Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):461-466
DOI 10.1590/SO100-720320140005029
To compare clinical and laboratory characteristics, obstetric and perinatal outcomes of patients with pre-eclampsia versus gestational hypertension.
A retrospective study was carried out to analyze medical records of patients diagnosed with pre-eclampsia and gestational hypertension whose pregnancies were resolved within a period of 5 years, for a total of 419 cases. We collected clinical and laboratory data, obstetric and perinatal outcomes. Comparisons between groups were performed using the test suitable for the variable analyzed: unpaired t test, Mann-Whitney U test or χ2test, with the level of significance set at p<0.05.
Were evaluated 199 patients in the gestational hypertension group (GH) and 220 patients in the pre-eclampsia group (PE). Mean body mass index was 34.6 kg/m2 in the GH group and 32.7 kg/m2 in the PE group, with a significant difference between groups. The PE group showed higher systolic and diastolic blood pressure and higher rates of abnormal values in the laboratory tests, although the mean values were within the normal range. Cesarean section was performed in 59.1% of cases of PE and in 47.5% of the GH group; and perinatal outcomes in terms of gestational age and birth weight were significantly lower in the PE group.
Women with gestational hypertension exhibit epidemiological characteristics of patients at risk for chronic diseases. Patients with pre-eclampsia present clinical and laboratory parameters of greater severity, higher rates of cesarean delivery and worse maternal and perinatal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):456-460
DOI 10.1590/SO100-720320140005075
To identify the frequency of polymorphism in the IL-10 gene, rs1800896 (-1082 A/G), in women with preeclampsia (PE) and in women in a control group and to associate the presence of this polymorphism with protection against the development of PE.
This was a case-control study conducted on 54 women with PE, classified according to the criteria of the National High Blood Pressure Education Program, and on 172 control women with at least two healthy pregnancies. The proposed polymorphism was studied by the technique of real time polymerase chain reaction (qPCR), with hydrolysis probes. Statistical analysis was performed using the χ2 test. Odds ratio and confidence interval of 95% were used to measure the strength of association between the studied polymorphism and the development of PE.
Statistically increased frequency of the AG genotype was observed among control women (85 versus 15% in women with PE). The G allele was significantly more frequent among control women than PE women (χ2test, p = 0.01). The odds ratio for carriers of the G allele was 2.13, indicating a lower risk of developing PE compared to non-carriers.
Thus, an association is suggested to occur between the presence of the G allele of the polymorphism in the IL-10 rs1800896 (-1082 A/G) gene and protection against the development of PE. More studies investigating the contribution of these variations and the mechanisms by which they affect the risk of developing PE still need to be undertaken.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(6):259-263
DOI 10.1590/S0100-720320140004812
To analyze the factors related to route of delivery in patients with pre-eclampsia.
A retrospective analytical study was conducted from January 2009 to January 2011, during which 250 medical records of patients diagnosed with pre-eclampsia who gave birth to live fetuses with a gestational age of 28 weeks or more were selected. The variables evaluated were: maternal age (19 years, 20−34 years and over 35 full years), gestational age at delivery (28−37 weeks and more than 37 weeks), parity (primiparous or multiparous), previous cesarean section, history of pre-eclampsia or chronic hypertension, current diagnosis of mild or severe pre-eclampsia, and birth weight of the newborn. The information was transcribed to a questionnaire based on the variables being investigated. The chi-square test was applied to identify the relationship between the variables, with the level of significance set at p<0.05, and the Odds Ratio (OR) was calculated only for the variables showing a statistically significant difference in order to determine the odds for the patient to be submitted to a cesarean section.
In this study, we observed a 78.4% rate of cesarean delivery, with 54.1% of the patients submitted to the procedure having a gestational age of 28 to 37 weeks (OR=3.1; p<0.01). Patients with a history of pre-eclampsia were 2.5 times more likely to have cesarean delivery (OR=2.5; p<0.02). All patients who had had a previous cesarean were submitted to cesarean delivery in the current pregnancy (p<0.01). Pregnant women with severe pre-eclampsia were 3.3 times more likely to progress to cesarean delivery than those with mild pre-eclampsia (OR=3.3; p<0.01).
