Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(9):562-568
The present comprehensive review aims to show the full extent of what is known to date and provide a more thorough view on the effects of SARS-CoV2 in pregnancy.
Between March 29 and May, 2020, the words COVID-19, SARS-CoV2, COVID- 19 and pregnancy, SARS-CoV2 and pregnancy, and SARS and pregnancy were searched in the PubMed and Google Scholar databases; the guidelines from well-known societies and institutions (Royal College of Obstetricians and Gynaecologists [RCOG], American College of Obstetricians and Gynecologists [ACOG], International Society of Ultrasound in Obstetrics & Gynecology [ISUOG], Centers for Disease Control and Prevention [CDC], International Federation of Gynecology and Obstetrics [FIGO]) were also included.
The COVID-19 outbreak resulted in a pandemic with > 3.3 million cases and 230 thousand deaths until May 2nd. It is caused by the SARS-CoV2 virus and may lead to severe pulmonary infection and multi-organ failure. Past experiences show that unique characteristics in pregnancy make pregnant women more susceptible to complications from viral infections. Yet, this has not been reported with this new virus. There are risk factors that seem to increase morbidity in pregnancy, such as obesity (body mass index [BMI] > 35), asthma and cardiovascular disease. Current reports describe an increased rate of pretermbirth and C-section. Vertical transmission
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(8):501-507
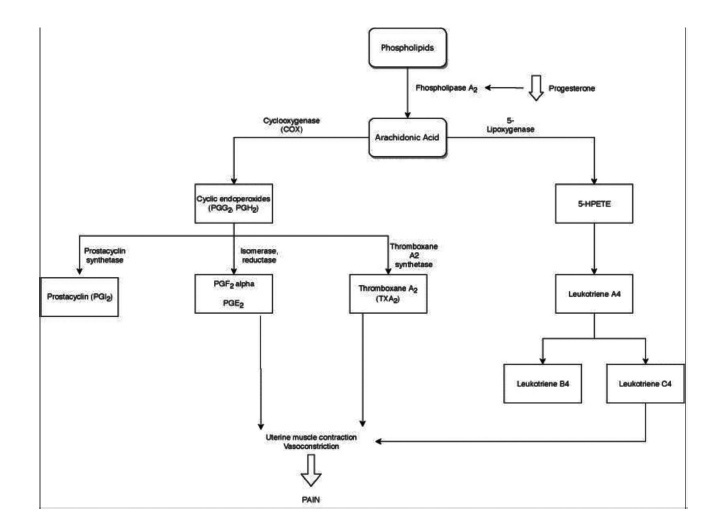
Primary dysmenorrhea is defined asmenstrual pain in the absence of pelvic disease. It is characterized by overproduction of prostaglandins by the endometrium, causing uterine hypercontractility that results in uterine muscle ischemia, hypoxia, and, subsequently, pain. It is the most common gynecological illness in women in their reproductive years and one of the most frequent causes of pelvic pain; however, it is underdiagnosed, undertreated, and even undervalued by women themselves, who accept it as part of themenstrual cycle. It hasmajor implications for quality of life, such as limitation of daily activities and psychological stress, being one of themain causes of school and work absenteeism. Its diagnosis is essentially clinical, based on the clinical history and normal physical examination. It is important to exclude secondary causes of dysmenorrhea. The treatment may have different approaches (pharmacological, nonpharmacological and surgical), but the first line of treatment is the use of nonsteroidal anti-inflammatory drugs (NSAIDs), and, in cases of women who want contraception, the use of hormonal contraceptives. Alternative treatments, such as topical heat, lifestyle modification, transcutaneous electrical nerve stimulation, dietary supplements, acupuncture, and acupressure, may be an option in cases of conventional treatments’ contraindication. Surgical treatment is only indicated in rare cases of women with severe dysmenorrhea refractory to treatment.