You searched for:"Edison Capp"
We found (8) results for your search.-
Review Article
Timing of semen cryopreservation: before or after processing?
Rev Bras Ginecol Obstet. 2024;46:e-rbgo36
Summary
Review ArticleTiming of semen cryopreservation: before or after processing?
Rev Bras Ginecol Obstet. 2024;46:e-rbgo36
Views158Abstract
Objective:
Seminal cryopreservation causes significant damage to the sperm; therefore, different methods of cryopreservation have been studied. The aim of the study was to compare the effects of density gradient processing and washing/centrifugation with seminal plasma removal for cryopreservation in semen parameters.
Methods:
Seminal samples of 26 normozoospermic patients were divided into 3 parts: with seminal plasma; after washing/centrifugation; and after selection through density gradient. The samples were cryopreserved for at least two weeks. Motility, sperm count, morphology and viability were evaluated before cryopreservation and after thawing.
Results:
Density gradient processing selected motile and viable sperm with normal morphology in fresh samples (p<0.05). Cryopreservation negatively affected all sperm parameters regardless of the processing performed, and even if the sperm recovery was lower in the density gradient after the thawing, progressive motility, total motility, viability and morphology remained higher (p<0.05).
Conclusion:
Cryopreservation significantly compromises sperm parameters (motility, morphology, viability). In normozoospermic patients, the density gradients select better quality spermatozoa compared to other processing methods; this benefit was kept after thawing.
Key-words CentrifugationcryopreservationDensity gradientSemenSeminal plasmaSperm countSperm washSpermatozoaSee more -
Short Communication
Medical Residents, the Group and the Formation of Professional Identity During the COVID-19 Pandemic
Rev Bras Ginecol Obstet. 2022;44(8):797-801
Summary
Short CommunicationMedical Residents, the Group and the Formation of Professional Identity During the COVID-19 Pandemic
Rev Bras Ginecol Obstet. 2022;44(8):797-801
Views4See moreAbstract
Residency is still considered the gold standard for quality medical training, and acquiring a professional identity as a specialist is one of its central elements. Residents obtain this identity through both the educational environment and direct interaction with peers and supervisors. However, modifications in health care and educational routines during the recent coronavirus disease 2019 (COVID-19) pandemic have significantly impaired these channels. This study is part of a qualitative research project to analyze professional identity formation in a medical residency program in obstetrics and gynecology at a public hospital in southern Brazil. The authors conducted 28 semi-structured interviews with medical residents and preceptors, as well as a focus group with the residents, which was recorded, transcribed, and analyzed in an effort to construct major analytical categories. Restricted movement and physical contact have forced the use of alternative means of interpersonal interaction, such as communication through social media or instant messaging applications. This has also affected educational activities, such as morning rounds, lectures, and seminars. These changes represent a significant impact, especially in Brazil, where physical proximity is an important cultural feature, even in the work and school environments. We speculate that this new type of virtual interaction will also affect the formation of professional identity among obstetrician-gynecologists. These findings suggest that medical residency programs should be attentive to changes in resident training to ensure that the specialist profile and the expected skills, which are consolidated over many years, are not lost.
-
Original Article
Ovarian Tissue Culture to Preserve Fertility in Transgender Male Patients after Hormonal Treatment
Rev Bras Ginecol Obstet. 2022;44(3):251-257
Summary
Original ArticleOvarian Tissue Culture to Preserve Fertility in Transgender Male Patients after Hormonal Treatment
Rev Bras Ginecol Obstet. 2022;44(3):251-257
Views1Abstract
Objective
To evaluate the reproductive and histological characteristics of fresh cultured ovarian tissue from transgender male patients.
Methods
An in vitro pilot study in which samples were collected during sex reassignment surgery for transgender male patients. The ovarian cortex was cut into fragments of 2 mm, 3mm, and 4 mm, and placed in a 96-well plate suitable for cultivation at days 0, 2, 4, 6, and 8, when the histology was analyzed.
Results
Stromal hyperplasia was observed in all samples, and it was not associated with the obtainment of primordial or primary follicles. Peripheral reduction in cell count was also a recurrent finding. Primordial and primary follicles were identified with a heterogeneous pattern in fragments from the same patient and from different patients, and follicles in more advanced stages of development (secondary and antral) were not found. There was an association between the diameter of the ovarian fragments and the identification of primary follicles (p=0.036). The number of days in culture was associated with histological signs of tissue damaging in the fragments (p=0.002). The total number of follicles identified in the samples with 2mm in diameter was significantly lower than in those that measured 4mm in diameter (p=0.031).
