Summary
Rev Bras Ginecol Obstet. 2023;45(9):511-516
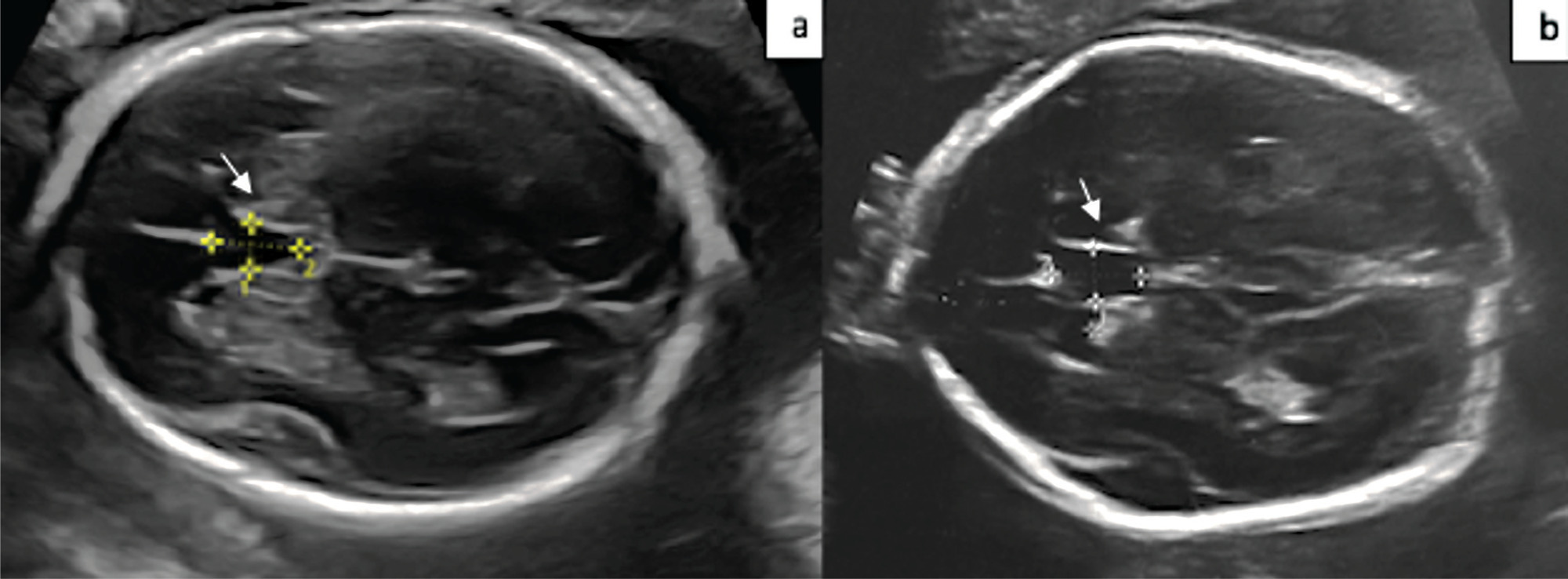
The aim of the present study is to compare the cavum septum pellucidi (CSP) z-score in euploid and aneuploid fetuses and to investigate the performance of the CSP width/length and CSP width/biparietal diameter (BPD) ratios as a diagnostic marker in aneuploidy.
A total of 54 patients, 20 aneuploid and 35 euploid fetuses, between 18 and 37 weeks of gestation, were included in this retrospective study. The CSP width z-score was compared between the two groups. Receiver operating characteristic (ROC) curves were calculated for the CSP width/length and CSP width/BPD ratios to predict aneuploidy.
The median CSP width was 4.8 mm (range, 1.8 to 8.5 mm) in the euploid group, and 5.4 mm (range 3.1 to 8.4 mm) in the aneuploid group. Cavum septum pellucidi width z-score, CSP width/length ratio, and CSP width/BPD ratio were significantly higher in fetuses with aneuploidy than in fetuses with normal karyotype (p = 0.001; p = 0.013; p = 0.028). In the ROC analysis, the CSP width/length ratio had the optimal cutoff value of 0.59, with 72.0% sensitivity and 58.0% specificity, and for the CSP width/BPD ratio, the cutoff value was 0.081 with 83.0% sensitivity and 61.0% specificity for detection of aneuploidy.
CSP width z-score was found to be increased in aneuploid fetuses. The CSP width /BPD ratio can be used as a new marker for predicting aneuploidy.
Summary
Rev Bras Ginecol Obstet. 2018;40(7):384-389
The main objective of this study was to examine the diagnostic performance of the first-trimester combined test for aneuploidies in unselected pregnancies from Rio de Janeiro and compare it with the examples available in the literature.
We investigated 3,639 patients submitted to aneuploidy screening from February 2009 to September 2015. The examination is composed of the Fetal Medicine Foundation risk evaluation based on nuchal translucency evaluation, mother’s age, presence of risk factors, presence of the nasal bone and Doppler of the ductus venous in addition to biochemical analysis of pregnancy-associated plasma protein A (PAPP-A) and beta-human chorionic gonadotropin (β-hCG) markers. The cut-off point for high risk for aneuploidies was defined as greater than 1:100, with intermediate risk defined between 1:100 and 1:1,000, and low risk defined as less than 1:1,000. The variable aneuploidy was considered as a result not only of trisomy of chromosome 21 but also trisomy of chromosomes 13 and 18.
