Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo44
To describe Top-hat results and their association with margin status and disease relapse in a referral facility in Brazil.
A retrospective study of 440 women submitted to LEEP to treat HSIL, in which 80 cases were complemented immediately by the top hat procedure (Top-hat Group - TH). TH Group was compared to women not submitted to Top-hat (NTH). The sample by convenience included all women that underwent LEEP from January 2017 to July 2020. The main outcome was the histological result. Other variables were margins, age, transformation zone (TZ), depth, and relapse. The analysis used the Chi-square test and logistic regression.
The TH Group was predominantly 40 and older (NTH 23.1% vs. TH 65.0%, p<0.001). No difference was found in having CIN2/CIN3 as the final diagnosis (NTH 17.0% vs. TH 21.3%, p=0.362), or in the prevalence of relapse (NTH 12.0% vs. TH 9.0%, p=0.482). Of the 80 patients submitted to top hat, the histological result was CIN2/CIN3 in eight. A negative top hat result was related to a negative endocervical margin of 83.3%. A CIN2/CIN3 Top-hat result was related to CIN2/CIN3 margin in 62.5% (p=0.009). The chance of obtaining a top hat negative result was 22.4 times higher (2.4-211.0) when the endocervical margin was negative and 14.5 times higher (1.5-140.7) when the ectocervical margin was negative.
The top hat procedure did not alter the final diagnosis of LEEP. No impact on relapse was observed. The procedure should be avoided in women of reproductive age.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(11):689-698
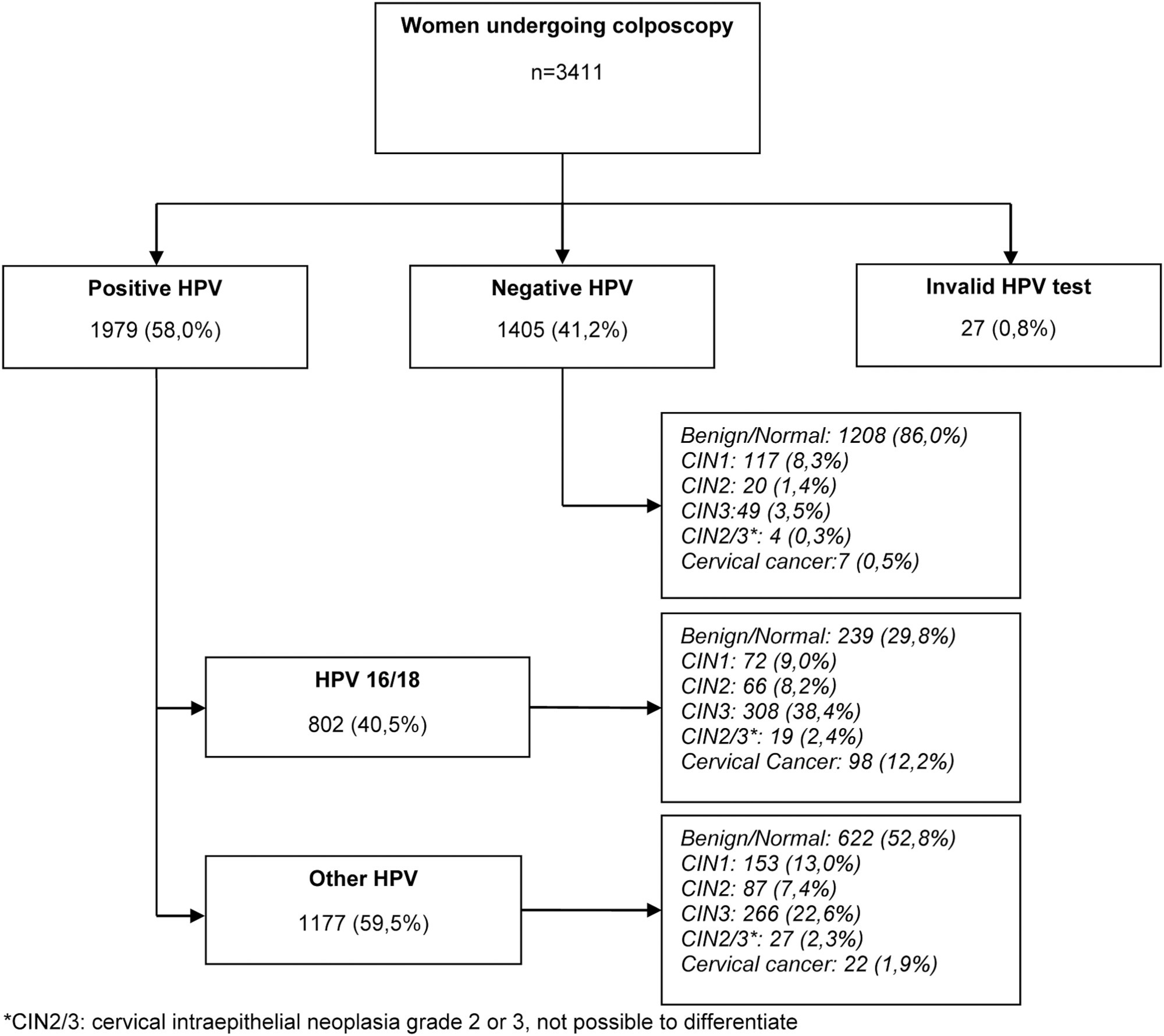
The present study aims to establish a risk profile for high-grade cervical lesions and cervical cancer (CIN2 + ) in women undergoing colposcopy at the Hospital do Câncer de Barretos, through the analysis of Human Papillomavirus (HPV) infection, cervical cytology, and patient's age.
