Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(11):566-573
DOI 10.1590/S0100-72032009001100007
PURPOSE: to identify the profile, tendency and causes of maternal death by pre-eclampsia/eclampsia in Paraná. METHODS: descriptive, transversal cohort study on maternal death by pre-eclampsia/eclampsia from 1997 to 2005. Data were obtained from case studies prepared by Maternal Death Committees that employ the Reproductive Age Mortality Survey Method to examine all the cases of death among women in fertile age. The general and specific maternal death rate (MDR) by pre-eclampsia/eclampsia were considered. To evaluate the tendency, triennial periods have been compared, two by two, taking into consideration the MDR of each period (p<0.05). In the triennial period from 2003 to 2005, 56 deaths by pre-eclampsia/eclampsia were analyzed. The variables focused were: age, income, schooling, gestation number and complications, pre-natal conditions, signs and symptoms related to the condition, delivery route, the time gestation was interrupted, the newborn conditions, access and treatment, ability to avoid and prevention measures. RESULTS: the general triennial MDR has presented significant decline, with 64.3/100,000 born-alive babies. There has been stability along the period for MDR by hypertensive disorder, with MDR of 11.8/100,000 born-alive. Primiparous women, women over 40 and with low socio-economical status have presented higher risks. In relation to the treatment, there has been underuse or inadequate use of conventional medicines for severe pre-eclampsia and eclampsia. The committees' analysis indicated that all the maternal death due to these conditions could have been avoided. CONCLUSIONS: actions aiming at minimizing the set of causes that lead to death by pre-eclampsia in Paraná should be enforced, including the training and monitoring of health professionals in order to apply the treatment protocols, besides the formalization of a reference net of clinics and hospitals, qualified for the care of high risk pregnancy and its intercurrences, to which pre-natal pregnant women are enrolled.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(2):82-88
DOI 10.1590/S0100-72032009000200006
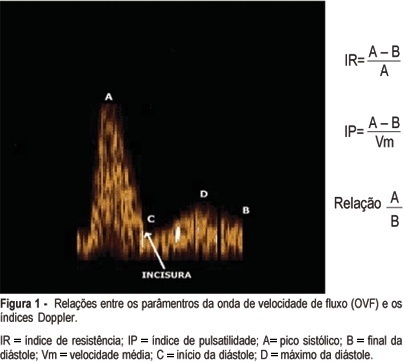
PURPOSE: to evaluate the effect of magnesium sulphate on the pulsatility index (PI) of the uterine, umbilical and fetal middle cerebral arteries, according to the persistency or not of the bilateral protodiastolic notch of the uterine arteries in severe pre-eclampsia. METHODS: a cohort study including 40 pregnant women with severe pre-eclampsia, 23 of them presenting bilateral protodiastolic notch, and 17, unilateral/absent notch. The patients were submitted to Doppler velocimetry before and 20 minutes after the intravenous administration of 6 g of magnesium sulphate. The examination was carried out with the patient in semi-Fowler position, the sonograms being obtained during fetal inactivity, in apnea and absent uterine contraction periods. All the exams were performed by two researchers, the average being considered as the final result. Wilcoxon's test was used to compare the PI, before and after magnesium sulphate in both groups. The difference between the two measurements (before and after magnesium sulphate) was compared between the groups (bilateral incision and unilateral/absent incision) using the Mann-Whitney test. RESULTS: there was a significant increase in the maternal heart rate (MHR) and decrease in the maternal blood pressure, and in the PI medians of the two uterine arteries and in the fetal middle cerebral artery, after magnesium sulphate in both groups. There was a significant decrease in the PI of the left uterine artery and in the umbilical artery, only in the protodiastolic unilateral/absent notch group. Nevertheless, it was not found any significant difference regarding the PI of the right uterine artery, or the cerebral/umbilical relationship, before and after magnesium sulphate in each group. No difference between the groups was found, before and after magnesium sulphate, for any of the studied outcomes. CONCLUSIONS: after the intravenous administration of 6 g of magnesium sulphate to patients with severe pre-eclampsia, a decrease in blood pressure and in the PI of the uterine, umbilical and fetal middle cerebral arteries occurs, besides the increase in the MHR, not influenced by the presence of bilateral protodiastolic notch in the uterine arteries.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(8):406-412
DOI 10.1590/S0100-72032008000800006
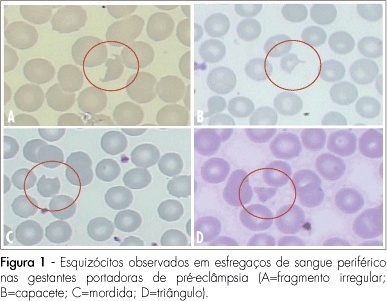