Conclusion
A diameter of 4mm is suitable for ovarian tissue culture with the benefit of ease of handling. Even after prolonged exposure to testosterone, the ovarian fragments presented primordial and primary follicles, maintaining viability throughout the days they were exposed to the culture. Freezing the ovarian cortex of transgender patients who will undergo surgery for gender reassignment would be an interesting option, in the future, for the preservation of fertility.
Key-words fertility preservationgender reassignment surgeryovarian reserveovarytissue culture techniquesSee more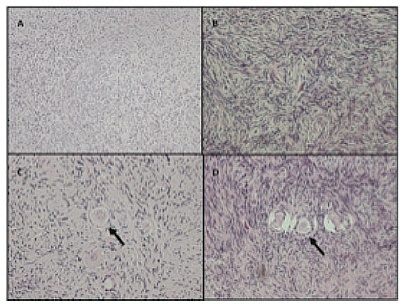
-
Original Article
Antral Follicles Count and Anti-Müllerian Hormone Levels after Gonadotoxic Chemotherapy in Patients with Breast Cancer: Cohort Study
Rev Bras Ginecol Obstet. 2017;39(4):162-168
Summary
Original ArticleAntral Follicles Count and Anti-Müllerian Hormone Levels after Gonadotoxic Chemotherapy in Patients with Breast Cancer: Cohort Study
Rev Bras Ginecol Obstet. 2017;39(4):162-168
Views1Abstract
Aim
To assess ovarian reserve (OVR) by means of follicle-stimulating hormone (FSH), anti-Müllerian hormone (AMH), and antral follicle count (AFC) measurement in eumenorrheic women with breast cancer, exposed to gonadotoxic chemotherapy.
Method
Fifty-two women (35.3 ± 3.8 years old) with breast cancer and undergoing cyclophosphamide-containing chemotherapy were enrolled. The assessment was performed before chemotherapy (T1) and after 2 (T2) and 6 months (T3).
