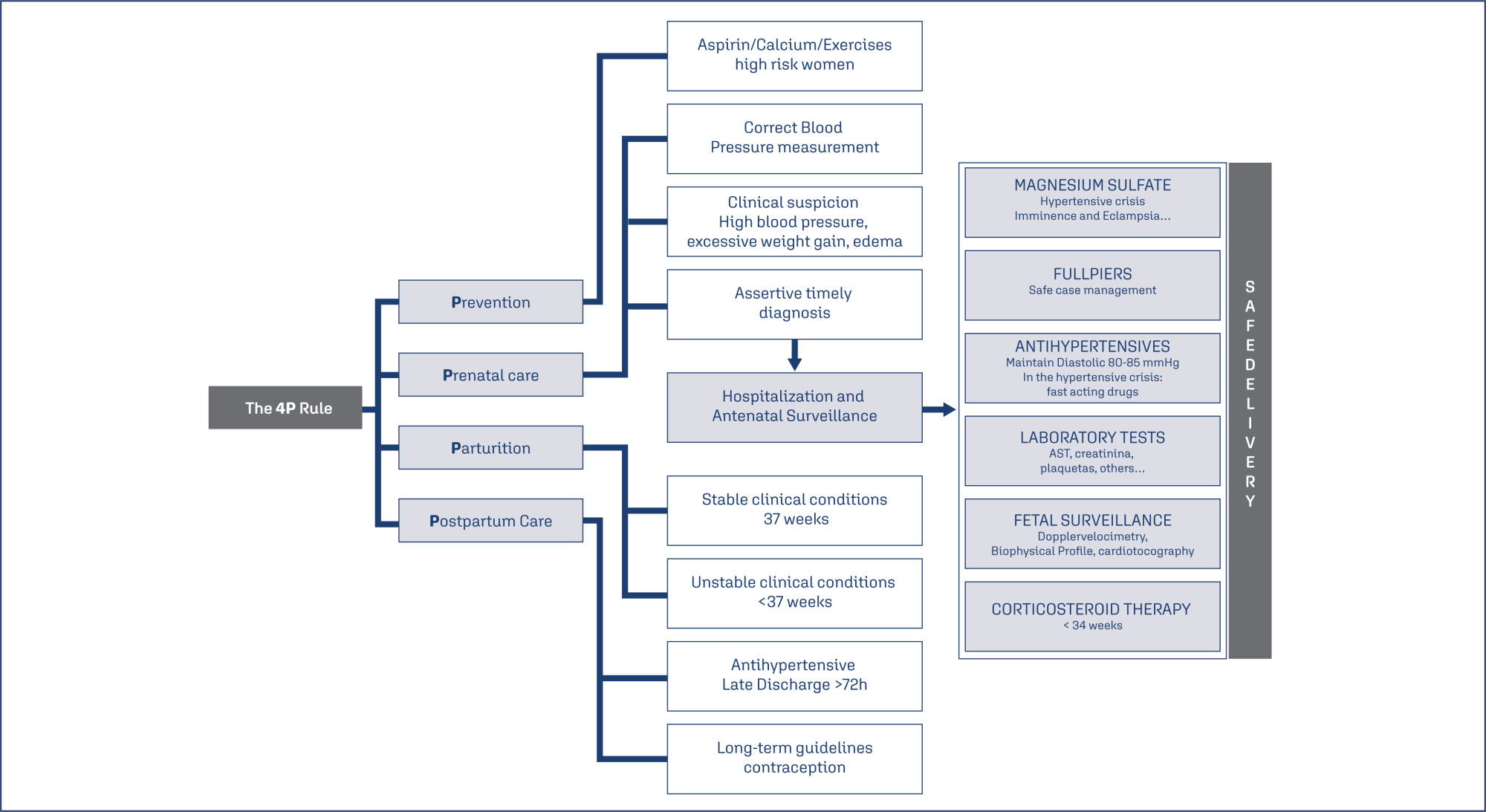
In low and middle-income countries such as Brazil, most maternal deaths are related to hypertensive complications. Preeclampsia is the leading cause of maternal mortality and morbidity. Significant proportion is associated with the following factors: lack of identification of high-risk women, lack of adequate prevention, difficulty in maintaining a high-risk prenatal follow-up, delayed diagnosis, insecurity and low use of magnesium sulphate, delayed pregnancy interruption and lack of postpartum follow-up of these high-risk cases. Four major actions are proposed to minimize this alarming clinical picture and reduce the mortality rates due to preeclampsia, called the "4 P Rule" (Adequate Prevention – Vigilant Prenatal Care – Timely Delivery (Parturition) – Safe Postpartum). From this simple "rule" we can open a range of important processes and reminders that may help in the guidance of preeclampsia management.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):231-237
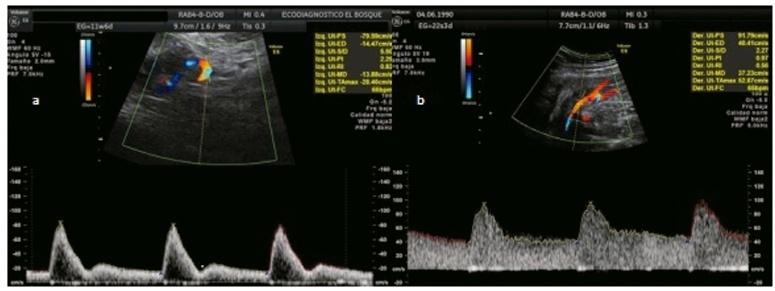
To analyze whether acetylsalicylic (ASA) intake modifies the mean uterine arteries pulsatility index (UtA-PI) at the 2nd or 3rd trimester in a cohort of pregnant women with abnormal mean UtA-PI at between 11 and 14 weeks of gestation.
This is a retrospective cohort study. Singleton pregnancies with abnormal mean UtA-PI at between 11 and 14 weeks of gestation were studied. The participants were divided into 3 groups: 1) If the participant did not take ASA during pregnancy; 2) If the participant took ASA before 14 weeks of gestation; and 3) If the participant took ASA after 14 weeks of gestation. The mean UtA-PI was evaluated at the 2nd and 3rd trimesters, and it was considered to improve when it decreased below the 95th percentile. The prevalence ratio (PR) and the number needed to treat (NNT) werecalculated.
