-
Case Report06-18-2021
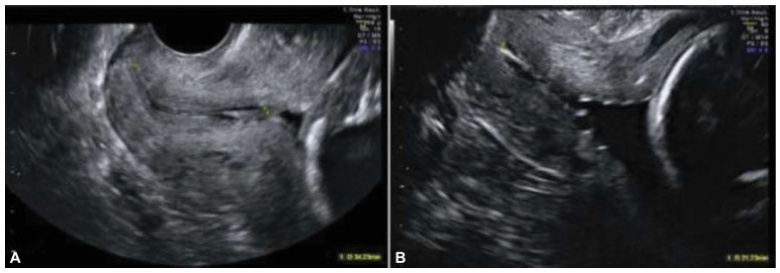
A Scary Complication: Single-center Study on Management and Outcome of Cesarean Scar Pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):311-316
Abstract
Case ReportA Scary Complication: Single-center Study on Management and Outcome of Cesarean Scar Pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):311-316
Views152See moreAbstract
A cesarean scar pregnancy (CSP) is a scary and life-threatening complication of cesarean section (CS). Nevertheless, the incidence of CS is constantly growing. The CSP incidence is 0,15% of pregnancies after CS which represents 6,1% of all ectopic pregnancies in women with condition after CS. Therefore, it should be more present in the clinical daily routine. From mild nonspecific symptoms to hypovolemic shock, diagnosis and therapy must be performed quickly. With the progressive growth of the scar pregnancy, a uterine rupture involves the risk of severe bleeding, and an emergency hysterectomy could be necessary. Prolongation of pregnancy has been successful only in a few cases.We report 11 cases from our hospital in the past 10 years. In the discussion, treatment options of this complication with an increasing incidence, which is associated with serious morbidity and mortality, are presented based on the current literature. Treatment options include drug therapy, but also surgical or combined procedures with radiological intervention.

-
Original Article06-18-2021
Continuation Rates of the 52-mg Levonorgestrel-releasing Intrauterine System according to the Primary Reason for its Use
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):291-296
Abstract
Original ArticleContinuation Rates of the 52-mg Levonorgestrel-releasing Intrauterine System according to the Primary Reason for its Use
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):291-296
Views185Abstract
Objective
To evaluate whether continuation rates with the 52-mg levonorgestrelreleasing intrauterine system (LNG-IUS) up to 5 years after placement differed between women using the method exclusively for contraception and those using the device for medical reasons alone.
Methods
A retrospective cohort study was conducted in a family planning clinic with 5,034 LNG-IUS users: 4,287 using the method exclusively for contraception and 747 for medical reasons alone. The continuation rate at 1 to 5 years of use was calculated by life table analysis.
Results
Initially, the continuation rate was significantly higher in the contraception group: 85.8 versus 83.4 and 77.4 versus 76.0 per 100 women-years in the 1st and 2nd years of use, respectively. There were more discontinuations due to bleeding/spotting in the medical reasons group in the first two years. The discontinuation rate according to reason for use was not significantly different from the third to the fifth year of use. No women discontinued due to amenorrhea in either group.
Conclusion
The continuation rate was significantly higher in the contraception group in the first two years of use. Amenorrhea was not a reason for discontinuation in either group, suggesting that counselling in this respect was adequate. Nevertheless, counselling could perhaps have been better with regards to the expected long period of bleeding and spotting in the first two years after placement.
Key-words Amenorrheableeding and spottingcontinuation ratecounsellingindication for uselevonorgestrel IUSSee morePlumX Metrics
- Citations
- Citation Indexes: 3
- Usage
- Full Text Views: 94
- Abstract Views: 18
- Captures
- Readers: 16
-
Original Article06-18-2021
Is there a Role for Antenatal Corticosteroids in Term Infants before Elective Cesarean Section?
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):283-290
Abstract
Original ArticleIs there a Role for Antenatal Corticosteroids in Term Infants before Elective Cesarean Section?
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):283-290
Views208See moreAbstract
Objective
Cesarean section (CS) delivery, especially without previous labor, is associated with worse neonatal respiratory outcomes. Some studies comparing neonatal outcomes between term infants exposed and not exposed to antenatal corticosteroids (ACS) before elective CS revealed that ACS appears to decrease the risk of respiratory distress syndrome (RDS), transient tachypnea of the neonate (TTN), admission to the neonatal intensive care unit (NICU), and the length of stay in the NICU.
Methods
The present retrospective cohort study aimed to compare neonatal outcomes in infants born trough term elective CS exposed and not exposed to ACS. Outcomes included neonatal morbidity at birth, neonatal respiratory morbidity, and general neonatal morbidity. Maternal demographic characteristics and obstetric data were analyzed as possible confounders.
