-
Original Article
A new screening of preterm birth in gestation with short cervix after pessary plus progesterone
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo39i
09-06-2024
Summary
Original ArticleA new screening of preterm birth in gestation with short cervix after pessary plus progesterone
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo39i
09-06-2024Views141See moreAbstract
Objective
This study aims to create a new screening for preterm birth < 34 weeks after gestation with a cervical length (CL) ≤ 30 mm, based on clinical, demographic, and sonographic characteristics.
Methods
This is a post hoc analysis of a randomized clinical trial (RCT), which included pregnancies, in middle-gestation, screened with transvaginal ultrasound. After observing inclusion criteria, the patient was invited to compare pessary plus progesterone (PP) versus progesterone only (P) (1:1). The objective was to determine which variables were associated with severe preterm birth using logistic regression (LR). The area under the curve (AUC), sensitivity, specificity, and positive predictive value (PPV) and negative predictive value (NPV) were calculated for both groups after applying LR, with a false positive rate (FPR) set at 10%.
Results
The RCT included 936 patients, 475 in PP and 461 in P. The LR selected: ethnics white, absence of previous curettage, previous preterm birth, singleton gestation, precocious identification of short cervix, CL < 14.7 mm, CL in curve > 21.0 mm. The AUC (CI95%), sensitivity, specificity, PPV, and PNV, with 10% of FPR, were respectively 0.978 (0.961-0.995), 83.4%, 98.1%, 83.4% and 98.1% for PP < 34 weeks; and 0.765 (0.665-0.864), 38.7%, 92.1%, 26.1% and 95.4%, for P < 28 weeks.
Conclusion
Logistic regression can be effective to screen preterm birth < 34 weeks in patients in the PP Group and all pregnancies with CL ≤ 30 mm.
-
Original Article/Infertility
Endometrial Progesterone and Estrogen Receptors in Relation to Hormonal Levels in Women with Unexplained Recurrent Miscarriage
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(11):676-682
12-05-2023
Summary
Original Article/InfertilityEndometrial Progesterone and Estrogen Receptors in Relation to Hormonal Levels in Women with Unexplained Recurrent Miscarriage
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(11):676-682
12-05-2023Views120See moreAbstract
Objective
Recurrent miscarriage has been linked to hormonal disturbance due to dysregulation of its receptors rather than to the availability of the hormone. We aimed to investigate endometrial expression of progesterone and estrogen receptors in relation to serum and endometrial hormonal levels in unexplained recurrent miscarriage.