A total of 72 participants with a mean UtA-PI>95th percentile at the 1st trimester of gestation were evaluated. Out of the 18 participants who took ASA, 8 participants started it before 14 weeks of gestation and 10 after. A total of 33.3% of these participants had improved the mean UtA-PI at the 2nd and 3rd trimesters of gestation, although it was not statistically significant (p=0.154). The prevalence ratio was 0.95 (95% confidence interval [CI]: 0.31-1.89), but between the 1st and 2nd trimesters of gestation, the PR was 0.92 (95%CI: 0.21-0.99) and it was statistically significant.
The present work demonstrates a modification of the mean UtA-PI in participants who took ASA compared with those who did not. It is important to check if ASA can modify the normal limits of uterine arteries because this could have an impact on surveillance.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(11):772-773
Pre-eclampsia (PE) is an obstetric disease with a multifactorial cause that affects ∼ 5% of pregnant women. Vision can be affected with varying severity, and retinal detachment is a very rare complication. It tends to be bilateral, diagnosed postpartum, and more prevalent in women who are primiparous and/or undergo caesarean delivery. The condition typically resolves completely and rarely causes total visual loss in the affected women. Fluorescence angiographic findings support the hypothesis that retinal detachment in PE is secondary to choroidal ischemia from intense arteriolar vasospasm. The present article is related to a case of a 37-year-old pregnant woman who had PE associated with a progressive blurred vision, diagnosed by ophthalmology as serous macular detachment of the retina.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(11):697-704
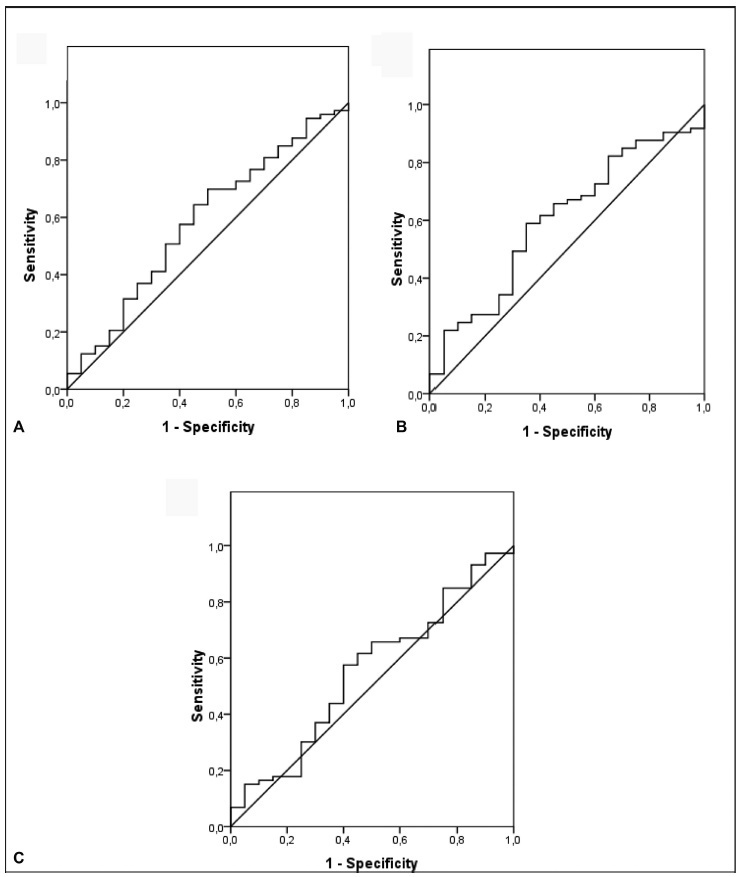
