Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(3):149-154
DOI 10.1590/S0100-72032005000300009
PURPOSE: to analyze the efficacy, safety and real advantage of vesicoamniotic shunt catheter in the intrauterine treatment of obstructive uropathy. METHODS: a retrospective and descriptive study, in which the evolution of 35 fetuses with obstructive uropathy, submitted to vesicoamniotic shunt from 1990 to 2004 in a Fetal Medical Center was evaluated. All these fetuses fitted the selection criteria defined by a protocol of this service, and had the parents' consent for the procedure. The Pediatric Nephrology Sector of the Hospital das Clínicas of UFMG assessed all of them after delivery to confirm the prenatal diagnosis and outcome. The dead neonates were studied by the Pathological Anatomy Sector of UFMG. Descriptive analysis of the following parameters was performed: prenatal diagnosis of the uropathy, gestational age at shunt insertion, time of catheter utilization, post-surgery complications, perinatal mortality and neonatal survival. RESULTS: posterior urethral valve was the most common uropathy (62.8%). The mean gestational age at the vesicoamniotic shunt placement was 26.1weeks and the mean time of its presence was 46 days (1-119 days). There were four intrauterine fetal deaths and 17 in the neonatal period (60% perinatal mortality). The main cause of death was pulmonary hypoplasia. Olygohidramnios was present in 33/35 fetuses (94.3%) and it was reversed in 23 of them (70%); fourteen fetuses survived the neonatal period. At present, there are 4 children followed up by the Pediatric Sector of Nephrology of Hospital das Clínicas. Two of them have been treated with peritoneal dialysis, awaiting renal transplantation. The other two have normal renal function. Their age varies from 2 months to 4 years. CONCLUSION: the vesicoamniotic shunt may be a viable intrauterine treatment for severe obstructive uropathy, with 40% of survival rate of fetuses that might have progressed to death. However, the procedure's success was directly related to the adequate selection, and to the early intervention in the uterus, performed before 32 weeks of gestation in fetuses with bilateral obstruction, without any associated malformation and with still preserved renal function. Olygohidramnios reversion did not guarantee a good prognosis. It remains controversial if the vesicoamniotic shunt can really ensure long-term renal function.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(3):155-160
DOI 10.1590/S0100-72032005000300010
PURPOSE: to evaluate the outcome of fetuses with risk of chromosomal anomalies over 1:300, based on the nuchal translucency measurement, according to the Fetal Medicine Program. METHODS: in the pregnancies with risk of chromosomal anomalies over 1:300, variables like fetal karyotype, spontaneous or induced abortion, prematurity, stillbirth, neonatal death, malformations, and healthy newborn were considered. We used Fisher's exact test to compare differences in proportions between groups. RESULTS: we selected 193 (3.6%) single pregnancies with risk of chromosomal anomalies over 1:300. Only 165 cases fulfilled the inclusion criteria. Of these only 32.1% underwent fetal karyotyping and of which 8.5% had chromosomal anomalies (85.7% had trisomy 21). Regarding pregnancy outcomes, 4.2% were spontaneous miscarriages, 4.2% induced abortions, 4.8% were premature, 1.8% had neonatal death, 1.8% were stillborn, and 4.2% had structural malformation (85.7% congenital heart diseases). Almost 85.0% were healthy newborns. Patients with abnormal karyotyping had more induced abortions (p<0.001) and more structural malformations (p<0.001) than patients with normal karyotyping. None of the genetic diseases or miscarriages was associated with invasive procedures. Sixty-six percent of the pregnancies with prenatal diagnosis of abnormal karyotype were interrupted. CONCLUSION: nuchal translucency is an important screening tool for chromosomal diseases especially for low-risk pregnancies. However, counseling pregnancies with high risk of chromosomal anomalies should consider that, although these fetuses have a worse prognosis, most of the outcomes are favorable.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):575-579
DOI 10.1590/S0100-72032005001000002
