-
Original Article
Outcomes after elevation of serratus anterior fascia flap versus serratus muscle flap in direct-to-implant breast reconstruction following mastectomy: a prospective study
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo13
00-00-2024
Summary
Original ArticleOutcomes after elevation of serratus anterior fascia flap versus serratus muscle flap in direct-to-implant breast reconstruction following mastectomy: a prospective study
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo13
00-00-2024Views349Abstract
Objective:
The purpose of this study was to compare postoperative pain between SF flap and serratus anterior muscle (SM) in direct-to-implant breast reconstruction.
Methods:
This is a prospective cohort study that included 53 women diagnosed with breast cancer who underwent mastectomy and one-stage implant-based breast reconstruction from January 2020 to March 2021. Twenty-nine patients (54.7%) had SF elevation, and 24 patients (45.3%) underwent SM elevation. We evaluated patient-reported early postoperative pain on the first day after surgery. Also, it was reported that all surgical complications in the first month and patient reported outcomes (PROs) were measured with the BRECON 23 questionnaire.
Results:
The serratus fascia group used implants with larger volumes, 407.6 ± 98.9 cc (p < 0.01). There was no significant difference between the fascial and muscular groups regarding the postoperative pain score reported by the patients (2 versus 3; p = 0.30). Also, there was no difference between the groups regarding early surgical complications and PROs after breast reconstruction.
Conclusion:
The use of SF seems to cause less morbidity, which makes the technique an alternative to be considered in breast reconstruction. Although there was no statistical difference in postoperative pain scores between the fascia and serratus muscle groups.
Key-words Breast implantsBreast neoplasmsbreast reconstructionFasciaMastectomyPainPostoperative periodSee more -
Original Article
Translation, cross-cultural adaptation to Brazilian Portuguese and measurement properties of the WaLIDD score
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo16
00-00-2024
Summary
Original ArticleTranslation, cross-cultural adaptation to Brazilian Portuguese and measurement properties of the WaLIDD score
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo16
00-00-2024Views396See moreAbstract
Objective:
Dysmenorrhea is the pain related to menstruation; to screen for the symptoms, a working ability, location, intensity of days of pain, and dysmenorrhea (WaLIDD) score was created. The purpose of this work was to culturally adapt and assess the measurement properties of the WaLIDD score for dysmenorrhea in Brazilian women.
Methods:
In this cross-sectional online study, we evaluated women with and without dysmenorrhea. Criterion validity and construct validity were assessed, respectively, by the Receiver Operator Characteristic (ROC) curve and correlations with the bodily pain and social functioning domains of medical outcomes study 36-item short-form health survey (SF-36), self-report of absenteeism and Stanford Presenteeism Scale for presenteeism. Test-retest reliability and measurement errors were assessed, respectively, by intraclass correlation coefficient (ICC) and Bland and Altman Graph.
Results:
430 women completed the test, 238 (55.4%) women had dysmenorrhea, and 199 (46.3%) answered the questionnaire twice for the retest. The cutoff points ≥4, ≥5, and ≥5 could discriminate between women with and without dysmenorrhea, absenteeism, and presenteeism related to dysmenorrhea, respectively. Correlations between SF-36 – pain and social functioning domains and WaLIDD score were weak to strong and negative. For WaLIDD total Score, ICC was 0.95 and the limits of agreement were −1.54 and 1.62.
Conclusion:
WaLIDD score is a short, valid and reliable instrument to screen and predict dysmenorrhea and could predict absenteeism and presenteeism related to dysmenorrhea in Brazilian women.
-
Review Article
Effect of Lubricant Use on Cervicovaginal Cytology – What’s the Evidence?
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(11):724-728
12-05-2023
Summary
Review ArticleEffect of Lubricant Use on Cervicovaginal Cytology – What’s the Evidence?
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(11):724-728
12-05-2023Views120See moreAbstract
Objective
To determine if the use of lubricating gel on the speculum during the cervicovaginal cytology examination interferes with the results obtained, as well as whether it reduces reported discomfort in patients.
Data sources
A systematic review was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations, with a search in the Pubmed/Medline, Scielo, Cochrane Library, Embase databases of articles published between January 2011 and May 2022. The keywords used were cytology, speculum, lubricant, result, and pain.
