Summary
Rev Bras Ginecol Obstet. 2024;46:e-rbgo36
Seminal cryopreservation causes significant damage to the sperm; therefore, different methods of cryopreservation have been studied. The aim of the study was to compare the effects of density gradient processing and washing/centrifugation with seminal plasma removal for cryopreservation in semen parameters.
Seminal samples of 26 normozoospermic patients were divided into 3 parts: with seminal plasma; after washing/centrifugation; and after selection through density gradient. The samples were cryopreserved for at least two weeks. Motility, sperm count, morphology and viability were evaluated before cryopreservation and after thawing.
Density gradient processing selected motile and viable sperm with normal morphology in fresh samples (p<0.05). Cryopreservation negatively affected all sperm parameters regardless of the processing performed, and even if the sperm recovery was lower in the density gradient after the thawing, progressive motility, total motility, viability and morphology remained higher (p<0.05).
Cryopreservation significantly compromises sperm parameters (motility, morphology, viability). In normozoospermic patients, the density gradients select better quality spermatozoa compared to other processing methods; this benefit was kept after thawing.
Summary
Rev Bras Ginecol Obstet. 2008;30(11):561-565
DOI 10.1590/S0100-72032008001100006
PURPOSE: to evaluate the influence of age on the quality of semen in men submitted to spermatic analysis in a human reproduction service, in cases of conjugal infertility. METHODS: a retrospective study in which the spermiograms of all men in process of investigation for conjugal infertility in a service of assisted reproduction in the Northeast of Brazil were evaluated from September 2002 to December 2004. A number of 531 individuals submitted to 531 spermatic evaluations were included in the study. The following parameters have been analyzed: spermatic volume, concentration, motility and morphology. The men under investigation have been divided in groups, according to the results obtained in each of the variables studied. Seminal volume groups were divided in: hypospermia, normospermia and hyperspermia. Spermatic concentration groups were divided in: azoospermia, oligospermia, normospermia and polyspermia. Motility groups were divided in: normal motility and asthenospermia. Morphology groups were divided in: normal morphology and teratospermia. The t test has been used to compare the average age of patients in groups with normal and in groups with altered parameters. The program XLSTAT (p<0.05) has been used for the statistical analysis. RESULTS: the individuals studied presented an average of 37±7.9 years old, with an average of seminal volume of 3±1.4 mL, a spermatic concentration of 61.4±66.4 spermatozoids by mL of semen, a progressive motility of 44.7±19.4% of the total of spermatozoids and normal morphology of 11.2±6.6% of the spermatozoids. Average age among groups were similar, except for that of individuals with hypospermia, which was significantly higher than the one from men with normospermia (39.6±10.3 versus 36.5±7.3, p=0.001). CONCLUSIONS: age interferes in an inversely proportional way on the ejaculated volume, but does not influence spermatic concentration, motility and morphology.
Summary
Rev Bras Ginecol Obstet. 2008;30(4):171-176
DOI 10.1590/S0100-72032008000400003
PURPOSE: the propose of this study was to analyze the clinical and laboratorial parameters of patients submitted to human assisted reproduction techniques with association of sperm processing techniques, in order to remove virus particles from semen samples of couples in which men was infected by human immunodeficiency virus (HIV). METHODS: it was assessed 11 intracytoplasmatic sperm injection (ICSI) cycles from couples whose men were HIV seropositive (HIV Group), and 35 cycles in which semen donors' samples were used in ICSI procedures (Control Group). Semen samples from Control Group were submitted to routine semen analysis, sperm wash and cryopreservation. The man from HIV Group received previous antibiotic therapy; the semen samples were analyzed routinely and prepared by sperm wash and density gradient method before cryopreservation. Those samples were evaluated to viral load and ICSI was performed when no HIV was detected. RESULTS: regards to semen analysis the groups were similar to sperm concentration and progressive motility. Nevertheless, the percentage of sperm with normal morphology were higher on Control Group (14.3%) than HIV (5.8%; p=0.002). On embryo parameters assessment, the normal fertilization (CT: 74.7% and HIV: 71.7; p=0.838, respectively) and good embryos rate (CT: 42.4% and HIV: 65.1%; p=0.312, respectively) were comparable. On the other hand, the Control Group presented better clinic results than HIV Group (ongoing pregnancy rate: 52.9% versus 12.5%; p=0.054, and implantation rate: 42.6 versus 10.4%; p=0.059, respectively), however the differences were not statistically significant. After delivery, no seroconversion was observed on mother and child. CONCLUSIONS: the association of sperm processing techniques in order to remove HIV from semen samples does not influence in laboratorial parameters of assisted reproduction techniques cycles. On the other hand, it has been demonstrated excellent results getting safety gametes to serodiscordant couples.