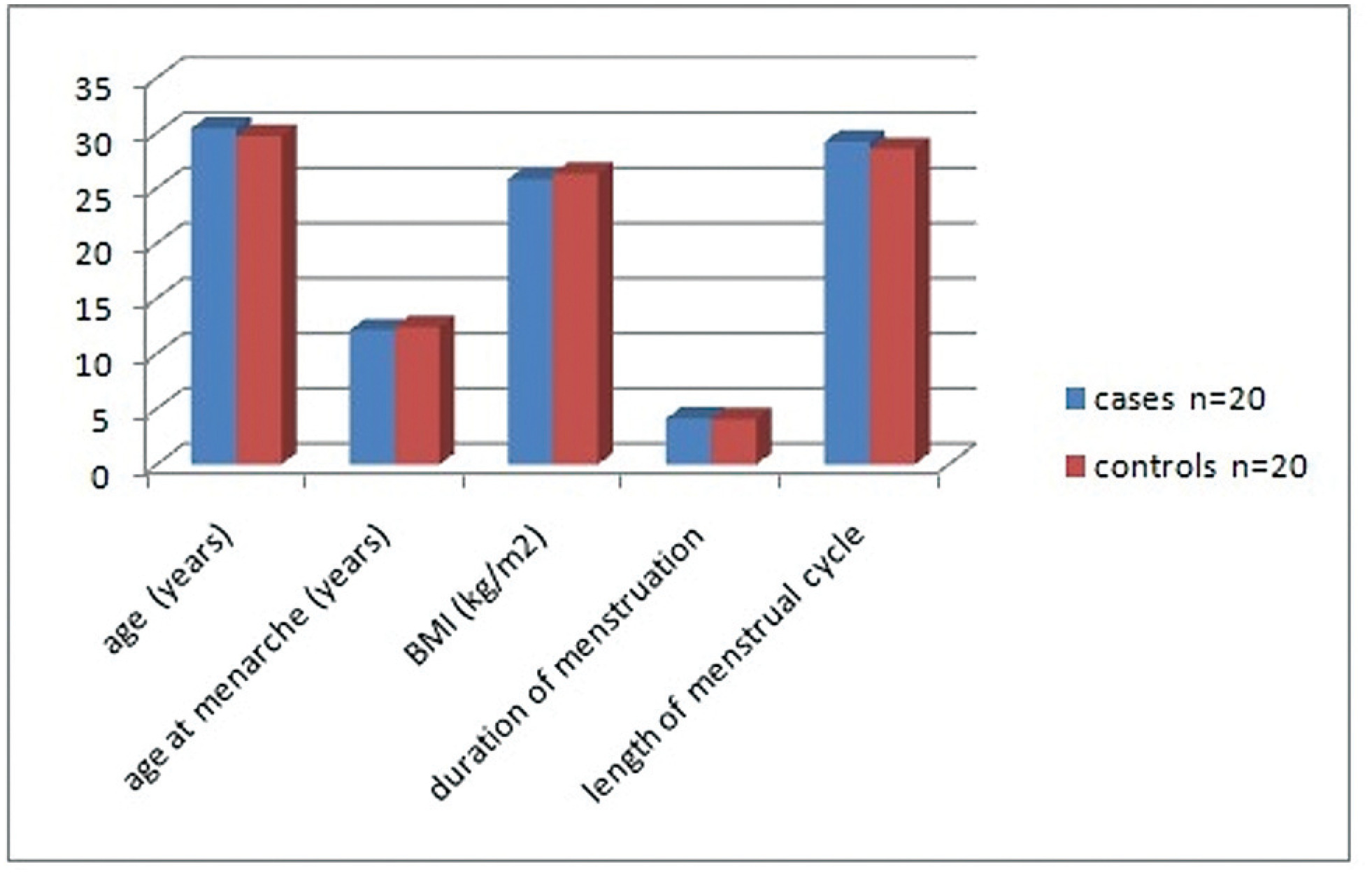
Methods
The present case control study included 20 cases with unexplained recurrent miscarriage and 20 parous women as controls. Ovulation was confirmed using an ovulation kit and 10 to 12 days after detecting the urinary luteinizing hormone surge, all women were subjected to a blood sample and to an endometrial biopsy. Progesterone and estrogen levels were measured in serum and in endometrial tissue and receptor concentrations were in the endometrial sample.
Results
Women with recurrent miscarriage showed significantly lower concentration of receptors in both the cytoplasm and the nucleus of endometrial tissue compared with controls. The nuclear/cytoplasm ratio of progesterone receptor was significantly higher in cases compared with controls, implicating that recurrent miscarriage is probably linked to nongenomic activity of the hormone; this was also significant for estrogen receptor. Serum progesterone and estrogen hormonal levels were comparable between groups while both hormones were significantly reduced in the endometrium of recurrent miscarriage cases. Receptors significantly correlated with endometrial hormonal level but not to serum level.
Conclusion
Recurrent miscarriage might be linked to reduced endometrial progesterone and estrogen receptors and appears to be more related to nongenomic activity of progesterone. Endometrial receptors expression correlates to tissue hormonal level rather than to serum hormonal level.
-
Original Article
Impact of Plasmatic Progesterone on the Day of Frozen Embryo Transfer in Hormone-induced Cycles
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):608-615
09-21-2021
Summary
Original ArticleImpact of Plasmatic Progesterone on the Day of Frozen Embryo Transfer in Hormone-induced Cycles
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):608-615
09-21-2021Views166See moreAbstract
Objective
To establish a relationship between serum progesterone values on the day of frozen blastocyst transfer in hormone-replaced cycles with the probability of pregnancy, miscarriage or delivery.
Methods
This was an ambispective observational study including all frozen-thawed embryo transfer cycles performed at our department following in vitro fecundation from May 2018 to June 2019. The outcomes evaluated were β human chorionic gonadotropin (β-hCG)-positive pregnancy and delivery. Groups were compared according to the level of serum progesterone on the day of embryo transfer: the 1st quartile of progesterone was compared against the other quartiles and then the 2nd and 3rd quartiles against the 4th quartile.