Selection of studies
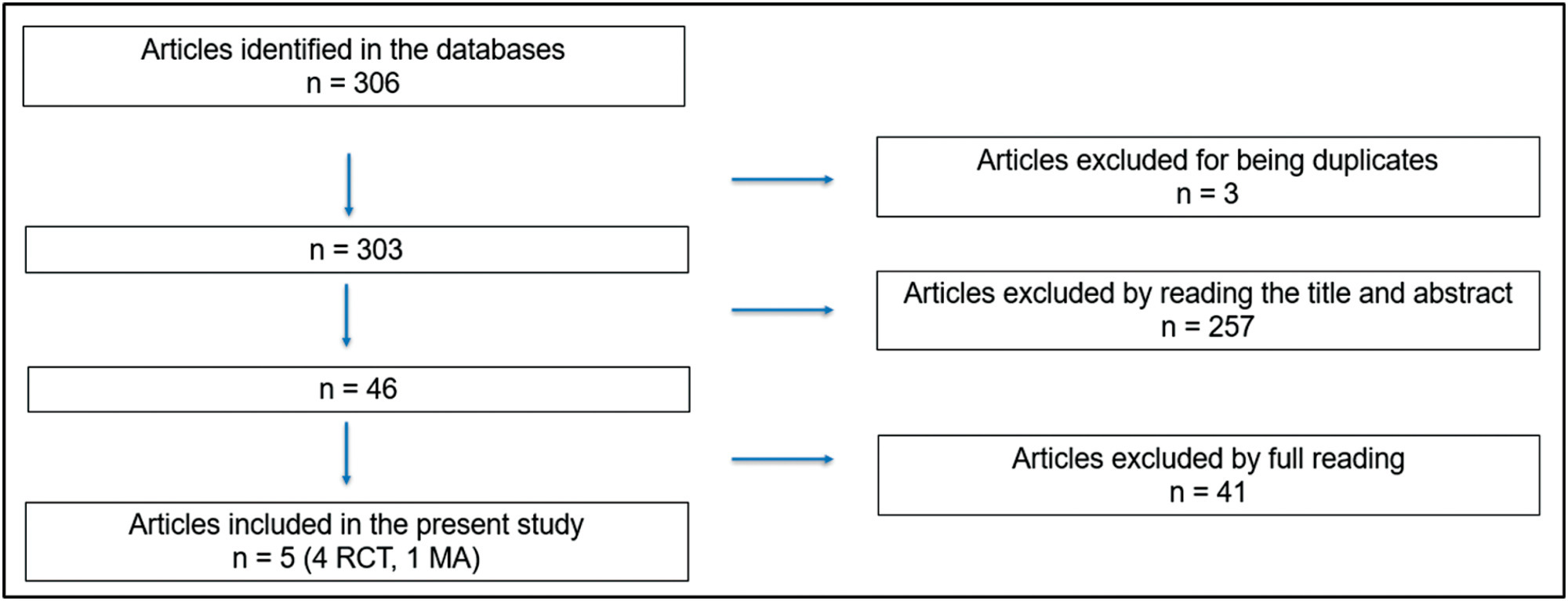
The initial search resulted in 306 articles, of which were excluded three because they were duplicates, 257 after reading the title and abstract and 41 after reading the full text. Thus, five articles were selected for the study: four randomized clinical trials and one metanalysis.
Data collection
The selection of articles was performed by two investigators. The 5 selected articles were read in full and submitted to a comparative analysis.
Data synthesis
Screening through cervicovaginal cytology allows for early diagnosis and reduction of associated mortality, but the procedure can be associated with pain. A small amount of aqueous lubricating gel in the speculum can be used to reduce the discomfort associated with performing cervicovaginal cytology.
Conclusion
The use of lubricating gel in the speculum does not seem to be associated with a change in the cytology result and reduces the discomfort associated with its insertion into the vagina.
-
Original Article
Nonpharmacological Methods to Reduce Pain During Active Labor in A Real-life Setting
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):03-10
04-14-2023
Summary
Original ArticleNonpharmacological Methods to Reduce Pain During Active Labor in A Real-life Setting
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):03-10
04-14-2023Views195See moreAbstract
Objective
To evaluate the association between pain intensity in the active phase of the first stage of labor with the use or not of nonpharmacological methods for pain relief in a real-life scenario.
