Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(5):351-356
07-30-2021
Most prenatal screening programs for toxoplasmosis use immunoassays in serum samples of pregnant women. Few studies assess the accuracy of screening tests in dried blood spots, which are of easy collection, storage, and transportation. The goals of the present study are to determine the performance and evaluate the agreement between an immunoassay of dried blood spots and a reference test in the serum of pregnant women from a population-based prenatal screening program for toxoplasmosis in Brazil.
A cross-sectional study was performed to compare the immunoassays Imunoscreen Toxoplasmose IgM and Imunoscreen Toxoplasmose IgG (Mbiolog Diagnósticos, Ltda., Contagem, Minas Gerais, Brazil)in dried blood spots with the enzymelinked fluorescent assay (ELFA, BioMérieux S.A., Lyon, France) reference standard in the serum of pregnant women from Minas Gerais Congenital Toxoplasmosis Control Program.
The dried blood spot test was able to discriminate positive and negative results of pregnant women when comparedwith the reference test, with an accuracy of 98.2% for immunoglobulin G (IgG), and of 95.8% for immunoglobulin M (IgM).
Dried blood samples are easy to collect, store, and transport, and they have a good performance,making this a promisingmethod for prenatal toxoplasmosis screening programs in countries with continental dimensions, limited resources, and a high prevalence of toxoplasmosis, as is the case of Brazil.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(6):442-451
07-27-2021
To determine the adequacy of compliance with antenatal care (ANC) by pregnant women in Peru and to identify the associated factors.
An analytical cross-sectional study of data from the 2019 Peruvian Demographic and Family Health Survey (Encuesta Demográfica y de Salud Familiar, ENDES, in Spanish) was conducted. The dependent variable was adequate compliance with ANC (provided by skilled health care professionals; first ANC visit during the first trimester of pregnancy; six or more ANC visits during pregnancy; ANC visits with appropriate content) by women aged 15 to 49 years in their last delivery within the five years prior to the survey. Crude and adjusted prevalence ratios and their 95% confidence intervals were calculated using a log-binomial regression model.
A total of 18,386 women were analyzed, 35.0% of whom adequately complied with ANC. The lowest proportion of compliance was found with the content of ANC (42.6%). Sociodemographic factors and those related to pregnancy, such as being in the age groups of 20 to 34 years and 35 to 49 years, havingsecondaryor higher education, belonging to a wealth quintile of the population other than the poorest, being from the Amazon region, not being of native ethnicity, having a second or third pregnancy, and having a desired pregnancy, increased the probability of presenting adequate compliance with ANC.
Only 3 out of 10women in Peru showed adequate compliancewith ANC. Compliance with the content of ANC must be improved, and strategies must be developed to increase the proportion of adequate compliance with ANC.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):317-322
06-18-2021
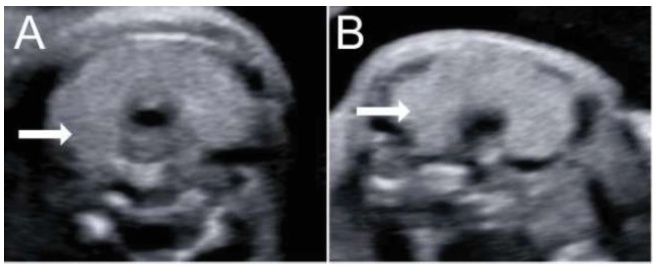
Fetal thyroid complications in pregnancy are uncommon, and are commonly related to the passage of substances through the placenta. The excessive iodine intake during the pregnancy is a well-known mechanism of fetal thyroid enlargement or goiter, and invasive procedures have been proposed for the treatment of fetal thyroid pathologies. In the present report, we demonstrate two cases from different centers of prenatal diagnosis of fetal thyroid enlargement and/or goiter in three fetuses (one pair of twins, wherein both fetuses were affected, and one singleton pregnancy). The anamnesis revealed the ingestion of iodine by the patients, prescribed from inadequate vitamin supplementation. In both cases, the cessation of iodine supplement intake resulted in a marked reduction of the volume of the fetal thyroid glands, demonstrating that conservative treatmentmay be an option in those cases. Also, clinicians must be aware that patients may be exposed to harmful dosages or substances during pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):256-263
06-18-2021
To investigate the association between prenatal care (PNC) adequacy indexes and the low birth weigth (LBW) outcome.