Retrospective cross-sectional study based on a computerized database of women aged ≥ 18 years old who underwent colposcopy at the Prevention Department of the Hospital do Câncer de Barretos from 2017 to 2019.
A total of 3,411 women were included, 58.0% were positive for high-risk-HPV test, with a higher prevalence of CIN2+ for HPV16 (30.3%) and other HPV (45.0%). Cytological findings that suggest invasive cervical cancer (squamous cells or adenocarcinoma), regardless of the status of HPV test, showed 100% diagnosis of CIN2 + , while atypias that suggest high-grade lesions, HSIL and ASC-H, positive for HPV test, showed in 86 and 55.2%, respectively, diagnosis of CIN2 + . ASC-H cytological results among women aged > 40 years old and negative HPV were mainly associated with benign findings. We observed that ≤ CIN1 has a higher prevalence among older women with negative HPV, while for high-grade lesions there is an increase among young women HPV16- and/or 18-positive. In cancer diagnosis, we observed a predominance of HPV 16/18 regardless of the age group.
The highest risks of precursor lesions and cervical cancer were found among women with positive HPV 16/18 tests and severe cytological atypia in population screening tests. In addition, cytological findings of ASC-H HPV negative in women > 40 years old usually represent benign findings in histological investigation.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(10):938-944
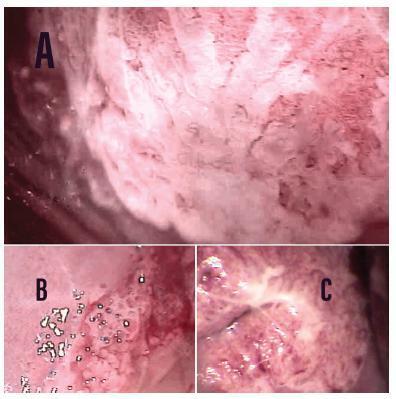
To assess the association between two colposcopic indices, the Swede score and the 2011 International Federation of Cervical Pathology and Colposcopy (IFCPC) Nomenclature as well as to determine the efficacy of the Swede score with cutoffs of 7 and 8.
In the present cross-sectional pilot study, 34 women who had at least 1 colposcopy-directed biopsy due to abnormal cytology were enrolled. The colposcopic findings were scored by both the Swede score and the 2011 IFCPC Nomenclature and were compared with each other. The Kappa coefficient and the McNemar test were used. Accuracy, sensitivity, specificity, and positive and negative predictive values (NPV and PPV, respectively) were calculated, as well as the effectiveness with cutoffs of 7 and 8 in identifying cervical intraepithelial neoplasm (CIN) 2+ when using the Swede score.
The correlation between the 2 colposcopic indices was 79.41%. The Kappa coefficient and the McNemar p-value were 0.55 and 0.37, respectively. The IFCPC Nomenclature had sensitivity, specificity, accuracy, PPV, and NPV of 85.71, 55.00, 67.64, 57.14, and 84.61%, respectively. The Swede score had sensitivity, specificity, accuracy, PPV, and NPV of 100, 63.15, 79.41, 68.18, and 100%, respectively. A Swede score cutoff of 7 for CIN 2+ detection had a specificity of 94.73%, while with a cutoff of 8 it increased to 100%. The sensitivity for both values was 60%. The PPV and NPV for cutoffs of 7 and 8 were 90 and 75 and 100 and 76%, respectively.
Although both colposcopic indices have good reproducibility, the Swede score showed greater accuracy, sensitivity, and specificity in identifying CIN 2 + , especially when using a cutoff of 8.