Methods
This was an observational cross-sectional study. The variables analyzed were obtained by a questionnaire with the mothers (up to 48 hours postpartum) to investigate the intensity of pain during labor using the visual analog scale (VAS). The nonpharmacological pain relief methods routinely used in obstetric practice were evaluated by consulting medical records. The patients were separated into two groups: Group I – patients who did not use nonpharmacological methods for pain relief and Group II –patients who used these methods.
Results
A total of 439 women who underwent vaginal delivery were included; 386 (87.9%) used at least 1 nonpharmacological method and 53 (12.1%) did not. The women who did not use nonpharmacological methods had significantly lower gestational age (37.2 versus 39.6 weeks, p < 0.001) and shorter duration of labor (24 versus 114 min, p < 0.001) than those who used the methods. There was no statistically significant difference in the pain scale score using the VAS between the group that used nonpharmacological methods and the group that did not (median 10 [minimum 2– maximum 10] versus 10 [minimum 6–maximum 10] p = 0.334).
Conclusion
In a real-life setting, there was no difference in labor pain intensity between the patients who used nonpharmacological methods and those who did not use them during the active phase of labor.
-
Original Article
Predictive Factors of Tolerance in Office Hysteroscopy – a 3-Year Analysis from a Tertiary Center
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):38-42
04-14-2023
Summary
Original ArticlePredictive Factors of Tolerance in Office Hysteroscopy – a 3-Year Analysis from a Tertiary Center
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(1):38-42
04-14-2023Views113See moreAbstract
Objective
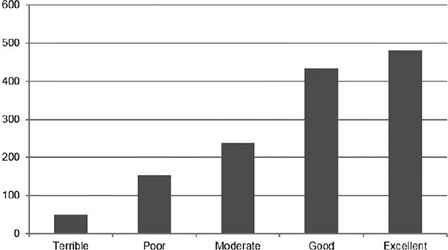
Pain is the primary limitation to performing hysteroscopy. We aimed to evaluate the predictive factors of low tolerance to office hysteroscopic procedures. Methods Retrospective cohort study of the patients who underwent office hysteroscopy from January 2018 to December 2020 at a tertiary care center. Pain tolerance to office-based hysteroscopy was subjectively assessed by the operator as terrible, poor, moderate, good, or excellent. Categorical variables were compared with the use of the Chi-squared test; an independent-samples t-test was conducted to compare continuous variables. Logistic regression was performed to determine the main factors associated with low procedure tolerance.
Results
A total of 1,418 office hysteroscopies were performed. The mean age of the patients was 53 ± 13.8 years; 50.8% of women were menopausal, 17.8% were nulliparous, and 68.7% had a previous vaginal delivery. A total of 42.6% of women were submitted to an operative hysteroscopy. Tolerance was categorized as terrible or poor in 14.9% of hysteroscopies and moderate, good, or excellent in 85.1%. A terrible or poor tolerance was more frequently reported in menopausal women (18.1% vs. 11.7% in premenopausal women, p = 0.001) and women with no previous vaginal delivery (18.8% vs. 12.9% in women with at least one vaginal birth, p = 0.007). Low tolerance led more often to scheduling a second hysteroscopic procedure under anesthesia (56.4% vs. 17.5% in reasonable-to-excellent tolerance, p < 0.0005).
Conclusion
Office hysteroscopy was a well-tolerated procedure in our experience, but menopause and lack of previous vaginal delivery were associated with low tolerance. These patients are more likely to benefit from pain relief measures during office hysteroscopy.
-
Review Article
Efficacy of Transversus Abdominis Plane Block in the Reduction of Pain and Opioid Requirement in Laparoscopic and Robot-assisted Hysterectomy: A Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):55-66
02-28-2022
Summary
Review ArticleEfficacy of Transversus Abdominis Plane Block in the Reduction of Pain and Opioid Requirement in Laparoscopic and Robot-assisted Hysterectomy: A Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):55-66
02-28-2022Views282Abstract
Objective
To summarize the available evidence of TAP Block in efficacy in laparoscopic or robotic hysterectomy.
Data Sources
We searched databases and gray literature for randomized controlled trials in which transversus abdominis plane (TAP) block was compared with placebo or with no treatment in patients who underwent laparoscopic or robot-assisted hysterectomy.