Results
Six months after chemotherapy, the prevalence of regular cycles was 60%. Anti-Müllerian hormone decreased down to undetectable levels at T2 and T3 (T1: 2.53 [1.00–5.31]; T2 < 0.08; T3: < 0.08 [< 0.08–1.07] ng/mL), (p< 0.0001). Antral follicle count was 11 [8.0–13.5] follicles at T1 and lower at T2 (5.50 [3.75–8.0] and T3 (5.0 [2.5–7.0]) (p< 0.0001). In patients who remained with regular cycles during chemotherapy or resumed normal menses, FSH and estradiol levels remained unchanged.
Conclusion
Anti-Müllerian hormone and AFC are useful as markers of OVR decline in women exposed to chemotherapy. Follicle-stimulating hormone is only adequate in women who become amenorrheic.
Key-words anovulationanti-Müllerian hormoneantral follicle countchemotherapy-induced amenorrheaovarian reserveSee more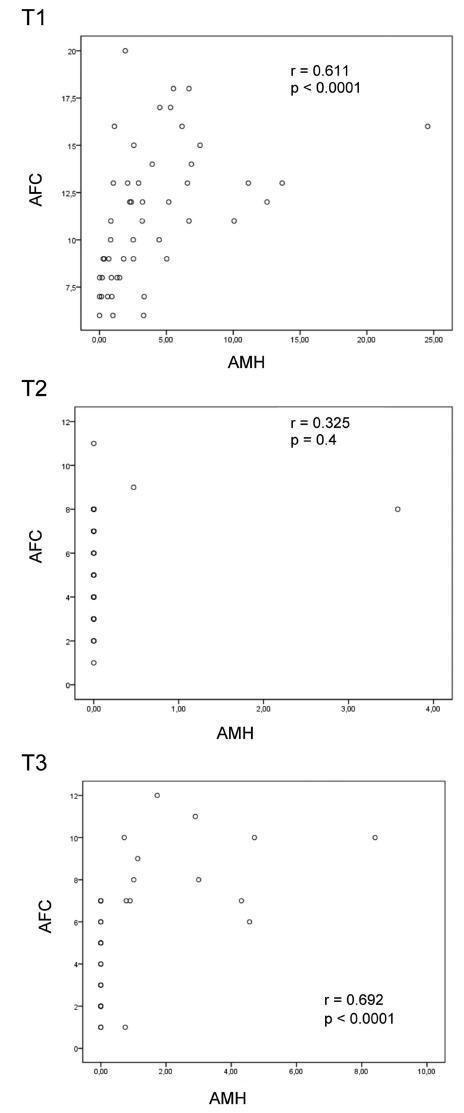
-
Artigos Originais
Factors associated with postpartum weight retention in a Brazilian cohort
Rev Bras Ginecol Obstet. 2015;37(4):164-171
Summary
Artigos OriginaisFactors associated with postpartum weight retention in a Brazilian cohort
Rev Bras Ginecol Obstet. 2015;37(4):164-171
DOI 10.1590/SO100-720320150005186
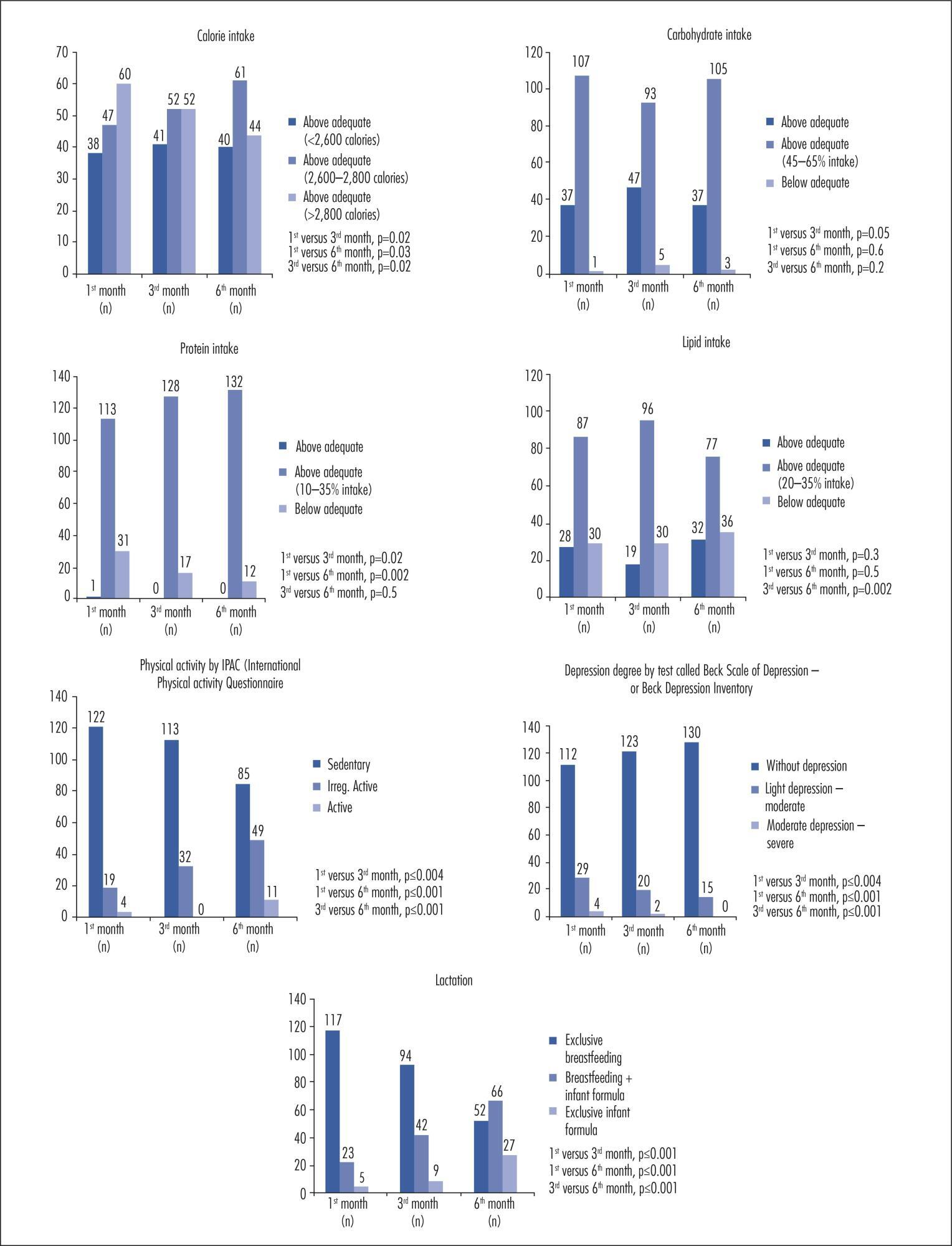
Views2See morePURPOSE:
To identify the factors associated with weight retention after pregnancy.