PURPOSE: to verify the occurrence of colonization by Streptococcus agalactiae in pregnant women attended at the prenatal outpatient clinic of the Teaching Maternity Hospital of Rio de Janeiro University (UFRJ) and to evaluate the susceptibility of the isolates to antimicrobial agents. METHODS: a total of 167 pregnant women between the 32nd and 41st week of gestation, regardless of risk factors, attended at the antenatal clinic between February 2003 and February 2004, were evaluated. The vaginal/anal material, collected by the same swab, was inoculated in Todd-Hewitt broth to which nalidixic acid (15 µg/mL) and gentamicin (8 µg/mL) were added, with following subcultures onto sheep blood-agar. Identification was carried out observing colony morphology and beta-hemolysis type on blood-agar, catalase, cAMP, and serological tests. The antimicrobial susceptibility testing used agar diffusion and agar dilution methods. Statistical analysis was performed by the chi2 test with the level of significance set at p<0,05. RESULTS: the frequency of colonization was 19.2%, with no significant differences when age, number of gestations, number of abortions and the presence or absence of diabetes mellitus were compared (p>0.05). All 32 isolated strains were susceptible to penicillin, cefotaxime, ofloxacin, chloramphenicol, vancomycin and meropenem. Resistance to erythromycin and clindamycin was detected in 9.4 and 6.2% of the isolates, respectively. CONCLUSIONS: the relatively high incidence (19.2%) of colonization by S. agalactiae among the evaluated pregnant women and the recovery of antimicrobial resistant strains, especially those recommended in cases of penicillin allergy, emphasize the importance, for a correct prevention of neonatal infections, of detecting colonization at the end of pregnancy and evaluating antimicrobial susceptibility.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):580-587
DOI 10.1590/S0100-72032005001000003
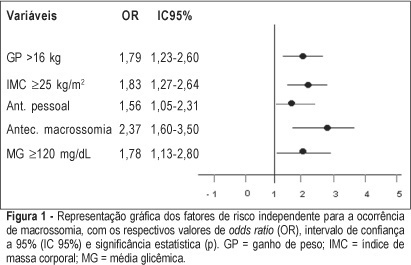
PURPOSE: to identify risk factors for fetal macrosomia in pregnant women with diabetes or daily hyperglycemia. METHODS: retrospective study, control-case, including 803 pairs of mothers and newborns belonging to this specific population, divided into two groups - macrosomic (cases, n=242) and non-macrosomic (controls, n=561). Variables regarding age, parity, weight and body mass index (BMI), weight gain (WG), diabetes history, high blood pressure and tabagism, diabetes type and classification, and glycemic control indicators in the third trimester were compared. The means were evaluated by the F test and the categorized variables were submitted to univariate analysis using the chi² test. The significative results were included in the multiple regression model for the identification of macrosomia independent risk considering OR, 95% CI and p value. The statistical significance limit of 5% was established for all analyses. RESULTS: there was a significative association between macrosomia and WG >16 kg, BMI >25 kg/m², personal, obstetric and macrosomic history, classification in the Rudge groups (IB and IIA + IIB), glycemic mean (GM) >120 mg/dL and postprandial glycemic mean >130 mg/dL in the third trimester. In the multiple regression analysis, WG >16 kg (OR=1,79; 95% CI: 1,23-1.60), BMI >25 kg/m² (OR=1.83; 95% CI: 1.27-2.64), personal history of diabetes (OR=1.56; 95% CI: 1.05-2.31) and of macrosomia (OR=2.37; 95% CI: 1.60-3.50) and GM >120 mg/dL in the third trimester (OR=1.78; 95% CI: 1.13-2.80) confirmed to be independent risk factors for macrosomia in these pregnancies. CONCLUSION: WG >16 kg, BMI >25 kg/m², GM >120 mg/dL in the third trimester and personal history of macrosomia and diabetes were identified as risk factors for fetal macrosomia in pregnant women with diabetes or daily hyperglycemia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):588-593
DOI 10.1590/S0100-72032005001000004
PURPOSE: to evaluate the prevalence of intrauterine adhesions after manual vacuum aspiration for the treatment of abortion. METHODS: a prospective, descriptive study, with group comparison was carried out between November 2000 and August 2001 on 80 women between 15 and 48 years old, admitted to a public hospital for abortion care. Manual vacuum aspiration consisted of extracting the uterine content by suction using a Karman syringe connected to plastic cannulas. Intrauterine adhesions were screened by hysteroscopy, performed 40-60 days after the aspiration. Statistical analysis was performed using Fisher exact test, ANOVA and estimation of prevalence risk, when indicated. RESULTS: hysteroscopy identified intrauterine adhesions in 13 patients (prevalence = 16.3%), most of them of the mucosal type (9 of 13), minimal severity (11 of 13) and lateral location in the uterus (5 of 13). Adhesions were more frequent at a gestational age more than 8 weeks (24.4 vs 3.7%; prevalence risk of 6.6) as well as in missed abortion (41.7 vs 12.1% ; prevalence risk of 3.54). CONCLUSIONS: prevalence of intrauterine adhesions after manual vacuum aspiration was 16.3%. Missed abortion and advanced gestational age seem to be associated with the occurrence of adhesions.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):594-598
DOI 10.1590/S0100-72032005001000005