Recent observations support the hypothesis that an imbalance between angiogenic factors has a fundamental role in the pathogenesis of pre-eclampsia and is responsible for the clinical manifestations of the disease. The goal of the present study was to evaluate the sensitivity, specificity, and the best accuracy level of Soluble fms-like tyrosine kinase-1 (sFlt-1), placental growth factor (PlGF), and sFlt-1/PlGF ratio in maternal serum and protein/creatinine ratio in urine sample to define the best cutoff point of these tests to discriminate between the patients with gestational hypertension and the patients with pre-eclampsia, to evaluate the possibility of using them as diagnostic methods.
A prospective longitudinal study was performed, and blood samples were collected from 95 pregnant patients with hypertension to measure serum concentrations of biomarkers sFlt-1 and PlGF. Urine samples were collected for protein screening. Significance was set as p < 0.05.
The sFlt-1/PlGF ratio demonstrated a sensitivity of 57.5% and a specificity of 60% using 50.4 as a cutoff point. The test that showed the best accuracy in the diagnosis of pre-eclampsia was protein/creatinine ratio, with a sensitivity of 78.9% and a specificity of 70% using 0.4 as a cutoff point and showing an area under the receiver operating characteristic curve of 0.80 (p < 0.001).
No studied laboratory test proved to be fairly accurate for the diagnosis of pre-eclampsia, except for the protein/creatinine ratio. The evidence is insufficient to recommend biomarkers sFlt-1 and PlGF to be used for the diagnosis of pre-eclampsia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(11):690-696
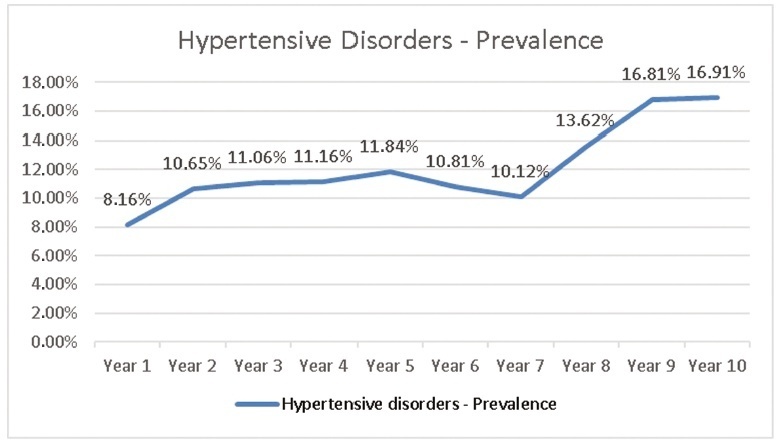
To evaluate the prevalence of hypertensive disorders, perinatal outcomes (preterm infants, low birthweight infants and Apgar score < 7 at the 5th minute and fetal deaths) and the cesarean rates in pregnant women hospitalized for delivery at the Maternidade Hilda Brandão da Santa Casa de Belo Horizonte, Belo Horizonte, state of Minas Gerais, Brazil, from March 1, 2008 to February 28, 2018.