Summary
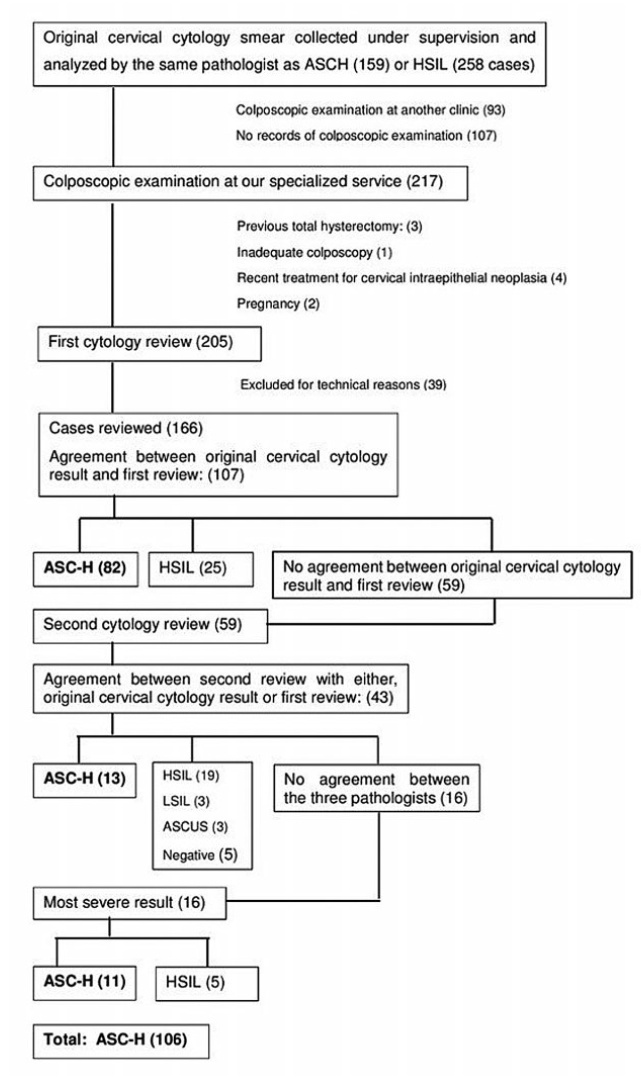
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(2):178-186
To determine the accuracy of colposcopy findings in diagnosing cervical intraepithelial neoplasia (CIN) in women with an atypical squamous cells, cannot exclude high-grade squamous intraepithelial lesion (ASC-H) pap smear result and analyze whether the prevalence of HSIL and cancer correlates with sociodemographic risk factors and specific colposcopic findings.
Colposcopic findings and sociodemographic risk factors were analyzed as possible predictors of a CIN 2 or worse diagnosis in women with an ASC-H pap smear result.
Accuracy of the colposcopic impression was 92%, sensitivity was 91.6%, and specificity was 93.1%, with a positive predictive value of 96.4% and negative predictive value of 84.3%. Diagnosis of CIN 2 or worse was more frequent in patients with a previous history of cervical dysplasia and pre-menopausal patients. Identification of major colposcopic findings, dense acetowhite epithelium, coarse mosaicism, and punctuation correlated significantly with CIN 2 or worse.
Colposcopy performed by an experienced examiner can accurately differentiate patients with CIN 1 or less from patients with CIN 2 or worse. Diagnosis of CIN 2 or worse was more frequent in patients with a previous history of cervical dysplasia and pre-menopausal patients. The degree of acetowhite changes was the best colposcopic feature to predict CIN2 or worse.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(3):280-286
The purpose of this study was to compare the frequency of the occurrence of high-risk human papillomavirus (HPV) and abnormal anal cytology in immunocompetent women with and without HPV-induced genital lesions.
This analytical cross-sectional, observational study was conducted between July 2017 and December 2018 in a specialized outpatient clinic of a tertiary hospital in Fortaleza, CE. Fifty-seven immunocompetent women with and without genital intraepithelial lesions were assessed; they were divided into two groups: group 1 was comprised of women with HPV-associated genital lesions (n=26), and group 2 was comprised of those without HPV-associated genital lesions (n=31). Samples for liquidbased cytology and high-risk DNA-HPV polymerase chain reaction real-time tests were collected from the cervix and anus. All cases were evaluated using high-resolution anoscopy; biopsies were performed when required. The Fisher exact and chi-squared tests were applied for consolidated data in the contingency table, and the Student ttest and Mann-Whitney U-test for independent variables.
Anal high-risk HPV infections were more frequent in group 1 (odds ratio [OR], 4.95; 95% confidence interval [CI], 1.34-18.3; p=0.012), along with concomitant highrisk HPV infections in the uterine cervix and the anus (OR 18.8; 95% CI, 2.20-160; p<0.001). The incidence of high-risk cervical HPV infection was associated with highrisk anal HPV infection (OR, 4.95; 95% CI, 1.34-18.3; p=0.012). There was no statistical difference concerning abnormal anal cytology or anoscopy between the groups, and no anal intraepithelial lesion was found in either group.
Immunocompetent women with HPV-associated genital lesions and high-risk cervical HPV were more likely to have high-risk anal HPV.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(3):140-145
To describe the referral for colposcopy in a Hospital in Brazil and the relative frequency of patients who benefited from it, considering the correct indications for the examination and its final diagnoses.