PURPOSE: to evaluate the significance of schizocytes presence in peripheral blood smear of pregnant women with pre-eclampsia, identifying and correlating them with other markers of hemolysis and of the disease severity. METHODS: Seventh six glass slides of peripheral blood smear of pregnant women with pre-eclampsia have been evaluated. After the smear, the slides have been stained with Leishman's dye and stored till they were examined with a Leica, model DLMB microscope, provided with the Qwin Lite 2.5 software that made it possible to record the images of selected fields in CD-ROM. Ten fields with approximately 100 erythrocytes were counted in each glass slide. Schizocytes (irregular fragment or helmet-shaped, bite-shaped or triangular) were considered as present, when their percentage was equal or higher than 0.2%, their presence being correlated with other hemolysis markers (hemoglobin, total bilirubin, lactic desidrogenasis and reticulocytes), pre-eclampsia markers (proteinuria and platelet number). The Statistical Package in Social Science for Windows (SPSS), 10.0 version has been used for statistical analysis, at p<0.05. RESULTS: schizocytes have been present in 31.6% of the pregnant women with pre-eclampsia. In most (75%) of the blood smears there have been three or four schizocytes. There has been no correlation between schizocyte presence and any other hemolysis marker, any pre-eclampsia marker or disease severity. CONCLUSIONS: schizocytes have been identified in a small number and in less than a third of the pregnant women with pre-eclampsia. There has been no correlation with other hemolysis marker parameters or with the disease severity. This way, the presence of schizocytes is not a marker of the clinical evolution of pre-eclampsia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(2):80-86
DOI 10.1590/S0100-72032008000200006
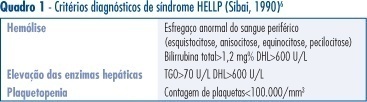
PURPOSE: to describe the clinical and laboratorial profile of HELLP syndrome patients admitted at an Obstetric Intensive Care Unit (ICU) and included in a randomized clinical trial to evaluate the efficacy of dexamethasone in this clinical setting. METHODS: the present study is a secondary analysis of a randomized clinical trial design to evaluate the efficacy of dexamethasone in patients with HELLP syndrome. This sample of patients was composed of patients in the puerperium, with the diagnosis of HELLP syndrome (diagnosis made before or after delivery) who were not chronic corticosteroid users and not carriers of any chronic disease which could modify HELLP syndrome's laboratorial parameters. Patients who were too critical or whose condition did not allow them to consent to participate were not included. Data were extracted from the records used in the randomized clinical trial. Age, parity, gestational age at admission and delivery, time of diagnosis (before or after delivery), HELLP syndrome classification (partial or complete), arterial blood pressure, and diuresis at admission were considered for analysis. Among laboratorial findings, hemoglobin, platelet count, liver enzymes, LDH, and serum bilirubin were analyzed. Complications presented by the patients were also analyzed as well as need of blood transfusions and duration of hospitalization. Analysis was made by the Epi-Info 3.3.2 program. RESULTS: one hundred and five patients were analyzed. Age varied from 14 to 49 years (means of 26.7). Regarding parity, 56 patients (53.8%) were primiparas. Analyzing the timing of the diagnosis, 47 patients (45.2%) had the diagnosis before delivery. The mean gestational age in these patients was 32.4 weeks. Hemorrhagic manifestations were observed in 36 patients (34.3%), oliguria was present in 49 patients (46.7%) and criteria for acute renal failure were seen in 21 (20%) of the cases. Hemotransfusions were necessary in 35 (33.3%) patients. Seven patients (6.7%) had pulmonary edema and four patients died, corresponding to 3.8% of the cases. The mean time from diagnosis of HELLP syndrome to discharge or death was 10.3 days, varying from 1 to 33 days. CONCLUSIONS: HELLP syndrome is an ominous diagnosis, which implicates in elevated maternal morbimortality. Among complications, oliguria and hemorrhagic manifestations were the most common findings and hemotransfusions were frequently required. Lethality reached 3.8%.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(11):561-567
DOI 10.1590/S0100-72032007001100003