METHODS:
A cohort study was performed with 145 women receiving maternity care at a hospital in Caxias do Sul, Rio Grande do Sul, Brazil, aged 19 to 45 years, between weeks 38 and 42 of pregnancy. The patients were evaluated at one month, three months, and six months after delivery. Student’s t-test or one-way analysis of variance (ANOVA) was used to compare groups, as indicated; correlations were assessed with Pearson’s and Spearman’s tests, as indicated; to identify and evaluate confounders independently associated with total weight loss, a multivariate linear regression analysis was performed and statistical significance was set at p≤0.05.
RESULTS:
There was a significant positive association between total weight gain – and a negative association with physical exercise during pregnancy – with total weight loss. Higher parity, inter-pregnancy interval, calorie intake, pre-pregnancy body mass index (BMI), weight gain related to pre-pregnancy BMI, presence and severity of depression, and lack of exclusive breastfeeding were directly associated with lower weight loss. Among nominal variables, level of education and marital status were significantly associated with total weight loss.
CONCLUSION:
In the present study, lower weight retention in the postpartum period was associated with higher educational attainment and with being married. Normal or below-normal pre-pregnancy BMI, physical activity and adequate weight gain during pregnancy, lower parity, exclusive breastfeeding for a longer period, appropriate or low calorie intake, and absence of depression were also determinants of reduced weight retention.
-
Review Article
Current treatment of leiomyomas
Rev Bras Ginecol Obstet. 2007;29(6):324-328
Summary
Review ArticleCurrent treatment of leiomyomas
Rev Bras Ginecol Obstet. 2007;29(6):324-328
DOI 10.1590/S0100-72032007000600008
Views3Leiomyomas are benign tumors. They appear in the myometrium and present a variable amount of fibrous conjunctive tissue. About 75% of the cases are not symptomatic and are usually found during abdominal, bimanual pelvic examination or during ultrasonography. The symptoms are directly related to the size, number and localization of the myomas. In the present review, the current clinical therapeutic procedures (oral anti-conceptive drugs, progestins and anti-progestins, analogues of the gonadothrophins’ releasing hormone (GnRH), and non-steroid anti-inflammatory drugs), and also the surgical procedures (hysterectomy, myomectomy, embolization) are presented for the treatment of leiomyomas.
Key-words Embolization, therapeuticGonadotropin-releasing, hormonehysterectomyleiomyomamyomaReceptors, progesteroneSee more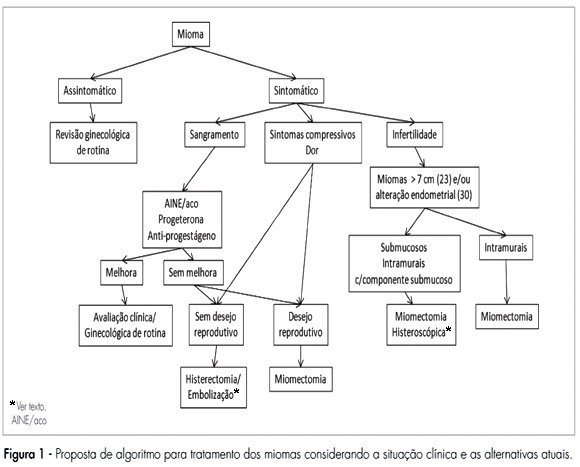
-
Original Article
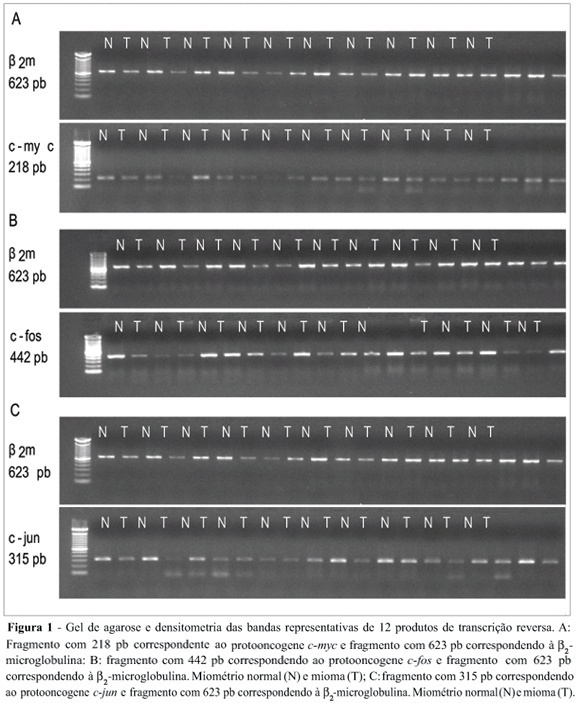
Expression of the protooncogenes c-fos, c-myc and c-jun in human normal miometrium and leiomyoma
Rev Bras Ginecol Obstet. 2006;28(10):590-595
Summary
Original ArticleExpression of the protooncogenes c-fos, c-myc and c-jun in human normal miometrium and leiomyoma
Rev Bras Ginecol Obstet. 2006;28(10):590-595
DOI 10.1590/S0100-72032006001000004