A total of 368,093 live term singleton births in the state of Rio de Janeiro (Brazil) from 2015 to 2016 were investigated using data from the Brazilian Live Birth Information System (Sistema de Informações sobre Nascidos Vivos, SINASC, in Portuguese). Seven PNC adequacy indexes were evaluated: four developed by Brazilian authors (Ciari Jr. et al., Coutinho et al., Takeda, and an index developed and used by the Brazilian Ministry of Health - MS) and three by authors from other countries (Kessner et al., the Adequacy of Prenatal Care Utilization index - APNCU, and the Graduated Prenatal Care Utilization Index - GINDEX). Adjusted odds ratios were estimated for the PNC adequacy indexes by means of multivariate logistic regression models using maternal, gestational and newborn characteristics as covariates.
When the PNC is classified as “inadequate”, the adjusted odds ratios to the LBWoutcome increase between 42% and 132%, depending on which adequacy index is evaluated. Younger (15 to 17 years old) and older (35 to 45 years old) mothers, those not married, of black or brown ethnicity, with low schooling (who did not finish Elementary School), primiparous, with preterm births, as well as female newborns had increasing odds for LBW. The models presented areas under the receiver operating characteristic (ROC) curve between 80.4% and 81.0%, and sensitivity and specificity that varied, respectively, between 57.7% and 58.6% and 94.3% and 94.5%.
Considering all PNC adequacy indexes evaluated, the APNCU had the best discriminatory power and the best ability to predict the LBW outcome.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):420-426
08-26-2020
Since the World Health Organization (WHO) declared coronavirus infection (COVID-19) a Public Health Emergency of International Concern in January 2020, there have been many concerns about pregnant women and the possible effects of this emergency with catastrophic outcomes inmany countries. Information on COVID-19 and pregnancy are scarce and spread throughout a fewcase series, with no more than 50 cases in total. The present review provides a brief analysis of COVID-19, pregnancy in the COVID-19 era, and the effects of COVID-19 on pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(10):597-606
11-07-2019
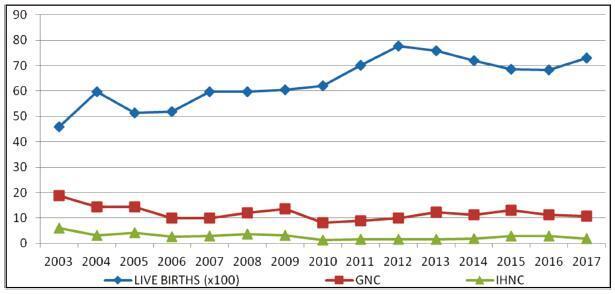
To evaluate conditions associated with stillbirth (SB), and possible trends related with it, in a maternity hospital school in the North zone of São Paulo.
An observational, cross-sectional study conducted at the Hospital Maternidade- escola de Vila Nova Cachoeirinha with 1,139 SBs in the period of 2003 to 2017. Cases of intermediate SB (ISB) (weight between 500 and 999 g) and late SB (LSB) (weight ≥ 1,000 g) were compared. We evaluated clinical data, laboratory tests, and fetal and placental studies. Data were stored in Windows Excel (Microsoft Corp., Redmond, WA, USA) worksheets, according to which graphs and tables were constructed. We used the statistical software SPSS for Windows version 18.0 (SPSS In., Chicago, IL, USA), estimating the prevalence ratio (PR) and odds ratio (OR), considering the 95% confidence interval (95% CI).
The general SB rate was 11.9%, and the in-hospital SB rate was 2.8%. Pregnant women younger than 16 years of age were more likely to have ISB (OR 0.32, 0.15- 0.76), while patients older than 40 years old had a higher chance of LSB (PR 0.85, 0.72- 0.99). A total of 25.7% of the general population did not have prenatal care, and 77.1% of the cases presented fetal death at admission. The cases of ISB had a statistically significant association with home birth (OR 0.61, 0.46-0.80). Cesarean section was performed in 16.1% of the subjects, and misoprostol was the most used method for induction. Necropsy and placental study of the fetuses were performed, respectively, in 94.2% and 97.3% of the cases. Associated causes were not identified in 22.1% of the cases, and the main causes identified were amniotic sac infections (27.9%), fetal malformations (12.5%), placental abruption (11.2%), hypertensive syndromes (8.5%), and maternal syphilis (3.9%), the latter with an increasing trend.