PURPOSE: to verify the association of abortion, recurrent fetal loss, miscarriage and severe pre-eclampsia with the presence of hereditary thrombophilias and antiphospholipid antibodies in pregnant women. METHODS: observational and transverse study of 48 pregnant women with past medical record of miscarriage, repeated abortion and fetal loss story (AB Group) and severe pre-eclampsia (PE Group), attended to in the High Risk Pregnancy Ambulatory of the Faculdade de Medicina (Famed) from the Universidade Federal de Mato Grosso do Sul (UFMS) from November 2006 to July 2007. The pregnant women of both groups were screened for the presence of antiphospholipid antibodies (anticardiolipin IgG and IgM, lupic anticoagulant and anti-beta2-glycoprotein I) and hereditary thrombophilias (protein C and S deficiency, antithrombin deficiency, hyperhomocysteinemia and factor V Leiden mutation). The laboratorial screening was performed during the pregnancy. The parametric data (maternal age and parity) were analyzed with Student’s tau test. The non-parametric data (presence/absence of hereditary thrombophilias and antiphospholipid antibodies, presence/absence of pre-eclampsia, fetal loss, miscarriage and repeated abortion) were analyzed with Fisher’s exact test in contingency tables. It was considered significant the association with p value <0.05. RESULTS: out of the 48 pregnant women, 31 (65%) were included in AB Group and 17 (35%) in PE Group. There was no significant difference between maternal age and parity within the groups. There was significant statistical association between recurrent fetal loss, recurrent abortions and previous miscarriages and maternal hereditary thrombophilias (p<0.05). There was no statistical association between the AB Group and the presence of antiphospholipid antibodies. Neither there were associations of the PE Group with maternal hereditary thrombophilias and the presence of antiphospholipid antibodies. CONCLUSIONS: the data obtained suggest routine laboratorial investigation for hereditary thrombophilias in pregnant women with previous obstetrical story of recurrent fetal loss, repeated abortion and miscarriage.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(8):446-452
DOI 10.1590/S0100-72032006000800002
PURPOSE: to describe the obstetric outcomes in pregnant adolescents at a tertiary hospital and to compare the maternal and labor outcomes between precocious and late adolescents. METHODS: in a transversal analytical study, 2058 cases were evaluated, considering 322 (15.65%) from the precocious group and 1736 (84.35%) from the late group that delivered at the "Maternidade Escola Assis Chateaubriand/UFC" from January 1, 2000 to December 31, 2000. The clinical complications in the prenatal period, kind of delivery, indications for cesarean section, birth gestational age at birth, birth weight, comparison of birth weight and gestational age, Apgar score at the first and fifth minute, presence of malformations, and neonatal death were analyzed. The exact Fisher and the chi2 tests were used to compare both groups. The prevalence ratio was calculated. RESULTS: from of total of deliveries, 25.95% belonged to adolescents. The average age was 17.19 years. Prenatal visits were made by 88% of the patients, but 60% had an insufficient number of visits. The most frequent clinical situations were preeclampsia (14.72%), anemia (12.97%) and urinary tract infections (6.37%), with no statistical difference between the groups. Thirty-one and three percent of the births were by cesarean section, preeclampsia being the main indication in the two age groups (25 and 23%, respectively). The frequency of an Apgar score less than 7 at the first minute was 19,9% in the precocious adolescent group and 14,2% in the late adolescent group (x²=6,96, p=0.008). There was no statistical difference regarding prematurity rate (20.2 vs 16.1%), low-birth weight infants (12.4 vs 10.4%), low Apgar score at the fifth minute (5.3 vs 3.3%), congenital malformations (3.1 vs 2.7%), and neonatal death (5.3 vs 3.3%). CONCLUSIONS: the precocious and late pregnant adolescents presented similar pregnancy evolution and obstetric outcomes, except for the differences of the first minute Apgar scores.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(6):323-330
DOI 10.1590/S0100-72032005000600006