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):427-435
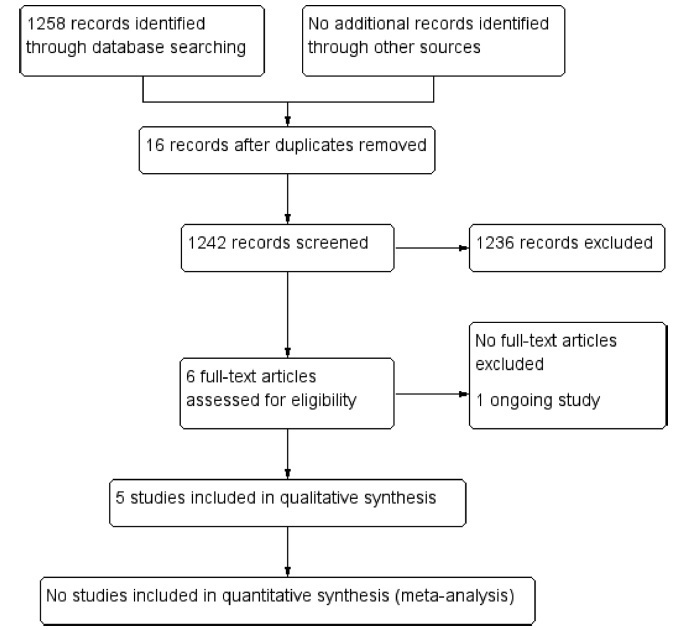
We performed a systematic review to assess the effectiveness and safety of Tribulus terrestris to treat female sexual dysfunction (FSD).
We performed unrestricted electronic searches in the MEDLINE, CENTRAL, EMBASE, LILACS, CINAHL, PsycINFO,WHO-ICTR, Clinicaltrials.gov and OpenGrey databases. Selection of studies We included any randomized controlled trials (RCTs) that compared T. terrestris versus inactive/active interventions. After the selection process, conducted by two reviewers, 5 RCTs (n = 279 participants) were included.
Data extraction was performed by two reviewers with a preestablished data collection formulary.
Due to lack of data and clinical heterogeneity, we could not perform meta-analyses. The risk of bias was assessed by the Cochrane Risk of Bias (RoB) tool, and the certainty of evidence was assessed with Grading of Recommendations, Assessment, Development and Evaluations (GRADE).
After 1 to 3 months of treatment, premenopausal and postmenopausal women randomized to T. terrestris had a significant increase in sexual function scores. Three months of treatment with T. terrestris showed a significant increase in the serum testosterone levels of premenopausal women. There was no report of serious adverse events, and none of the studies assessed health-related quality of life. The certainty of the evidence was very low, whichmeans that we have very little confidence in the effect estimates, and future studies are likely to change these estimates.
MoreRCTs are needed to supportor refute the use of T. terrestris. The decision to use this intervention should be shared with the patients, and the uncertainties around its effects should be discussed in the clinical decision-making process. Number of Protocol registration in PROSPERO database: CRD42019121130
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):420-426
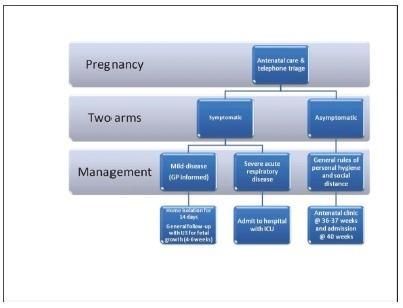