Excluding the losses, the results of 2,748 patients were analyzed. The firsttrimester combined test achieved 71.4% sensitivity with a 7.4% false-positive (FP) rate, specificity of 92.6%, positive predictive value (PPV) of 6.91% and negative predictive value (NPV) of 99.76%, when the cut-off point considered was greater than 1:1,000. Through a receiving operating characteristics (ROC) curve, the cut-off point that maximized the sensitivity and specificity for the diagnosis of aneuploidies was defined as 1:1,860. When we adjusted the false-positive (FP) rate to 5%, the detection rate for this analysis is 72.7%, with a cut-off point of 1:610.
The combined test of aneuploidy screening showed a detection rate inferior to those described in the literature for a higher FP rate.
Summary
Rev Bras Ginecol Obstet. 2015;37(7):333-338
DOI 10.1590/S0100-720320150005373
To describe the prevalence of malformations found in fetuses with trisomy of chromosomes 13, 18 and 21 by identifying the most frequent within each condition.
A retrospective cross-sectional study with the analysis of trisomy cases of chromosomes 13, 18 and 21 diagnosed through fetal karyotype obtained by amniocentesis/cordocentesis, between October 1994 and May 2014, at a Teaching Hospital in Brazil Southern Region. Malformations identified through morphological ultrasonography were described and, subsequently, confirmed in newborn examinations and/or fetal autopsy. The results were analyzed using Fisher's test and analysis of variance (ANOVA), with a 5% level of significance (p=0.05).
Sixty-nine cases of trisomy were diagnosed among 840 exams; nine were excluded due to outcome outside Hospital de Clínicas de Porto Alegre or incomplete records, remaining 60 cases (nine cases of chromosome 13 trisomy, 26 of chromosome 18, and 25 of chromosome 21). In all three groups, heart disease occurred in most cases; the ventricular septal defect was more prevalent and occurred in 66.7% of the trisomy 13 group. Gastrointestinal abnormalities were more prevalent in the trisomy 18 group, especially omphalocele (38.5%; p<0.01). Genitourinary anomalies were more significantly frequent in the trisomy 13 group (pyelectasis, 55.6% - p<0.01; ambiguous genitalia, 33.3% - p=0.01). Central nervous system defects were identified in all cases of trisomy 13. Facial cracks were significantly more prevalent among fetuses with trisomy 13 (66.7%; p<0.01). Hand and feet malformations significantly differed among the trisomy groups. Hand defects occurred in 50% of trisomy 18 cases, and in 44.4% of all trisomy 13 cases (p<0.01); congenital clubfoot was more common in the trisomy 18 group, being detected in 46.2% of fetuses (p<0.01). The abnormalities were found in 50.9, 27.3 and 21.7% of trisomy 18, 13 and 21 cases respectively.
Many fetal malformations identified at ultrasound are suggestive of trisomy and represent an important tool for etiologic diagnosis and prenatal and pre-conception genetic counseling.
Summary
Rev Bras Ginecol Obstet. 2006;28(3):151-157
DOI 10.1590/S0100-72032006000300003
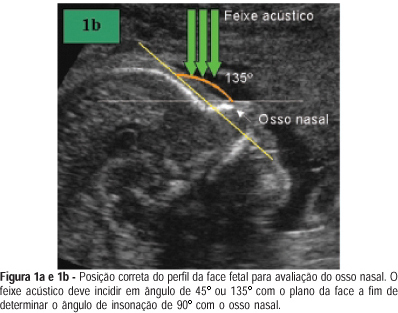
PURPOSE: the absence of fetal nasal bone is correlated with trisomy 21. Although a hypoplastic nasal bone is also correlated with trisomy 21, there is no clear definition of this term in the literature. Our objective was to establish the reference values for fetal nasal bone size throughout gestation in a local population in Brazil. METHODS: it is a cross-sectional study on 902 fetuses at 10 to 39 weeks of gestation. After having excluded fetal malformations and maternal diseases which are known to interfere with fetal growth, 625 fetuses were selected. We obtained a mid-sagittal view of the fetal profile by holding the ultrasound bean at an angle of 45º or 135º. The nasal bone size mean was calculated by using polynomial regression. The Anderson-Darling test proved the normal distribution of the measurements (p>0.05). RESULTS: of the 625 fetuses, 88.3% were from single gestations and 11.7% from multiple ones. There was a direct correlation between fetal nasal bone size and gestational age. The variability of nasal bone size became larger as gestational age increased. Minimal length of 1.0 and 4.7 mm in the first and second trimesters, respectively, were found. CONCLUSIONS: there is a direct correlation between fetal nasal bone size and gestational age. This correlation is valid either for a single gestation or a multiple one. These measurements of the fetal nasal bone will allow us to use them as a screening test for cromosomal abnormalities. This is a useful study if we consider the large miscegenation of the Brazilian population. However, further systematic and standardized approach to study the fetal nasal bone is needed to establish its real value in fetuses once classified as at high or low risk for aneuploidies.
Search
Search in:
breast (42) breast cancer (42) breast neoplasms (95) Cesarean section (72) endometriosis (66) infertility (56) Maternal mortality (43) menopause (82) obesity (58) postpartum period (40) pregnancy (225) Pregnancy complications (99) Prenatal care (68) prenatal diagnosis (50) Prevalence (41) Quality of life (51) risk factors (94) ultrasonography (79) urinary incontinence (40) women's health (48)