Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(1):40-46
DOI 10.1590/S0100-72032012000100008
PURPOSE: To determine the frequency and the association of serum markers for inherited and acquired thrombophilias in pregnant women with a history of severe pre-eclampsia in previous pregnancies. METHODS: Case-control study consisting of 81 pregnant women with a history of severe pre-eclampsia in previous pregnancies (study group) and 32 women with no history of severe pre-eclampsia in previous pregnancies (control group). The presence of inherited thrombophilia and antiphospholipid antibodies was screened in both groups. We used the chi-square test with Yates correction to assess associations and calculate the relative risks. RESULTS: The presence of thrombophilia was detected in 60.0% of patients with a previous history of pre-eclampsia and in 6.0% of the control patients. A significant association was found between pre-eclampsia in a previous pregnancy and the presence of markers for hereditary thrombophilia/antiphospholipid antibodies (p<0.05). The relative risk to develop pre-eclampsia was found to be 1.57 (1.34
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(12):421-425
DOI 10.1590/S0100-72032011001200008
Placenta vascular lesions are a group of distinct yet related entities that include chorangiomas and diffuse multifocal chorangiomatosis. Chorangioma is an expansive nodular lesion with an incidence of about 1%. Diffuse multifocal chorangiomatosis is rare (0.2%) and mostly seen in placentas before the 32nd gestational week. The authors present a case of a monochorionic/biamniotic twin pregnancy, in which, at the 26th gestational week, one fetus developed intrauterine growth restriction (IUGR), hydrops, and anemia associated with a tumor of the placenta with increased vascularization in the Doppler study. Pathological examination of the placenta diagnosed diffuse multifocal chorangiomatosis. This rare case report of diffuse multifocal chorangiomatosis with prenatal manifestations resembling those of a chorangioma proves that prenatal ultrasound detection of a placenta tumor, with increased vascularization at Doppler study, must raise other diagnostic possibilities beside chorangioma.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):367-375
DOI 10.1590/S0100-72032011001100008
Preeclampsia, which affects about 3 to 5% of pregnant women, is the most frequent medical complication in pregnancy and the most important cause of maternal and perinatal morbidity and mortality. During the past three decades, numerous clinical, biophysical, and biochemical screening tests have been proposed for the early detection of preeclampsia. Literature shows large discrepancies in the sensitivity and predictive value of several of these tests. No single screening test used for preeclampsia prediction has gained widespread acceptance into clinical practice. Instead, its value seems to be in increasing the predictive value of panels of tests, which include other clinical measurements. The aim of this review was to examine the combination of maternal risk factors, mean arterial blood pressure, and uterine artery Doppler, together with biomarkers in the preeclampsia prediction.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(7):158-163
DOI 10.1590/S0100-72032011000700007
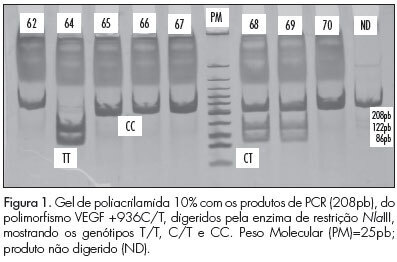
PURPOSE: To identify genetic polymorphisms of endothelial growth factor (VEGF), positions +936C/T and -2578C/A, in women with pre-eclampsia. METHODS: This was a cross-sectional study conducted on 80 women divided into two groups: pre-eclampsia and control. The sample was characterized using a pre-structured interview and data transcribed from the medical records. DNA extraction, amplification of sequences by the Polymerase Chain Reaction (PCR) with specific primers and polymorphism analysis of Restriction Fragment Length Polymorphism (RFLP) were performed to identify polymorphisms. The statistical analysis was performedin a descriptive manner and using the ![]() test. The multiple logistic regression model was used to determine the effect of polymorphisms on pre-eclampsia. RESULTS:Ahigher frequency of the T allele of theVEGF +936C/T polymorphism was observedin patients with pre-eclampsia, but with no significant difference. The presence of allele A of the VEGF -2578C/A was significantly higher in the control group. CONCLUSIONS:No significant association was observed between VEGF +936C/Tpolymorphism andpre-eclampsia. For the VEGF -2578C/A polymorphism a significant differencewas observed between thecontrol and pre-eclampsia group, with allele A being the most frequent in the control, suggesting the possibility that carriers of allele A have lower susceptibility to the development of pre-eclampsia.