After individual analysis, only gestational age and a diagnosis of severe pre-eclampsia showed significant differences, representing risk factors for this type of delivery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(8):363-367
DOI 10.1590/S0100-72032013000800005
PURPOSE: To evaluate the perinatal factors that influence the incidence of necrotizing enterocolitis (NEC) in newborns infants (NBI) weighing less than 1,500 g. METHODS: A prospective study that analyzed all infants with birth weight (BW) less than 1,500 g born between January 2006 to December 2010 (n=183). They were divided into two groups, i.e. infants diagnosed with NEC (n=18) and infants without a diagnosis of NEC (n=165), which were compared in terms of perinatal factors that could influence the incidence of NEC. Mean data were compared by Student's t-test or nonparametric tests and percentages of categorical variables were compared by the χ² test. When the variables showed differences between groups, they were analyzed using logistic regression with the dependent variable as the presence of NEC. The statistical package used was SPSS 16.0 for Windows. RESULTS: The two groups were similar in terms of most of the clinical and demographic neonatal and maternal data, except for the presence of preeclampsia (PE), which was higher in patients whose children developed NEC (61.1 versus 35,6%). The presence of PE increased the chance of occurrence of NEC by 2.84 times (95%CI 1.0 - 7.7). CONCLUSION: The only factor that can interfere with the incidence of NEC in infants of very low birth weight was the presence of PE. Awareness of this fact can guide the perinatal team in providing more judicious care regarding the prevention of NEC in this specific population.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(8):357-362
DOI 10.1590/S0100-72032013000800004
PURPOSE: To establish reference values for the first trimester uterine artery resistance index (UtA-RI) and pulsatility index (UtA-PI) in healthy singleton pregnant women from Northeast Brazil. METHODS: A prospective observational cohort study including 409 consecutive singleton pregnancies undergoing routine early ultrasound screening at 11 - 14 weeks of gestation was performed. The patients responded to a questionnaire to assess maternal epidemiological characteristics. The left and right UtA-PI and UtA-RI were examined by color and pulsed Doppler by transabdominal technique and the mean UtA-PI, mean UtA-RI and the presence of bilateral protodiastolic notching were recorded. Quartile regression was used to estimate reference values. RESULTS: The mean±standard deviation UtA-RI and UtA-PI were 0.7±0.1 and 1.5±0.5, respectively. When segregated for gestation age, mean UtA-PI was 1.6±0.5 at 11 weeks, 1.5±0.6 at 12 weeks, 1.4±0.4 at 13 weeks and 1.3±0.4 at 14 weeks' gestation and mean UtA-RI was 0.7±0.1 at 11 weeks, 0.7±0.1 at 12 weeks, 0.6±0.1 at 13 weeks and 0.6±0.1 at 14 weeks' gestation. Uterine artery bilateral notch was present in 261 (63.8%) patients. We observed that the 5th and 95th percentiles of the UtA-PI and UtA-RI uterine arteries were 0.7 and 2.3 and, 0.5 and 0.8, respectively. CONCLUSION: Normal reference range of uterine artery Doppler in healthy singleton pregnancies from Northeast Brazil was established. The 95th percentile of UtA-PI and UtA-RI values may serve as a cut-off for future prediction of pregnancy complications studies (i.e., pre-eclampsia) in Northeast Brazil.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(7):309-316
DOI 10.1590/S0100-72032013000700005
PURPOSE: To determine perinatal outcomes and factors associated with fetal brain sparing effect diagnosed by Doppler flow velocimetry in patients with arterial hypertension. METHODS: We performed a cross-sectional retrospective study including 129 pregnant women with arterial hypertension and submitted to Doppler flow velocimetry, within fifteen days before delivery. Women with multiple pregnancies, fetal malformations, genital bleeding, placenta praevia, premature rupture of membranes, smoking, illicit drug use and chronic diseases were excluded. We analyzed the biological, socio-demographic and obstetric characteristics, as well the perinatal outcomes. To determine the association between variables, we used the χ² test, Fisher's exact test and Student's t-test. Multiple logistic regression analysis was performed to determine the factors associated with fetal centralization. RESULTS: Pre-eclampsia was the most frequent hypertensive disorder (53.5%) and fetal brain sparing effect was observed in 24.0% of fetuses. The prenatal factors associated with fetal brain sparing were the persistence of bilateral protodiastolic notches in uterine arteries (OR 3.6; 95%CI 1.4 - 9.4; p=0.009) and intrauterine growth restriction (IUGR) (OR 3.3; 95%CI 1.2 - 9.3; p=0.02). The perinatal outcomes associated with fetal brain sparing were gestational age <32 weeks, small for gestational age (SGA) infants, birth weight <2,500 g and perinatal death. There was no association with other maternal or neonatal variables. CONCLUSIONS: The main factors associated with fetal brain sparing were persistence of uterine arteries notches, IUGR, and increased frequency of adverse perinatal outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(4):148-152