PURPOSE: to verify if there is any difference in the number of miscarriages and newborns with low weight in patients with scleroderma (SSc) when compared with women without the disease, between the two clinical variants of the disease and when the expression of SSc occurred before or after the gestation. METHODS: twenty-six patients were analyzed regarding the number of pregnancies, miscarriages, sex, and birth weight of the children, studying the clinical variant of the disease and the temporal relationship between diagnosis and gestation. The patients had not used either medications that could interfere in gestation or had any other disease that could do it. For control, twenty-six healthy women, without diseases that might alter the gestation, of the same ages and socioeconomic status were studied. For the statistical analysis study, tables of frequency, tables of contingency, and Fisher, chi2 and Mann-Whitney tests were used. Statistical significance was considered when p<0.05. RESULTS: among the patients with SSc, there were 96 gestations with 13.5% (n=13) of miscarriages. In the control group, there were 94 gestations with 9.6% (n=9) of miscarriages. There were no differences in the number of newborns with low weight between the two groups (cases, n=8 and controls, n=6, with p=0.54), nor in the number of miscarriages (p=0.46). However, the number of newborn babies with low weight was significantly higher among the cases with the diffuse disease (diffuse form, n=4 and limited, n=4, with p=0.04) and among patients that became pregnant after the diagnosis of SSc (37.5% in women known to be sick and 6.7% in women who became pregnant before getting ill, with p=0.03). The number of male newborns was higher in the women with SSc (p=0.002). CONCLUSIONS: the women with SSc showed a higher number of low-weight newborns in the group with diffuse disease and when pregnancy occurred after the clinical diagnosis of the disease.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):599-606
DOI 10.1590/S0100-72032005001000006
PURPOSE: comparative analysis of the outcome of women with advanced pelvic endometriosis and women with tubal sterilization submitted to intracytoplasmic sperm injection (ICSI). METHODS: ninety-three infertile women, with normal menstrual cycle, without hormonal or surgical treatment during 12 months, body mass index of 20-25, ovaries with no tumors or cysts were included in the present study and divided into two groups: tubal sterilization (TUB), 39 women, and endometriosis (EDT), 54 women with III-EDT and IV-EDT, undergoing ovulatory induction using r-FSH and ICSI. Clinical and laboratorial data were compared. chi2, Fisher, Student's t, and Mann-Whitney tests were employed. RESULTS: lower estradiol levels (2,243.1 vs 1,666.3; p=0.001) and lower number of follicles per patient (16.9 vs 13.9, p=0.001) were noted in EDT group, in spite of more units of r-FSH (1,775.6 vs 1,998.6; p=0.007, for TUB and EDT, respectively). There were no differences in the rates of retrieved oocyte (69 vs 73.5%; p=0.071) as well as in normal fertilization rates (83.7 vs 81.7%; p=0.563, for TUB and EDT, respectively. However, lower number of top quality preembryos were obtained in patients from EDT group (36.5 vs 24.8%, TUB and EDT, respectively; p=0.005). Total pregnancy (41.0 vs 42.6%; p=0.950) and implantation rates (13.9 vs 14.5%; p=0.905) were not different when groups TUB and EDT were compared. CONCLUSIONS: ovaries of women from EDT group seem to be less responsive to ovulatory induction with r-FSH. EDT seems to impair the mean number of follicles and top quality preembryos with no impairment of retrieved oocyte and fertilization rates. However, once obtained, preembryos from EDT patients are able to exhibit similar implantation potential and pregnancy when compared with patients from TUB group.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):607-612
DOI 10.1590/S0100-72032005001000007
PURPOSE: to test the hypothesis that gene TP53 codon 72 polymorphism is a risk factor for premalignant and malignant cervical lesions associated or not with human papillomavirus (HPV). METHODS: uterine cervical samples were collected for HPV DNA and TP53 codon 72 polymorphism tests from 155 patients who underwent cervical biopsy. Three groups were formed according to histological diagnosis: low-grade squamous intraepithelial lesion (LSIL), high-grade squamous intraepithelial lesion (HSIL) and cervical carcinoma. Subjects without cytological and histological displasic changes were considered controls. To verify the association between the gene TP53 codon 72 polymorphism and the groups, the chi2 test was applied. Confidence interval was considered significant at 95% (alpha=0.05). RESULTS: forty subjects were found to present cervical carcinoma, 18 had HSIL, 24 had LSIL and 73 were grouped as controls. The genotype Arg/Arg p53 was found in 60% of the patients with cancer, in 50.0% of the cases with HSIL, 45.8% with LSIL, and in 45.2% of the controls. No significant differences were identified in the frequencies of p53 genotype between all groups, independently of the presence of HPV (chi2: 3.7; p=0.716). CONCLUSIONS: our data do not support hypothesis that the gene TP53 codon 72 polymorphism is important for the development of pre-malignant and malignant cervical lesions associated or not with HPV.