test. The multiple logistic regression model was used to determine the effect of polymorphisms on pre-eclampsia. RESULTS:Ahigher frequency of the T allele of theVEGF +936C/T polymorphism was observedin patients with pre-eclampsia, but with no significant difference. The presence of allele A of the VEGF -2578C/A was significantly higher in the control group. CONCLUSIONS:No significant association was observed between VEGF +936C/Tpolymorphism andpre-eclampsia. For the VEGF -2578C/A polymorphism a significant differencewas observed between thecontrol and pre-eclampsia group, with allele A being the most frequent in the control, suggesting the possibility that carriers of allele A have lower susceptibility to the development of pre-eclampsia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(4):157-163
DOI 10.1590/S0100-72032011000400002
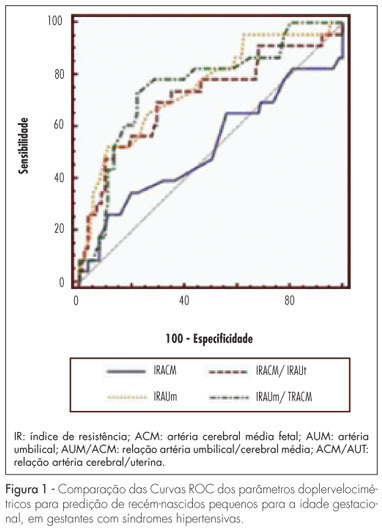
PURPOSE: to determine the best Doppler flow velocimetry index to predict small infants for gestational age (SGAI), in pregnant women with hypertensive syndromes. METHODS: a cross-sectional study was conducted enrolling 129 women with high blood pressure, submitted to dopplervelocimetry up to 15 days before delivery. Women with multiple fetuses, fetal malformations, genital bleeding, placental abruption, premature rupture of fetal membranes, smoking, use of illicit drugs, and chronic diseases were excluded. A receiver operating characteristic (ROC) curve for each Doppler variable was constructed to diagnose SGAI and the sensitivity (Se), specificity (Sp), positive (PLR) and negative (NLR) likelihood ratio were calculated. RESULTS: the area under the ROC curve for the middle cerebral artery resistance index was 52% (p=0.79) with Se, Sp, PLR, and NLR of 25.0, 89.1, 2.3 and 0.84% for a resistance index lower than 0.70, respectively. While the area under the ROC curve for the resistance index of the umbilical artery was 74% (p=0.0001), with Se=50.0%, Sp=90.0%, PLR=5.0 and NLR=0.56, for a resistance index higher or equal to 0.70. The area under the ROC curve for the resistance index umbilical artery/middle cerebral artery ratio was 75% (p=0.0001). When it was higher than 0.86, the Se, Sp, PLR and NLR were 70.8, 80.0, 3.4 and 0.36%, respectively. For the resistance index of the middle cerebral artery/uterine artery ratio, the area under the ROC curve was 71% (p=0.0001). We found a Se=52.2%, Sp=85.9%, PLR=3.7 and NLR=0.56, when the ratio was lower than 1.05. When we compared the area under the ROC curve of the four dopplervelocimetry indexes, we observed that only the resistance index umbilical artery/middle cerebral artery, resistance index middle cerebral artery/uterine artery and resistance index umbilical artery ratios seem to be useful for the prediction of SGA. CONCLUSION: in patients with high blood pressure during pregnancy, all dopplervelocimetry parameters, except the middle cerebral artery resistance index, can be used to predict SGAI. The umbilical artery/middle cerebral artery ratio seems to be the most recommended one.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(1):49-57
DOI 10.1590/S0100-72032011000100008
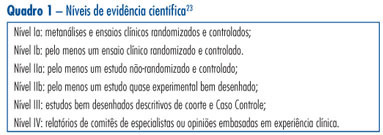
This is a traditional (narrative) review with the objective of highlighting the contribution of obstetric ultrasonography (US) between the 11th and 14th week of pregnancy, commonly called first trimester anomaly scan. In addition to being used for the screening of chromosomal anomalies, US can be employed during this period to confirm or determine gestational age, evaluate fetal anatomy, diagnose malformations, screen major structural abnormalities and genetic syndromes, define the prognosis of pregnancy, diagnose and characterize multiple pregnancies, and screen preeclampsia and intrauterine growth restriction. The most important studies about this subject published between 1990 and 2010 in the Cochrane and PubMed libraries were included. The selected studies can be classified with scientific levels I to III.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(9):459-468