A retrospective study was performed in the colposcopy service database of the Hospital Universitário de Taubaté, Taubaté, state of São Paulo, Brazil. The frequency validated in the analysis of the medical records of women referred for clinical indication or cytological alteration, attended from March 2015 to March 2017. The population selected and analyzed included 256 results that were correlated to the cytological, clinical data and the result of the colposcopy.
Of the women referred, 45% presented out of the age of screening according to the guidelines of cervical cancer screening, 8.6% being adolescents and young adults < 25 years old, and 36.4% of the patients being ≥ 65 years old. A total of 50% of the patients had no indication of colposcopy, that is, normal cytologies, benign changes, ectopia, cervicitis, atypical squamous cells of indeterminate significance (ASC-US) and low-grade intraepithelial lesion (LSIL) without persistence and normal clinical appearance. A total of 39.84% who underwent colposcopy had high-grade lesion or cancer results, thus benefiting from the adequate referral.
Most (60.16%) of the patients referred to the colposcopy service did not benefit from the referral for results without changes, such as negative colposcopies, histologies with no cervical intraepithelial neoplasm (CIN) or only CIN 1, or were out of the age for screening. These findings therefore demonstrate a significant number of unnecessary and inadequate referrals.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):410-416
To estimate the cytological and colposcopic performances for the diagnosis of cervical neoplasias.
Cross-sectional retrospective study with data from patients’ charts. The participants underwent colposcopy, guided biopsies, and excision when needed. The cytological and colposcopic categorization followed the Bethesda System and the international colposcopic terminologies. The cytology and colposcopy performances were evaluated by sensitivity (SE), specificity (SP), positive predictive value (PPV), and negative predictive value (NPV) analyses with 95% confidence interval (95% CI).
From 1,571 participants, a total of 1,154 (73.4%) were diagnosed with cervical squamous intraepithelial neoplasia grade 2 or worse (CIN 2+), 114 (7.2%) with adenocarcinoma in situ or worse (AIS+), 615 (39.2%) presented atypical squamous cells, cannot exclude high-grade squamous intraepithelial lesion or worse (ASC-H+) cytology, and 934 (59.4%) presented major or suspicious for invasion colposcopic abnormalities. The SE, SP, PPV, and NPV of ASC-H+ for diagnoses of CIN 2+ and AIS+ were, respectively: 44% (95% CI: 41-47) and 72% (95% CI: 67-76), 79% (95% CI: 77-81) and 79% (95% CI: 75-83), 88% (95% CI: 87-90) and 55% (95% CI: 50-60), and 28% (95% CI: 26-31) and 88% (95% CI: 85-91). The SE, SP, PPV, and NPV of major or suspicious for invasion colposcopic abnormalities for diagnoses of CIN 2+ and AIS+were, respectively: 62% (95% CI: 60-65) and 86% (95% CI: 83-89), 59% (95% CI: 57-62) and 59% (95% CI: 55-64), 85% (95% CI: 83-87) and 44% (95% CI: 40-49), and 29% (95% CI: 27-32) and 92% (95% CI: 89-94).
The SE analyses results of ASC-H+ and major or suspicious for invasion colposcopic abnormalities were higher for diagnoses of glandular neoplasias. These results confirm the role of cytology in identifying women at risk who will have their final diagnoses settled by colposcopy and histology.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(3):123-127
Expectant follow-up for biopsy-proven cervical intraepithelial neoplasia (CIN) 1 is the current recommendation for the management of this lesion. Nevertheless, the performance of the biopsy guided by colposcopy might not be optimal. Therefore, this study aimed to calculate the rate of underdiagnoses of more severe lesions in women with CIN 1 diagnosis and to evaluate whether age, lesion extent and biopsy site are factors associated with diagnostic failure.
Eighty women with a diagnosis of CIN 1 obtained by colposcopy-guided biopsy were selected for this study. These women were herein submitted to large loop excision of the transformation zone (LLETZ). The prevalence of lesions more severe than CIN 1 was calculated, and the histological diagnoses of the LLETZ specimens were grouped into two categories: "CIN 1 or less" and "CIN 2 or worse."
The prevalence of lesions diagnosed as CIN 2 or worse in the LLETZ specimens was of 19% (15/80). Three women revealed CIN 3, and 1 woman revealed a sclerosing adenocarcinoma stage I-a, a rare type of malignant neoplasia of low proliferation, which was not detected by either colposcopy or previous biopsy. The underdiagnosis of CIN 2 was not associated with the women's age, lesion extension and biopsy site.
The standard methods used for the diagnosis of CIN 1 may underestimate the severity of the true lesion and, therefore, women undergoing expectant management must have an adequate follow-up.