Results
A total of 140 transfers were included in the analysis: 87 with β-HCG>10 IU/L (62%), of which 50 (36%) delivered and 37 had a miscarriage (42%).Women with lower progesterone levels (< 10.7ng/mL) had a trend toward higher β-HCG-positive (72 versus 59%; p>0.05), lower delivery (26 versus 39%; p>0.05) and higher miscarriage rates (64 versus 33%; p<0.01). Comparing the middle quartiles (P25-50) with those above percentiles 75, the rate of pregnancy was similar (60 versus 57%; p>0.05), although there was a trend toward a higher number of deliveries (43 versus 31%; p>0.05) and a lower number of miscarriages (28 versus 45%; p>0.05). These differences were not statistically significant.
Conclusion
There were no differences in pregnancy and delivery rates related with the progesterone level when measured in the transfer day. The miscarriage rate was higher in the 1st quartile group.
-
Original Article
Progesterone’s Serum Level and a New Ultrasonographic Parameter in the First Trimester Pregnancy – Prognostic Factors for Embryonic Demise
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(9):525-530
09-30-2019
Summary
Original ArticleProgesterone’s Serum Level and a New Ultrasonographic Parameter in the First Trimester Pregnancy – Prognostic Factors for Embryonic Demise
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(9):525-530
09-30-2019Views147See moreAbstract
Objective
The etiology of embryonic demise is multifactorial, with chromosomal abnormalities being the most common (40%). The purpose of the present study is to evaluate the correlation between a serum biomarker, progesterone, and an ultrasonographic parameter, the distance between yolk sac and embryo (DYSE) in assessing the prognosis of pregnancy outcome in the 1st trimester.
Methods
The present study is a prospective case-control analysis that includes 2 groups of patients: 81 patients with first-trimester normal evolutive pregnancy and 89 patients with embryonic demise, all of the patients having between 6 and 11 weeks of amenorrhea. Endovaginal ultrasonographic exploration was performed to evaluate the distance between the lower pole of the embryo and the yolk sac. From each subject enrolled in the study, 20ml of blood was collected for progesterone serum level measurement.
Results
Regarding the DYSE in the case group, lower values were observed compared with the control group, the difference being statistically significant. In the statistical analysis of serum progesterone values, statistically significant differences were observed between the 2 groups (p<0.05).
Conclusion
The DYSE has a high positive predictive value in identifying pregnancies with potentially reserved outcome, with the present study demonstrating that a DYSE<3mm causes an unfavorable evolution of the pregnancy. Low serum levels of progesterone are associated with an increased rate of nonviable embryos. The correlation between these two parameters increases the effectiveness of screening methods in prenatal monitoring and improves the diagnostic methods for the firsttrimester pregnancies whose outcome potential can be reserved.
-
Case Report
Autoimmune Progesterone Dermatitis: A Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(3):203-205
05-16-2019
Summary
Case ReportAutoimmune Progesterone Dermatitis: A Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(3):203-205
05-16-2019Views147See moreAbstract
Introduction
Autoimmune progesterone dermatitis (APD) is a rare autoimmune dermatosis characterized by recurrent cutaneous and mucosal lesions during the luteal phase of the menstrual cycle that disappear some days after the menses.
Case
Report A 34-year-old primipara woman with no significant past medical history and no prior exogenous hormone use, who presented with cyclic skin eruptions starting 1 year after the delivery. The lesions occurred 6 days before the menses and disappeared in between 1 and 2 days after the menstruation ceased. The patient was diagnosed after a positive response to an intradermal test with progesterone and was successfully treated with combined oral contraceptives. The skin eruptions have not returned since the initiation of this therapy.
Conclusion
Dermatologists, gynecologists, and obstetricians should be aware of this rare entity. Furthermore, if this condition is suspected, a thorough history taking on the menstrual cycle and results of the intradermal progesterone test are mandatory.