A case-control study was performed, and the groups selected for comparison were those of pregnant women with and without hypertensive disorders. Out of the 36,724 women, 4,464 were diagnosed with hypertensive disorders and 32,260 did not present hypertensive disorders
The prevalence of hypertensive disorders was 12.16%; the perinatal outcomes and cesarean rates between the 2 groups with and without hypertensive disorders were: preterm infants (21.70% versus 9.66%, odds ratio [OR] 2.59, 95% confidence interval [CI], 2.40-2.80, p < 0.001); low birthweight infants (24.48% versus 10.56%; OR 2.75; 95% CI, 2.55-2.96; p < 0.001); Apgar score < 7 at the 5th minute (1.40% versus 1.10%; OR 1.27; 95% CI, 0.97-1.67; p = 0.84); dead fetuses diagnosed prior to delivery (1.90% versus 0.91%; OR 2.12; 95% CI, 1.67-2.70; p < 0.001); cesarean rates (60.22% versus 31.21%; OR 3.34; 95% CI, 3.14-3.55; p < 0.001).
Hypertensive disorders are associated with higher rates of cesarean deliveries and higher risk of preterm infants, low birthweight infants and a higher risk of fetal deaths.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(5):318-332
Pre-eclampsia is a multifactorial and multisystemic disease specific to gestation. It is classically diagnosed by the presence of hypertension associated with proteinuria manifested in a previously normotensive pregnant woman after the 20th week of gestation. Pre-eclampsia is also considered in the absence of proteinuria if there is target organ damage. The present review takes a general approach focused on aspects of practical interest in the clinical and obstetric care of these women. Thus, it explores the still unknown etiology, current aspects of pathophysiology and of the diagnosis, the approach to disease prediction, its adverse outcomes and prevention. Management is based on general principles, on nonpharmacological and on pharmacological clinical treatment of severe or nonsevere situations with emphasis on the hypertensive crisis and eclampsia. Obstetric management is based on preeclampsia without or with signs of clinical and/or laboratory deterioration, stratification of gestational age