Views3See moreUterine myomas are common benign tumors of the female genital tract. The expression of growth factor signal transduction cascade components including the protooncogenes c-myc, c-fos, and c-jun seem to be involved in the development of myomas. PURPOSE: To compare the gene (mRNA) and protein expression of the protooncogenes c-fos, c-myc, and c-jun in human normal myometrium and leiomyoma. METHOD: A case-control study was performed. Samples were collected from 12 patients submitted to hysterectomy at the Hospital de Clínicas at Porto Alegre. The expression of the specific mRNA for c-myc, c-fos, c-jun, and beta-microglobulin was assessed through the RT-PCR technique, using specific primers to each gene. The protein expression of these protooncogenes was evaluated through the Western blot technique with specific antibodies. RESULTS: No statistically significant difference was observed in the gene expression for these protooncogenes between normal myometrium and leiomyoma (c-myc: 0,87 ± 0,08 vs 0,87 ± 0,08, p = 0,952; c-fos: 1,10 ± 0,17 vs 1,01 ± 0,11, p = 0,21; c-jun: 1,03 ± 0,12 vs 0,96 ± 0,09, p = 0,168, respectively). No statiscally significant difference was observed for the protein expression of these protooncogenes between normal myometrium and leiomyoma (c-myc: 1,36 ± 0,48 vs 1,53 ± 0,29, p = 0,569; c-fos: 8,85 ± 5,5 vs 6,56 ± 4,22, p = 0,434; e c-jun: 6,47 ± 3,04 vs 5,42 ± 2,03, p = 0,266, respectively). CONCLUSION: No difference was observed in the gene expression (transcription) nor in the protein expression (translation) of the protooncogenes c-myc, c-fos, and c-jun between leiomyoma and myometrium.
-
Original Article
Gonadal cytogenetic analysis in patients with primary amenorrhea
Rev Bras Ginecol Obstet. 2005;27(3):125-129
Summary
Original ArticleGonadal cytogenetic analysis in patients with primary amenorrhea
Rev Bras Ginecol Obstet. 2005;27(3):125-129
DOI 10.1590/S0100-72032005000300005
Views3See moreBACKGROUND: patients with primary amenorrhea and gonadal dysgenesia have higher serum gonadotrophins and should be submitted to chromosome studies. Karyotype studies may be performed in gonadal tissue or peripheral blood however, it is not yet established if cases of primary amenorrhea without signs of virilization need additional investigation of gonadal karyotype. PURPOSE: to analize the gonadal karyotypes (ovaries) from patients with primary amenorrhea and compare them to their respective peripheral blood karyotypes. METHODS: clinical and karyotype data of 12 patients were retrospectively analyzed from January 1997 to December 2003. RESULTS: when the investigation was indicated for primary amenorrhea without signs of virilization, the gonadal and peripheral blood karyotypes were concordant in 8 cases (7 cases 46XX and 1 case 46XY). One patient with virilization signs was the only case of discordant karyotype. CONCLUSION: the present study suggests that the gonadal karyotype does not bring additional information to peripheral blood karyotype in patients with amenorrhea and no signs of virilization. Although all previous studies had a small number of patients, it seems advisable to investigate the gonadal karyotype in patients with signs of virilization. The cost-benefit analysis could allow cost and stress reduction for patients, family and institutions.
Search
Search in:
Tag Cloud
breast (42) breast cancer (42) breast neoplasms (95) Cesarean section (72) endometriosis (66) infertility (56) Maternal mortality (43) menopause (82) obesity (58) postpartum period (40) pregnancy (225) Pregnancy complications (99) Prenatal care (68) prenatal diagnosis (50) Prevalence (41) Quality of life (51) risk factors (94) ultrasonography (79) urinary incontinence (40) women's health (48)