Method of Study
Selection Two researchers independently evaluated the eligibility of the selected articles. Tabulation, Integration, and Results Seven studies were selected, involving 518 patients. Early postoperative pain showed a difference in the mean mean difference (MD): - 1.17 (95% confidence interval [CI]: - 1.87-0.46) in pain scale scores (I2=68%), which was statistically significant in favor of using TAP block, but without clinical relevance; late postoperative pain: DM 0.001 (95%CI: - 0.43-0.44; I2=69%); opioid requirement: DM 0.36 (95%CI: - 0.94-1.68; I2=80%); and incidence of nausea and vomiting with a difference of 95%CI=- 0.11 (- 0.215-0.006) in favor of TAP.
Conclusion
With moderate strength of evidence, due to the high heterogeneity and imbalance in baseline characteristics among studies, the results indicate that TAP block should not be considered as a clinically relevant analgesic technique to improve postoperative pain in laparoscopic or robotic hysterectomy, despite statistical significance in early postoperative pain scale scores.
Key-words laparoscopic hysterectomyOpioidPainrobotic-assisted hysterectomytransversus abdominis plane blockSee more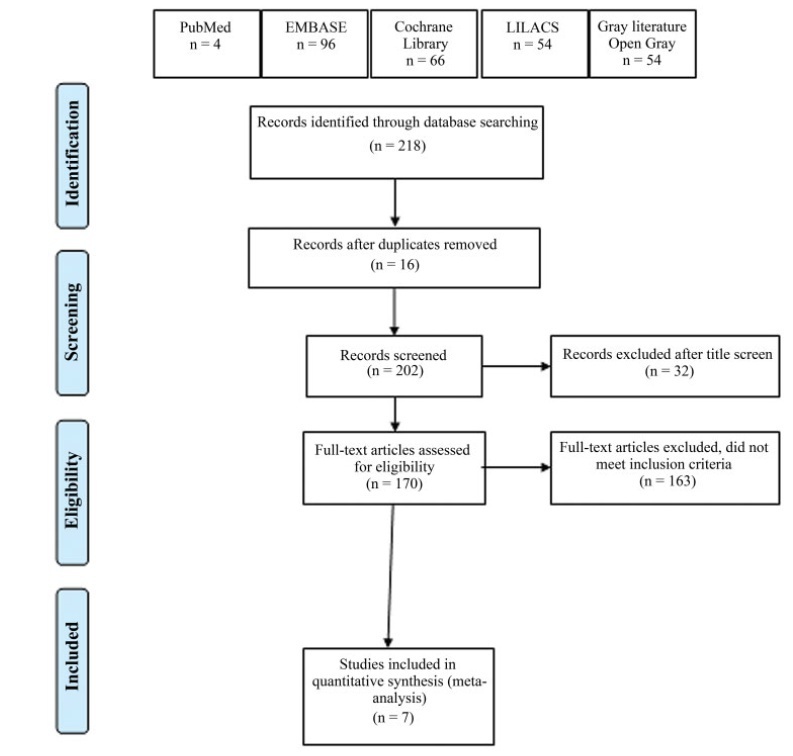
-
Review Article
Primary Dysmenorrhea: Assessment and Treatment
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(8):501-507
09-25-2020
Summary
Review ArticlePrimary Dysmenorrhea: Assessment and Treatment
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(8):501-507
09-25-2020Views349See moreAbstract
Primary dysmenorrhea is defined asmenstrual pain in the absence of pelvic disease. It is characterized by overproduction of prostaglandins by the endometrium, causing uterine hypercontractility that results in uterine muscle ischemia, hypoxia, and, subsequently, pain. It is the most common gynecological illness in women in their reproductive years and one of the most frequent causes of pelvic pain; however, it is underdiagnosed, undertreated, and even undervalued by women themselves, who accept it as part of themenstrual cycle. It hasmajor implications for quality of life, such as limitation of daily activities and psychological stress, being one of themain causes of school and work absenteeism. Its diagnosis is essentially clinical, based on the clinical history and normal physical examination. It is important to exclude secondary causes of dysmenorrhea. The treatment may have different approaches (pharmacological, nonpharmacological and surgical), but the first line of treatment is the use of nonsteroidal anti-inflammatory drugs (NSAIDs), and, in cases of women who want contraception, the use of hormonal contraceptives. Alternative treatments, such as topical heat, lifestyle modification, transcutaneous electrical nerve stimulation, dietary supplements, acupuncture, and acupressure, may be an option in cases of conventional treatments’ contraindication. Surgical treatment is only indicated in rare cases of women with severe dysmenorrhea refractory to treatment.