Summary
Rev Bras Ginecol Obstet. 2006;28(12):708-714
DOI 10.1590/S0100-72032006001200004
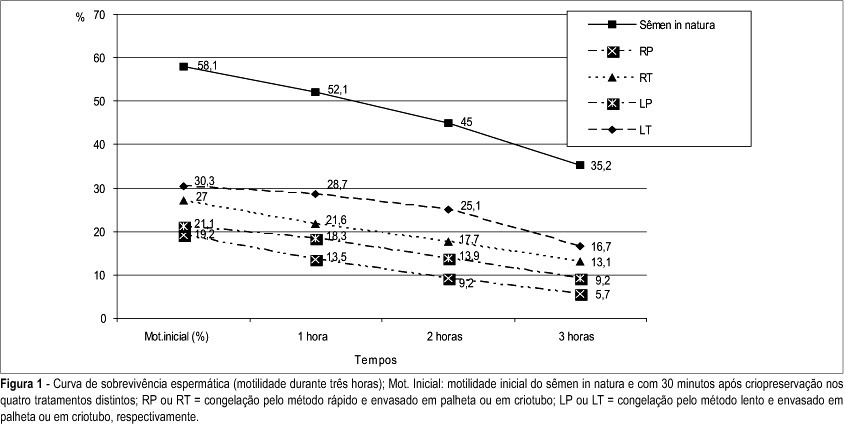
PURPOSE: to compare two different methods of freezing and two types of human semen storage during cryopreservation process. METHODS: experimental research in which the cryopreservation of 18 semen samples from 18 volunteers was studied. Following the addition of the cryoprotectant medium, Test-yolk buffer, the semen samples were packaged into 0.25 mL straws or into 2 mL cryotubes and submitted to cryopreservation by slow or rapid methods, in four different treatments: RS (cryopreservation by rapid method and packaged in straws), RT (rapid-cryotubes), SS (slow-straws), and ST (slow-cryotubes). Samples were thawed after 24 hand then maintained at 37ºC. Data collected were analyzed by the Student t-test, with p<0.05, using the SPSS computer program for Windows®, version 11.0.0. RESULTS: the motility of spermatozoa decreased after the cryopreservation process. The initial motility rate was 58.1% and motilities after the different methods of cryopreservation were 19.2% (RS), 27% (RT), 21.1% (SS) and 30.3% (ST). There was a significant decrease of the normal morphology. The initial normal morphology was 14.2% and morphologies after the different methods of cryopreservation were 12.8% (RS), 12.6% (RT), 12.6% (SS) and 12.4% (ST). CONCLUSIONS: the slow method of cryopreservation with storage in cryotubes showed the best recovery of motile cells after freezing and thawing. There was no difference among the methods when appraised the morphology.
Summary
Rev Bras Ginecol Obstet. 2006;28(11):652-657
DOI 10.1590/S0100-72032006001100004
PURPOSE: to determine if the previous fertility history can predict current fertility status of a patient examined for couple’s infertility. METHODS: retrospective study involving semen analyses from 183 consecutive subfertile patients evaluated from September 2002 to March 2004. We excluded those patients who had undergone radio or chemotherapy, orchiectomy or vasectomy. Mean values of all analyses were used for patients with multiple semen analysis. Patients with more than 20x10(6) sperm/mL, motility higher than 50% and with normal strict sperm morphology higher than 14% were considered normal. Patients were divided into two groups, according to the fertility status: primary infertility (118 patients) and secondary infertility (65 patients). Data were analyzed according to the chi2 test and the Student t-test. RESULTS: no differences were detected in the mean age between patients with primary infertility, 37.3±6.3, and secondary infertility, 38.1±5.9; p=0.08. In the group of patients with primary infertility, 51.9% (61 patients) had a normal sperm concentration, 70.3% (83 patients) had normal sperm motility and 26.3% (31 patients) had normal sperm morphology. In the group of patients with secondary infertility, 53.8% (35 patients) had normal sperm concentration, 75.4% (49 patients) had normal sperm motility and 32.3% (21 patients) had normal sperm morphology. No significant differences were detected in sperm concentration (21.3x10(6)/mL versus 23.1x10(6)/mL; p=0.07), motility (45.2 versus 48.1%; p=0.08) and morphology (6.1 versus 6.4%; p=0.09) between groups of patients with primary and secondary infertility. CONCLUSIONS: semen analysis should be requested even in cases of prior male fertility. Physicians should not presume a patient to have a normal semen analysis based on his previous history of initiating a pregnancy.
Summary
Rev Bras Ginecol Obstet. 2006;28(1):44-49
DOI 10.1590/S0100-72032006000100008
PURPOSE: to evaluate the influence of abstinence period on seminal characteristics in infertile men and to establish a better seminal quality after pooling the samples. METHODS: a retrospective study was performed on 88 oligozoospermic (n=25), asthenozoospermic (n=43), and oligoasthenozoospermic (n=20) men whose partners underwent intrauterine insemination between September 2002 and December 2004. We excluded men with a normal semen analysis or women with abnormalities suggestive of infertility. Each man produced two semen samples in a short period of time (30 min to 1 h). We evaluated semen volume, total motile sperm count and percentage sperm motility. Comparisons were made between the first and second semen samples. After pooling the samples, we compared the total motile sperm count between the first sample and the pooled samples. Statistical evaluation was performed by Student's t test and the chi2 test. RESULTS: in oligozoospermic men, there were no differences in the semen characteristics between the first and the second seminal samples (p>0.05). The total motile sperm count increased significantly in the second sample in comparison to the first sample in asthenozoospermic (42.4±6.8 vs 51.5±7.2x10(6) sperm/mL) and oligoasthenozoospermic men (11.1±7.4 vs 14.35±7.2x10(6) sperm/mL (p<0.05). The pool of two ejaculates increased the total motile sperm count in comparison to the first sample (p<0.05) in oligozoospermic, asthenozoospermic and oligoasthenozoospermic men by 110.5, 110.3 and 136.03%, respectively. CONCLUSIONS: a short period of abstinence is associated with higher sperm motility in infertile men. The pool of two semen samples is a way to increase the total motile sperm count in this group of patients whose wives want to undergo an intrauterine insemination instead of in vitro fertilization.
Search
Search in:
breast (42) breast cancer (42) breast neoplasms (95) Cesarean section (72) endometriosis (66) infertility (56) Maternal mortality (43) menopause (82) obesity (58) postpartum period (40) pregnancy (225) Pregnancy complications (99) Prenatal care (68) prenatal diagnosis (50) Prevalence (41) Quality of life (51) risk factors (94) ultrasonography (79) urinary incontinence (40) women's health (48)