Results
A total of 334 newborns met the inclusion criteria. One third of the population study (n=129; 38.6%) received ACS. The present study found that the likelihood for RDS (odds ratio [OR]=1.250; 95% confidence interval [CI]: 0.454-3.442), transient TTN (OR=1.,623; 95%CI: 0.556-4.739), and NIUC admission (OR=2.155; 95%CI: 0.474-9.788) was higher in the ACS exposed group, although with no statistical significance. When adjusting for gestational age and arterial hypertension, the likelihood for RDS (OR=0,732; 95%CI: 0.240-2.232), TTN (OR=0.959; 95%CI: 0.297–3.091), and NIUC admission (OR=0,852; 95%CI: 0.161-4.520) become lower in the ACS exposed group.
Conclusion
Our findings highlight the known association between CS-related respiratory morbidity and gestational age, supporting recent guidelines that advocate postponing elective CSs until 39 weeks of gestational age.
PlumX Metrics
- Citations
- Citation Indexes: 3
- Usage
- Full Text Views: 74
- Abstract Views: 13
- Captures
- Readers: 34
-
Original Article06-18-2021
The Effect of Dialectic Behavioral Counseling on Depression, Anxiety, and Postpartum Hematocrit Level
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):275-282
Abstract
Original ArticleThe Effect of Dialectic Behavioral Counseling on Depression, Anxiety, and Postpartum Hematocrit Level
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):275-282
Views202See moreAbstract
Objective
Childbirth is a biological, psychological, and sociological event that can be a positive or negative experience, and, without support, this period may be potentially damaging. Parturition may distort maternal emotions and lead to short- or long-term disorders such as postpartum depression and anxiety. The present research aims to study the effects of dialectic behavioral therapy-based counseling on depression, anxiety symptoms, and postpartum hematocrit level.
Methods
The current research is a clinical trial study, and the sample was selected using parturients who were referred to the Health General Center with a diagnosis of postpartum depression and anxiety. The sample size consisted of 116 subjects who agreed to participate in the study. The patients in intervention group underwent group dialectic behavioral counseling (10 sessions/one session per week) and the control group did not receive any type of intervention. The patients were assessed in the first and last sessions as well as 2 months after the end of the sessions, using the Beck depression scale and Spielberg anxiety scale as well as the results of hematocrit tests. Data were analyzed using the IBMSPSS Statistics for Windows, Version 21.0 (IBMCorp., Armonk, NY, USA)
Results
The results implied the effectiveness of dialectic behavioral therapy on reduction of the depression score, anxiety symptoms (p-value ≤ 0.0001), and hematocrit level (p-value=0.04). The participants’ depression, anxiety, and hematocrit levels decreased in the experiment group compared to the control group, and this decrease has remained until the 2-month follow-up.
Conclusion
It seems that dialectic behavioral counseling reduces the levels of postpartum depression, anxiety, and hematocrits.
PlumX Metrics
- Citations
- Policy Citations: 1
- Citation Indexes: 3
- Usage
- Full Text Views: 59
- Abstract Views: 3
- Captures
- Readers: 79
-
Original Article06-18-2021
The Impact of Routine Transvaginal Ultrasound Measurement of the Cervical Length on the Prediction of Preterm Birth: A Retrospective Study in a Tertiary Hospital
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):264-274
Abstract
Original ArticleThe Impact of Routine Transvaginal Ultrasound Measurement of the Cervical Length on the Prediction of Preterm Birth: A Retrospective Study in a Tertiary Hospital
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):264-274
Views200Abstract
Objective
To evaluate the applicability and usefulness of second-trimester TUCL to predict PTB in a cohort of Portuguese pregnant women.
Methods
Retrospective cross-sectional cohort study including all singleton pregnant women who performed their second-trimester ultrasound (between weeks 18 and 22þ6 days) from January 2013 to October 2017 at Centro Hospitalar Universitário São João.
Results
Our cohort included 4,481 women. The prevalence of spontaneous PTB was of 4.0%, with 0.7% occurring before the 34th week of gestation. The mean TUCL was of 33.8mm,and percentiles 3, 5 and 10 corresponded toTUCLs of 25.0mm, 27.0mmand 29.0mmrespectively. The multiple logistic regression analysis, including maternal age, previous PTB and cervical surgery showed a significant negative association between TUCL and PTB, with an odds ratio (OR) of 0.92 (95% confidence interval [95%CI]: 0.90-0.95; p<0.001). The use of a TUCL of 20mm is the best cut-off, when compared with the 25-mm cut-off, improving the prediction of risk.
Conclusion
The present study showed an inverse association between TUCL and PTB, and that the inclusion of other risk factors like maternal age, previous PTB and cervical surgery can improve the screening algorithm. Furthermore, it emphasizes that the TUCL cut-off that defines short cervix can differ according to the population.