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(4):172-177
DOI 10.1590/SO100-720320150005238
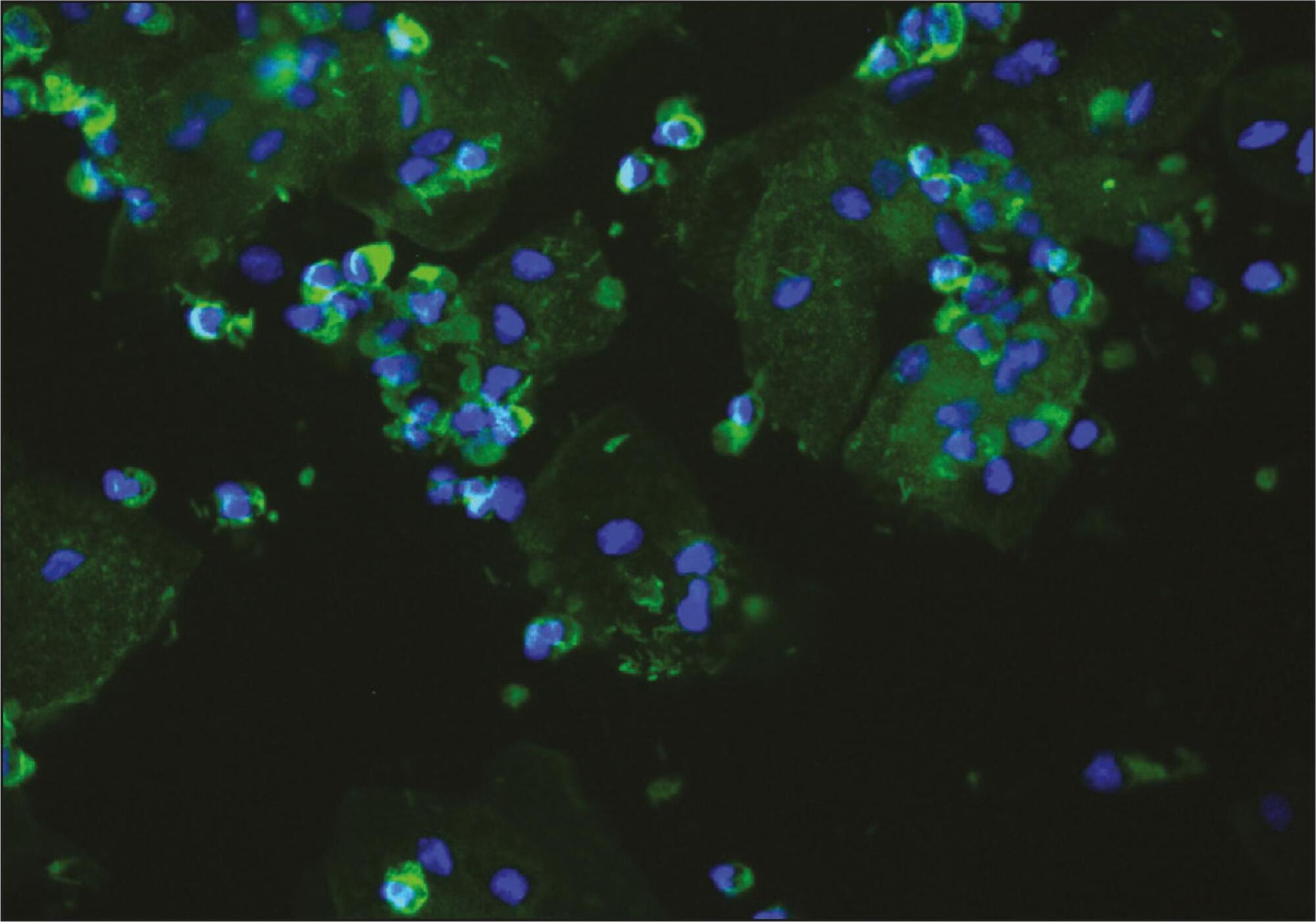
To evaluate the presence of podocyturia in chronic hypertensive pregnant women in the third trimester of pregnancy and its possible association with renal disease.
This was an observational study of a convenience sample of 38 chronic hypertensive pregnant women. The podocytes were labeled by the indirect immunofluorescence technique with anti-podocin and diamidino-phenylindole (DAPI). The count was made on 30 random fields analyzed and corrected according to urinary creatinine (podocytes/mg creatinine). The patients were assigned to two groups: NG (normal glomerular function), up to 100 podocytes, and GP (probable glomerulopathy), more than 100 podocytes. Urinary creatinine was measured by the alkaline picrate method. The variables analyzed were body mass index, gestational age, and systolic and diastolic blood pressure at the time of sample collection. Data were analyzed using the SPSS - version 16.0 (IBM - USA). Statistical analysis was performed by the χ2 test, and significant differences were considered when p<0.05.
The median podocyte count was 20.3 (0.0-98.1) for group GN, and 176.9 (109.1-490.6) for GP. The mean body mass index was 30.2 kg/m2 (SD=5.6), mean gestational age was 35.1 weeks (SD=2.5), median systolic blood pressure was 130.0 mmHg (100.0-160.0) and median diastolic blood pressure was 80.0 mmHg (60.0-110.0). There was no significant correlation between podocyturia and body mass index (p=0.305), gestational age (p=0.392), systolic blood pressure (p=0.540) or diastolic blood pressure (p=0.540).
In this study, there was no podocyturia pattern consistent with the presence of active renal disease, although some of the women studied (15.8%) exhibited a significant loss. We believe that it is premature to recommend the inclusion of the determination of podocyturia in routine prenatal clinical practice in chronically hypertensive pregnant women.