DOI 10.1590/S0100-72032013000400003
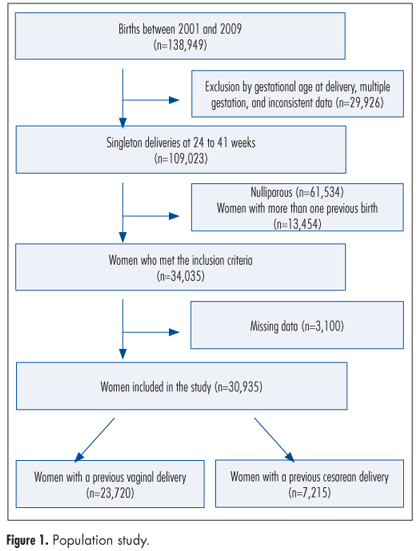
PURPOSE: To examine obstetric outcomes in the second birth of women who had undergone a previous cesarean delivery. METHODS: This was a large hospital-based retrospective cohort study. We included pregnant women who had a previous delivery (vaginal or cesarean) attending their second birth from 2001 to 2009. Main inclusion criteria were singleton pregnancies and delivery between a gestation of 24 and 41 weeks. Two cohorts were selected, being women with a previous cesarean delivery (n=7,215) and those with a vaginal one (n=23,720). Both groups were compared and logistic regression was performed to adjust for confounding variables. The obstetric outcomes included uterine rupture, placenta previa, and placental-related complications such as placental abruption, preeclampsia, and spontaneous preterm delivery. RESULTS: Women with previous cesarean delivery were more likely to have adverse outcomes such as uterine rupture (OR=12.4, 95%CI 6.8-22.3), placental abruption (OR=1.4, 95%CI 1.1-2.1), preeclampsia (OR=1.4, 95%CI 1.2-1.6), and spontaneous preterm delivery (OR=1.4, 95%CI 1.1-1.7). CONCLUSIONS: Individuals with previous cesarean section have adverse obstetric outcomes in the subsequent pregnancy, including uterine rupture, and placental-related disorders such as preeclampsia, spontaneous preterm delivery, and placental abruption.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(3):102-106
DOI 10.1590/S0100-72032012000300002
PURPOSE: To assess the prevalence of obstetric risk factors and their association with unfavorable outcomes for the mother and fetus. METHODS: A longitudinal, descriptive and analytical study was conducted on 204 pregnant women between May 2007 and December 2008. Clinical and laboratory assessments followed routine protocols. Risk factors included socio-demographic aspects; family, personal and obstetric history; high pre-gestational body mass index (BMI); excessive gestational weight gain and anemia. Adverse outcomes included pre-eclampsia (4.5%), gestational diabetes mellitus (3.4%), premature birth (4.4%), caesarian birth (40.1%), high birth weight (9.8%) and low birth weight (13.8%). RESULTS: The average age was 26±6.4 years; the mothers were predominantly non-white (84.8%), 51.8% had incomplete or complete secondary level schooling, 67.2% were in a stable marital relationship and 51.0% had a regular paid job; 63.7% were admitted to the prenatal clinic during the second trimester and 16.7% during the first, with 42.6% being primiparous. A past history of chronic hypertension was reported by 2.9%, pre-eclampsia by 9.8%, excessive gestational weight gain by 15.2% and former gestational diabetes mellitus by 1.0%. In the current pregnancy, elevated pre-gestational BMI was found in 34.6%; 45.5% presented with excessive gestational weight gain, 25.3% with anemia and 47.3% with dyslipidemia. Of the 17.5% of cases with altered blood glucose, gestational diabetes mellitus was confirmed in 3.4% and proteinuria occurred in 16.4% of all cases. Adverse maternal fetal outcomes included pre-eclampsia (4.5%), gestational diabetes mellitus (3.4%), premature birth (4.4%), caesarean birth (40.1%) and high and low birth weight (9.8% and 13.8%, respectively). Independent predictors of adverse maternal fetal outcomes were identified by Poisson multivariate regression analysis: pre-gestational BMI>25 kg/m² was a predictor for pre-eclampsia (RR=17.17; 95%CI 2.14-137.46) and caesarian operation (RR=1.79; 95%CI 1.13-2.85), previous caesarean was a predictor for present caesarean operation (RR=2.28; 95%CI 1.32-3.92) and anemia and high gestational weight gain were predictors for high birth weight (RR=3.38; 95%CI 1.41-8.14 and RR=4.68; 95%CI 1.56-14.01, respectively). CONCLUSION: Pre-gestational overweight/obesity, previous caesarean, excessive weight gain and anemia were major risk factors for pre-eclampsia, caesarean operations and high birth weight.