DOI 10.1590/S0100-72032010000900008
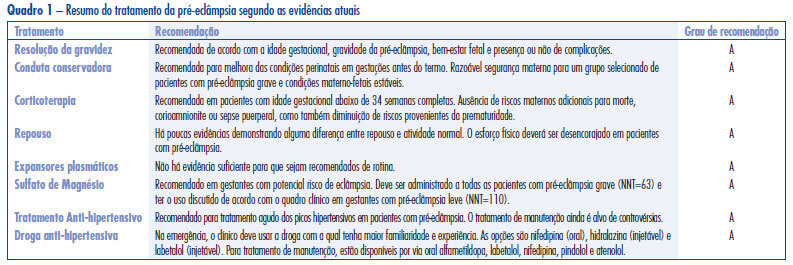
Hypertensive disorders in pregnancy deserve special attention in the setting of global public health. Currently, they represent the third cause of maternal mortality in the world and first in Brazil. From a practical standpoint, pre-eclampsia remains a syndrome that leads to serious repercussions on maternal and fetal mortality and its etiology is not well known. Currently, the best treatment for forms of pre-eclampsia is being discussed at different times in pregnancy and puerperium, with the objective to reduce the high rates of maternal and fetal morbidity and mortality. Considering the pathophysiology of the event, anticipation of delivery is the best treatment for pre-eclampsia. The use of magnesium sulfate is recommended in all cases of severe pre-eclampsia and eclampsia for prevention and treatment of seizures. Likewise, treatment of hypertensive crises is recommended. Hydralazine, nifedipine and labetalol have been the most commonly used drugs for this purpose, but their use depends on the familiarity of the treating physician. Antenatal corticoid therapy is indicated whenever there is an imminent risk of preterm delivery between 24 and 34 weeks. In contrast, there is insufficient evidence to recommend bed rest and routine plasma volume expansion, and there is an urgent need for randomized clinical trials to determine whether maintenance antihypertensive treatment in pregnant women has benefits or risks for mothers and fetuses in all clinical forms of disease, particularly in cases of pure pre-eclampsia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(8):398-404
DOI 10.1590/S0100-72032010000800007
PURPOSE: to evaluate the characteristics regarding care of Bolivian pregnant women and their outcomes in Hospital Municipal Vereador José Storopolli. METHODS: a cross-sectional retrospective case-control study comparing two groups of pregnant women from 2003 to 2007. The Study Group included 312 Bolivian pregnant women and the Control Group, 314 Brazilian women. The groups were compared with respect to demographic variables, the presence of maternal complications and perinatal outcomes. Statistical analysis was performed by χ2 test and, when necessary, by applying Yates' correction. RESULTS: compared to Brazilian mothers, a smaller number of Bolivian women received prenatal care (16.4 versus 5.1%, p<0.001) and among those that did, the percentage of those who had less than five visits was higher (50 versus 19.3%, p<0.001). Compared to the Brazilian group, the Bolivian group had fewer unwed mothers (12.1 versus 25.4%, p<0.001) and a lower number of nulliparous women (34.1 versus 43.6%, p=0.017). Congenital syphilis had a higher incidence in the Bolivian group (2.9 versus 0.5%, p<0.05), as well as a higher number of newborns classified as large for gestational age (14.6 versus 5.8%, p <0.001). CONCLUSIONS: the failure to attend prenatal care or its completion with an inadequate number of consultations, and the higher number of cases of congenital syphilis observed among the Bolivian women show the great vulnerability of this ethnic minority group to health problems. Consequently, it is necessary a strategic planning of the sectors responsible for coordinating assistance in our country, in order to reduce this disparity, either through socio-economic improvements or by the implementation of health care tailored to the needs of this group.