Among the factors associated to SB were: hypertensive syndromes, amniotic sac infections, fetal malformations, placental abruption and syphilis. There was a growing trend in the number of cases of syphilis, which translates an alert. Diagnostic limitations justify indeterminate causes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(8):471-476
08-01-2018
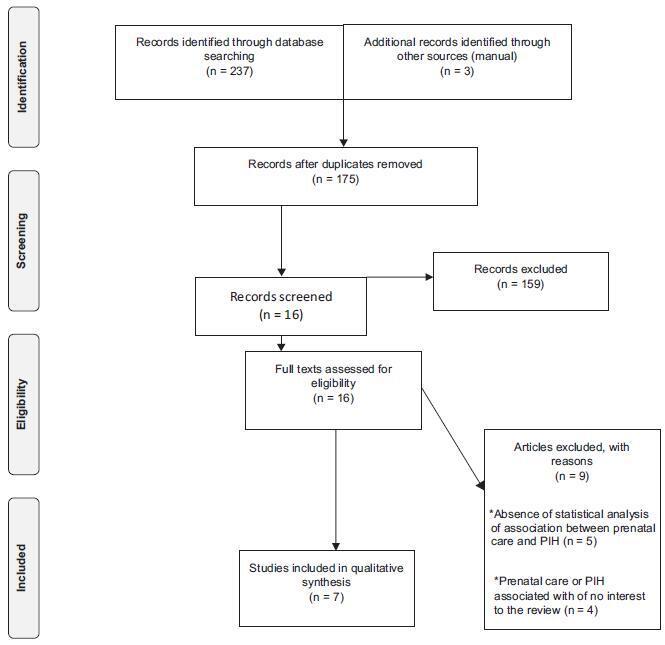
Evaluate the influence of prenatal care on the occurrence of gestational hypertension.
The Web of Science, Scopus, Pubmed, Cochrane and ClinicalTrials electronic databases were searched for articles published between January 1st, 2012 and December 31st, 2016. No language restrictions were imposed. The following keywords were used: prenatal care, medical assistance, prenatal education, pregnancy-induced hypertension. The preferred reporting items for systematic reviews and meta-analyses (PRISMA) checklist was employed. Two hundred and forty articles were identified during the initial search, but only seven met the inclusion criteria. This systematic review is registered with the international prospective register of systematic reviews (PROSPERO; #CRD42017064103).
The seven studies hada lowriskof bias,withmethodological quality scores ranging fromsix to eight points. Five studies found a positive relationship between prenatal care and pregnancy-induced hypertension, whereas two studies found no significant association between the two variables. The divergence among the studies may have been due to the type of healthcare service at which the study was conducted and the sample size.
Although the studies analyzed differed with regard to methodological aspects, the findings demonstrate the importance of prenatal care during the gestational period as a prevention and health promotion measure.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):209-224
04-01-2018
To review the existing recommendations on the prenatal care of women with systemic lupus erythematosus (SLE), based on currently available scientific evidence.
An integrative review was performed by two independent researchers, based on the literature available in the MEDLINE (via PubMed), EMBASE and The Cochrane Library databases, using the medical subject headings (MeSH) terms “systemic lupus erythematosus” AND “high-risk pregnancy” OR “prenatal care.” Studies published in English between 2007 and 2017 were included; experimental studies and case reports were excluded. In cases of disagreement regarding the inclusion of studies, a third senior researcher was consulted. Forty titles were initially identified; four duplicates were excluded. After reading the abstracts, 7 were further excluded and 29 were selected for a full-text evaluation.
Systemic lupus erythematosus flares, preeclampsia, gestation loss, preterm birth, fetal growth restriction and neonatal lupus syndromes (mainly congenital heartblock) were the major complications described. The multidisciplinary team should adopt a specific monitoring, with particular therapeutic protocols. There are safe and effective drug options that should be prescribed for a good control of SLE activity.
Pregnant women with SLE present an increased risk for maternal complications, pregnancy loss and other adverse outcomes. The disease activity may worsen and, thereby, increase the risk of other maternal-fetal complications. Thus, maintaining an adequate control of disease activity and treating flares quickly should be a central goal during prenatal care.