Since the World Health Organization (WHO) declared coronavirus infection (COVID-19) a Public Health Emergency of International Concern in January 2020, there have been many concerns about pregnant women and the possible effects of this emergency with catastrophic outcomes inmany countries. Information on COVID-19 and pregnancy are scarce and spread throughout a fewcase series, with no more than 50 cases in total. The present review provides a brief analysis of COVID-19, pregnancy in the COVID-19 era, and the effects of COVID-19 on pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(7):415-419
It is estimated that around 28 million surgeries will be postponed or canceled worldwide as a result of this pandemic, causing a delay in the diagnosis and treatment of more than 2 million cancer cases. In Brazil, both the National Health Agency (ANS) and National Health Surveillance Agency (ANVISA) advised the postponement of elective and non-essential surgeries, causing a considerable impact on the number of surgical procedures that decreased by 33.4% in this period. However, some women need treatment for various gynecological diseases that cannot be postponed. The purpose of this article is to present recommendations on surgical treatment during the COVID-19 pandemic.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(6):356-364
The present paper reports on the local treatment of breast cancer from a historical perspective. A search for articles written in English was made in the Medline and EMBASE databases, and 40 papers were selected. Over the past 10 years, various randomized, controlled clinical trials on the local treatment of breast cancer indicated that patients with the samemolecular subtypemay receive different individualized surgical treatments aimed atoptimizing systemic adjuvant therapy. With a view to retaining the gainsmade in diseasefree and overall survival, surgical techniques have advanced from radical surgery to conservative mastectomies, thus reducing sequelae, while adjuvant and neoadjuvant therapies have contributed toward controlling the disease, both distant metastases and local recurrence. Current studies evaluate whether future breast cancer therapy may even succeed in eliminating surgery to the breast and axilla altogether.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(5):289-296
Intrauterine growth restriction (IUGR) is associated with poor perinatal prognosis and a higher risk of stillbirth, neonatal death, and cerebral palsy. Its detection and the evaluation of its severity by new Doppler velocimetric parameters, such as aortic isthmus (AoI), are of great relevance for obstetrical practice. The AoI is a vascular segment that represents a point of communication between the right and left fetal circulations. It is considered to be a functional arterial shunt that reflects the relationship between the systemic and cerebral impedances, and has