-
Artigos Originais
Regularity of cycles and ovulatory pattern in young women with sickle cell anemia
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(11):525-529
01-20-2010
Summary
Artigos OriginaisRegularity of cycles and ovulatory pattern in young women with sickle cell anemia
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(11):525-529
01-20-2010DOI 10.1590/S0100-72032010001100002
Views100See morePURPOSE: to evaluate the characteristics of the menstrual cycle and to identify the occurrence of ovulation in nulliparous young women with sickle cell anemia (SCA). METHODS: we conducted a case-control study including 26 nulliparous women of reproductive age, divided into two groups: "cases", consisting of 13 women with SCA, and "Control" Group, consisting of 13 healthy women with the same interval since menarche. The characteristics of the menstrual cycle were reported by the participants, who were also submitted to measurements of serum progesterone, basal body temperature curves and transabdominal ultrasound in three consecutive cycles (total: 78 cycles) in order to identify the occurrence of ovulation. The results were compared between groups using the nonparametric Mann-Whitney or Kruskal Wallis tests, and the differences were considered significant when p-value < 0.05. RESULTS: no significant difference was found in mean chronological age between the two groups (p = 0.2) in the pattern of the menstrual cycle when duration of flow (p = 0.4) and interval between cycles (p = 0.3) were compared. There was no difference between groups in age at menarche (p = 0.05). Mean hemoglobin value was 8.4 g/dL (± 0.9) in the group of women with SCA and 12.6 g/dL (± 0.8) in the control group (p < 0.01). The frequency of ovulatory cycles was similar for cases (76.9%) and controls (92.3%) (p = 0.5), with a predominance of individuals with three ovulatory cycles in the control group (84.6%) compared to 23.1% in the case group (p = 0.04). CONCLUSION: the findings justify the need for effective guidance for patients with SCA regarding sexual activity, the possibility of pregnancy and the alternatives for contraception.
-
Artigos Originais
Progesterone receptor gene polymorphism and recurrent spontaneous abortion
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(5):229-233
08-26-2010
Summary
Artigos OriginaisProgesterone receptor gene polymorphism and recurrent spontaneous abortion
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(5):229-233
08-26-2010DOI 10.1590/S0100-72032010000500005
Views121See morePURPOSE: to assess a possible association between polymorphism of the progesterone receptor gene (PROGINS) and recurrent spontaneous abortion (RSA). METHODS: in this case-control study, 85 women with at least three previous spontaneous abortions without an identifiable cause (RSA Group) and 157 women with at least two previous term pregnancies without pathologies and no previous miscarriage (Control Group) were selected. An amount of 10 mL of peripheral blood was collected by venipuncture and genomic DNA was extracted by the DTAB/CTAB method, followed by the polymerase chain reaction (PCR) under specific conditions for this polymorphism and by amplification by 2% agarose gel electrophoresis. The bands were visualized with an ultraviolet light transilluminator and the gels were photographed. Differences in the PROGINS genotype and allele frequencies between groups were analyzed by the χ2 test, with the level of significance set at p<0.05. The Odds Ratio (OR) was also used, with 95% confidence intervals 95%CI. RESULTS: PROGINS genotypic frequencies were 72.3% T1T1 and 27.7% T1T2 for the RSA group and 764% T1T1, 22.3% T1T2 and 1.3% T2T2 for the control group. There were no differecnes between groups when the genotype and allele frequencies were analyzed: respectively p=0.48 (OR: 0.8) and p=0.65 (OR: 0.9). CONCLUSIONS: our results suggest that PROGINS polymorphism is not associated with RSA.
-
Artigos Originais
Modulation by progesterone of pain sensitivity to mechanical and ischemic stimuli in young and healthy women
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(6):306-311
09-04-2008
Summary
Artigos OriginaisModulation by progesterone of pain sensitivity to mechanical and ischemic stimuli in young and healthy women
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(6):306-311
09-04-2008DOI 10.1590/S0100-72032008000600007
Views89See morePURPOSE: to investigate the relationship between pain perception (experimental pain threshold and tolerance, in response to ischemia and pressure) in young and healthy young women and female sexual hormone seric levels (estradiol and progesterone). METHODS: 18 volunteers have participated of this study, during three consecutive menstrual cycles. A pressure algometer and a manual dynamometer have been used to measure painful responses to pressure and ischemia algesic stimuli. Blood has been collected for assessment of both hormonal and painful variables, during three menstrual cycles, whose characterization was based on daily oral temperature record, a diary of the menstrual cycles with the onset and end of each cycle, and on estradiol and progesterone plasmatic levels. The average for the algesic variables measured has been compared by analysis of variance (ANOVA) and the Tukey-Kramer's post-test, among the menstrual cycle phases (follicular, periovulatory, early luteal, late luteal and menstrual). The Pearson's test has been used for correlation analysis between algesic and hormonal variables. Statistical significance has been defined as p<0.05. RESULTS: no significant change in pain parameters among the menstrual cycle phases has been observed. Nevertheless, there have been significant negative correlations between progesterone and ischemic threshold (r=-0.23; p<0.01), and pressure tolerance (r=-0.23; p<0.01) at the early luteal phase. CONCLUSIONS: these results indicate that the increase in progesterone levels correlates with a decrease of ischemic threshold and pressure tolerance, suggesting that progesterone plays a role in the pain modulation during the early luteal phase.