PURPOSE: to determine the validity of uterine artery Doppler velocimetry for the prediction of pregnancy complications in a population of low-risk nulliparae. SUBJECTS: a prospective study was conducted on 45 patients in their first pregnancy with no history of chronic diseases. Uterine artery Doppler velocimetry was performed between 24 and 26 weeks, with the determination of resistance index (RI), pulsatility index (PI), S/D ratio, and the presence or absence of incisure in the flow velocity wave. Data were analyzed by the Mann-Whitney test for non-parametric samples, and the Fisher exact test was used in the evaluation of the qualitative parameters. RESULTS: pregnancy complications were observed in twelve patients, with four cases of preeclampsia, one case of small for gestational age newborn (SGA NB), one case of SGA NB + preterm delivery (PTD), three cases of PTD, one case of fetal centralization, and two cases of presence of thick meconium in the amniotic fluid at the time of pregnancy resolution. We noted that RI (median 0.56 x 0.68), PI (median 0.98 x 1.29) and S/D ratio (median 2.2 x 2.9) were higher at the examination performed between 24 and 26 weeks in patients with complications and did not differ in preeclampsia and SGA cases. The presence of bilateral incisure showed 100 and 90% sensitivity, 60.2 and 62.5% specificity, 29.4 and 42,9% positive predictive value (PPV), and 100 and 95.2% negative predictive value (NPV) for the detection of preeclampsia or SGA and of any complication of pregnancy, respectively. An altered Doppler showed 83.3 and 83.3% sensitivity, 69.7 and 69.7% specificity, 33.3 and 50.0% PPV, and 95.8 and 92.0% NPV for the detection of preeclampsia or SGA and of any complication of pregnancy, respectively. CONCLUSION: high impedance indices and the presence of a bilateral incisure in the uterine arteries between 24 and 26 weeks of pregnancy seem to be good predictors of pregnancy and perinatal complications.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(6):316-322
DOI 10.1590/S0100-72032005000600005
PURPOSE: to evaluate the relationship between renal transplantation and pregnancy through the analysis of clinical and obstetric intercurrent events and perinatal outcomes. METHODS: a retrospective series of 39 cases of pregnancy in 37 women with renal transplantation from January 1997 to December 2003 was evaluated. A control group consisted of 66 pregnant women with no previous clinical pathologies. This group received prenatal care and these patients delivered during 2002 and 2003. Preeclampsia, premature rupture of membranes, premature delivery, and intrauterine growth restriction were used to compare these variables. Demographic characteristics of these groups were related to the mean age at conception, ethnic characteristics and obstetric past. Regarding renal transplantation the type of donator and used immunosuppressive drugs were evaluated. The studied clinical variables were chronic hypertension, anemia and urinary tract infection. The interval between the surgery and conception, occurrence of dysfunction, rejection and loss of the allograft were characteristcs related to the allograft. Obstetric variables were related to the type of delivery, incidence of preeclampsia and premature rupture of membranes. Perinatal outcomes were premature delivery and intrauterine growth restriction and these results were compared with renal function. The used statistical methods were the chi2 and Fisher's exact tests. The significance level was fixed always as less than or equal to 0.05 (5%). RESULTS: the mean age at conception was 27 years. The live donator was the most frequent among the patients. Among the immunosuppressive drugs, cyclosporine was the most used. Chronic hypertension occurred in 82% of the cases, anemia in 77% and urinary tract infection in 38.5%. The incidence of renal dysfunction was 47.4% and preeclampsia was the main cause. The loss of the renal transplantation occurred in 10.2%. Delivery by cesarean section was performed in 53.8% of the patients, and the main causes were hypertensive syndromes. Preeclampsia occurred in 28.2%. Among the perinatal outcomes, premature delivery occurred in 46.1% of the cases, with a significant relation to creatinine level greater than or equal to 1.5 mg/dL at the start of prenatal care. Another observed intercurrent event was intrauterine growth restriction, which occurred in 41.0%, and here we found no relation between this event and creatinine levels. CONCLUSIONS: young patients constituted the study group. Chronic hypertension, anemia and urinary tract infection were very common. Renal dysfunction was frequent and must be investigated during prenatal care. There were four cases of loss of the transplant due to clinical or obstetric causes. Cesarean delivery had the highest incidence, but vaginal delivery should be the first choice in these cases. Preeclampsia occurred very frequently and this complication should be considered as a high risk. Preterm delivery and intrauterine growth restriction were the main perinatal complications. Premature deliveries before 37 weeks of gestation were related to allograft function.