recently been proposed as a tool to detect the status of hemodynamic balance and prognosis of IUGR in fetuses. In the present review, we noticed that in healthy fetuses, the AoI net flow is always antegrade, but in fetuses with IUGR the deterioration of placental function leads to progressive reduction in its flow until it becomes mostly retrograde; this point is associated with a drastic reduction in oxygen delivery to the brain. The more impaired the AoI flow is, the greater is the risk of impairment in the Doppler velocimetry of other vessels; and the alterations of the AoI Doppler seem to precede other indicators of severe hypoxemia. Although there seems to be an association between the presence of retrograde flow in the AoI and the risk of long-term neurologic disability, its role in the prediction of perinatal morbi-mortality remains unclear. The AoI Doppler seems to be a promising tool in the management of fetuses with IUGR, but more studies are needed to investigate its employment in clinical practice.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(4):218-227
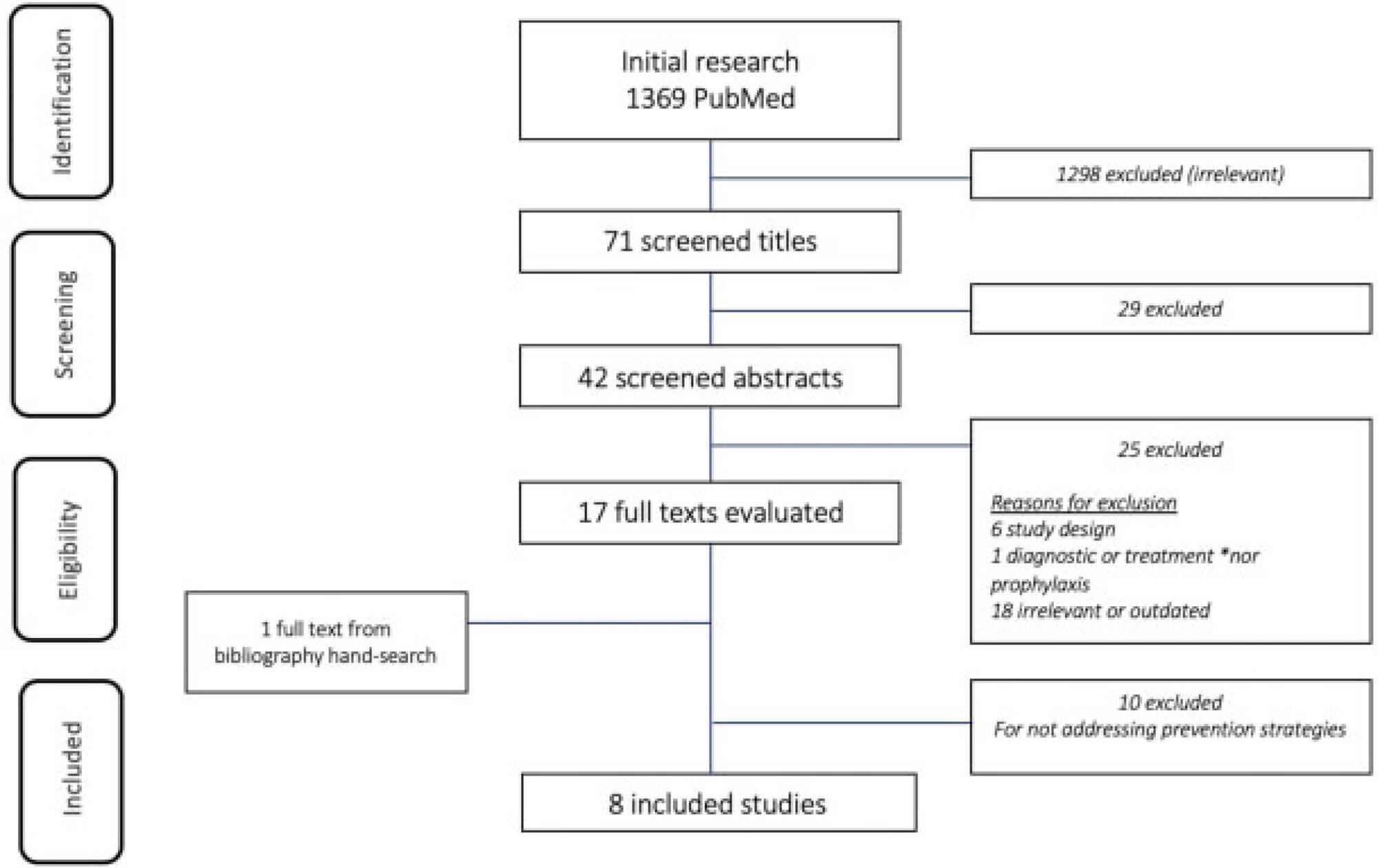
To identify current strategies and recommendations for venous thromboembolism prophylaxis associated with the pregnancy-puerperal cycle, a condition of high morbidity and mortality among women.
The literature search was performed between May and October 2019, using the PubMed database, including papers published in Portuguese, English and Spanish. The terms thromboembolism (Mesh) AND pregnancy (Mesh) OR postpartum (Mesh) were used as descriptors, including randomized controlled trials, meta-analyses, systematic reviews and guidelines published from 2009 to 2019, presenting strategies for prevention of thromboembolism during pregnancy and the postpartum.
Eight articles met the inclusion criteria. Many studies evaluated were excluded because they did not address prevention strategies. We compiled the recommendations from the American Society of Hematologists, the American College of Obstetricians and Gynecologists, the Royal College of Obstetricians and Gynecologists, the Society of Obstetricians and Gynaecologists of Canada, the American College of Chest Physicians and the Royal Australian and New Zealand College of Obstetricians and Gynaecologists.
There are some gaps in the research, and clinical studies with appropriate methodology are needed to support decisions made regarding the risk of thromboembolism in the perigestational period. Thus, the attention of the professionals involved in the care of pregnant and postpartum women is crucial, as it is a condition associated with high morbidity and mortality.