Key-words cervical length cut-offPreterm birthpreterm birth screeningtransvaginal ultrasound cervical lengthSee morePlumX Metrics
- Citations
- Citation Indexes: 2
- Usage
- Full Text Views: 85
- Abstract Views: 20
- Captures
- Readers: 30
-
Original Article06-18-2021
Association between Prenatal Care Adequacy Indexes and Low Birth Weight Outcome
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):256-263
Abstract
Original ArticleAssociation between Prenatal Care Adequacy Indexes and Low Birth Weight Outcome
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):256-263
Views222See moreAbstract
Objective
To investigate the association between prenatal care (PNC) adequacy indexes and the low birth weigth (LBW) outcome.
Methods
A total of 368,093 live term singleton births in the state of Rio de Janeiro (Brazil) from 2015 to 2016 were investigated using data from the Brazilian Live Birth Information System (Sistema de Informações sobre Nascidos Vivos, SINASC, in Portuguese). Seven PNC adequacy indexes were evaluated: four developed by Brazilian authors (Ciari Jr. et al., Coutinho et al., Takeda, and an index developed and used by the Brazilian Ministry of Health – MS) and three by authors from other countries (Kessner et al., the Adequacy of Prenatal Care Utilization index – APNCU, and the Graduated Prenatal Care Utilization Index – GINDEX). Adjusted odds ratios were estimated for the PNC adequacy indexes by means of multivariate logistic regression models using maternal, gestational and newborn characteristics as covariates.
Results
When the PNC is classified as “inadequate”, the adjusted odds ratios to the LBWoutcome increase between 42% and 132%, depending on which adequacy index is evaluated. Younger (15 to 17 years old) and older (35 to 45 years old) mothers, those not married, of black or brown ethnicity, with low schooling (who did not finish Elementary School), primiparous, with preterm births, as well as female newborns had increasing odds for LBW. The models presented areas under the receiver operating characteristic (ROC) curve between 80.4% and 81.0%, and sensitivity and specificity that varied, respectively, between 57.7% and 58.6% and 94.3% and 94.5%.
Conclusion
Considering all PNC adequacy indexes evaluated, the APNCU had the best discriminatory power and the best ability to predict the LBW outcome.
PlumX Metrics
- Citations
- Citation Indexes: 10
- Usage
- Full Text Views: 125
- Abstract Views: 38
- Captures
- Readers: 61
-
Editorial06-18-2021
Provision and Guidance for Postpartum Contraception – Ensuring Reproductive Rights during Times of Crises
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):247-249
Abstract
EditorialProvision and Guidance for Postpartum Contraception – Ensuring Reproductive Rights during Times of Crises
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):247-249
Views186Reproductive choice and access to contraception are basic rights for all women, representing a major step forward in the improvement of gender equality. Sexual and reproductive health is paramount when considering public health, and has been directly affected by the COVID-19 pandemic, since these services suffered a reduction in their capacity for elective care, including […]See more -
Review Article06-02-2021
SARS-CoV-2 Infection and Placental Pathology Infecção por SARS-CoV-2 e patologia placentária
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(6):474-479
Abstract
Review ArticleSARS-CoV-2 Infection and Placental Pathology Infecção por SARS-CoV-2 e patologia placentária
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(6):474-479
Views272See moreAbstract
Placental pathophysiology in SARS-CoV-2 infection can help researchers understand more about the infection and its impact on thematernal/neonatal outcomes. This brief review provides an overview about some aspects of the placental pathology in SARSCoV- 2 infection. In total, 11 papers were included. The current literature suggests that there are no specific histopathological characteristics in the placenta related to SARSCoV- 2 infection, but placentas frominfected women aremore likely to show findings of maternal and/or fetal malperfusion. The most common findings in placentas from infected women were fibrin deposition and intense recruitment of inflammatory infiltrates. The transplacental transmission of this virus is unlikely to occur, probably due to low expression of the receptor for SARS-CoV-2 in placental cell types. Further studies are needed to improve our knowledge about the interaction between the virus and the mother-fetus dyad and the impact on maternal and neonatal/fetal outcomes.
PlumX Metrics
- Citations
- Citation Indexes: 13
- Usage
- Full Text Views: 111
- Abstract Views: 15
- Captures
- Readers: 44
Search
Search in:
Tag Cloud
Pregnancy (252)Breast neoplasms (104)Pregnancy complications (104)Risk factors (103)Menopause (88)Ultrasonography (83)Cesarean section (78)Prenatal care (71)Endometriosis (70)Obesity (61)Infertility (57)Quality of life (55)prenatal diagnosis (51)Women's health (48)Maternal mortality (46)Postpartum period (46)Pregnant women (45)Breast (44)Prevalence (43)Uterine cervical neoplasms (43)