Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo70
To compare outcomes in patients with repeated implantation failure undergoing Intracytoplasmic Sperm Injection/In vitro fertilization (IVF/ICSI) plus immunosuppressants such as prednisolone, prednisone, or cyclosporine A versus the use of IVF/ICSI alone.
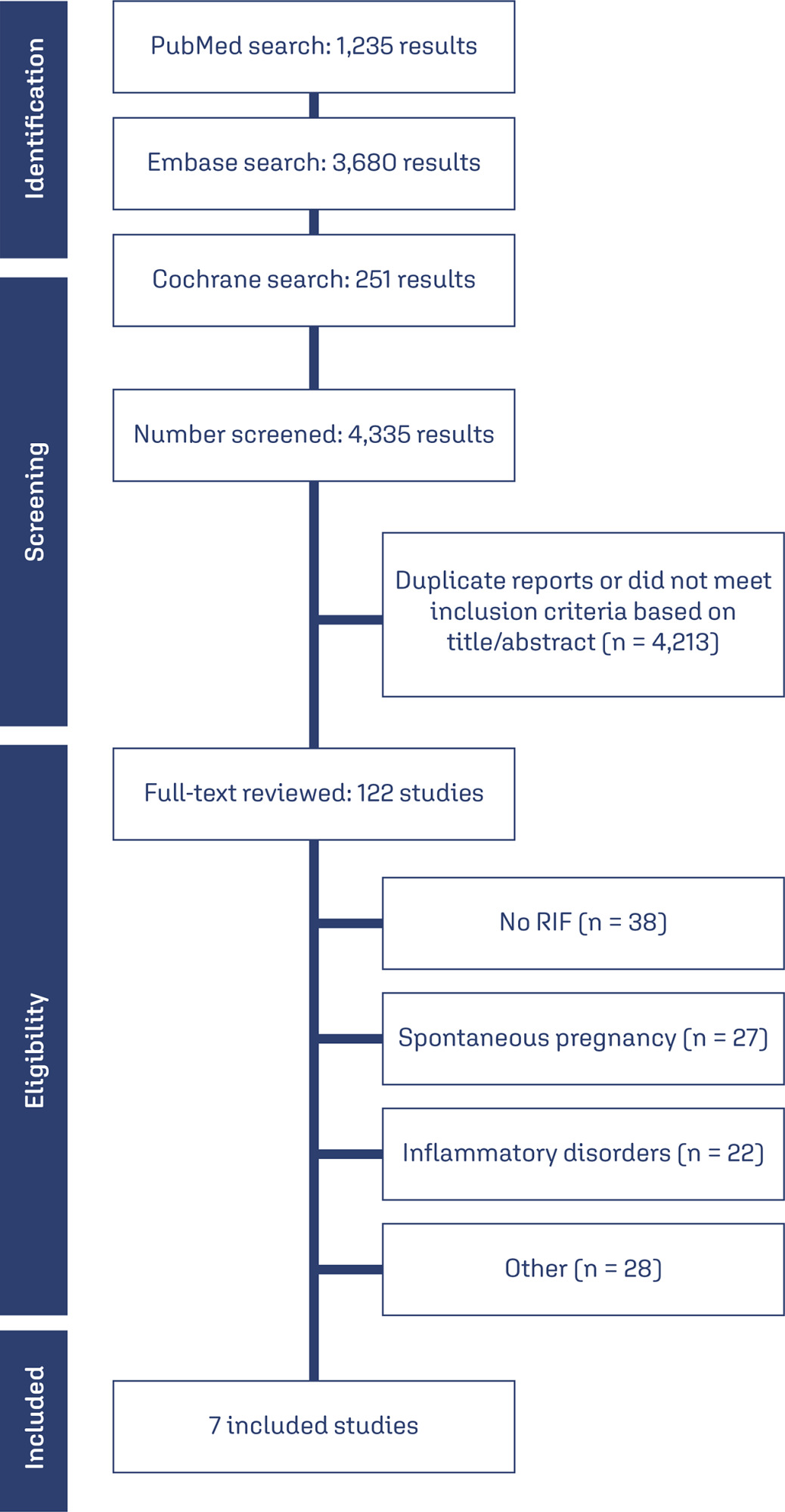
Databases were systematically searched in PubMed, Cochrane, and Embase databases in September 2023.
Randomized clinical trials and observational studies with the outcomes of interest were included.
We computed odds ratios (ORs) for binary endpoints, with 95% confidence intervals (CIs). Heterogeneity was assessed using I2 statistics. Data were analyzed using Review Manager 5.4.The main outcomes were live birth, miscarriage, implantation rate, clinical pregnancy, and biochemical pregnancy.
Seven studies with 2,829 patients were included. Immunosuppressive treatments were used in 1,312 (46.37%). Cyclosporine A improved implantation rate (OR 1.48; 95% CI 1.01-2.18) and clinical pregnancy (1.89, 95% CI 1.14-3.14). Compared to non-immunosuppressive treatment, prednisolone and prednisone did not improve live birth (OR 1.13, 95% CI 0.88-1.46) and miscarriage (OR 1.49, 95% CI 1.07-2.09). Prednisolone showed no significant effect in patients undergoing IVF/ICSI, clinical pregnancy (OR 1.34; 95% CI 0.76-2.36), or implantation rate (OR 1.36; 95% CI 0.76-2.42).
Cyclosporine A may promote implantation and clinical pregnancy rates. However, given the limited sample size, it is important to approach these findings with caution. Our results indicate that prednisolone and prednisone do not have any beneficial effects on clinical outcomes of IVF/ICSI patients with repeated implantation failure.
CRD42023449655
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo69
To compare the effectiveness and safety of non-mRNA versus mRNA COVID-19 vaccines on pregnant women and their newborns in a systematic review with meta-analysis.
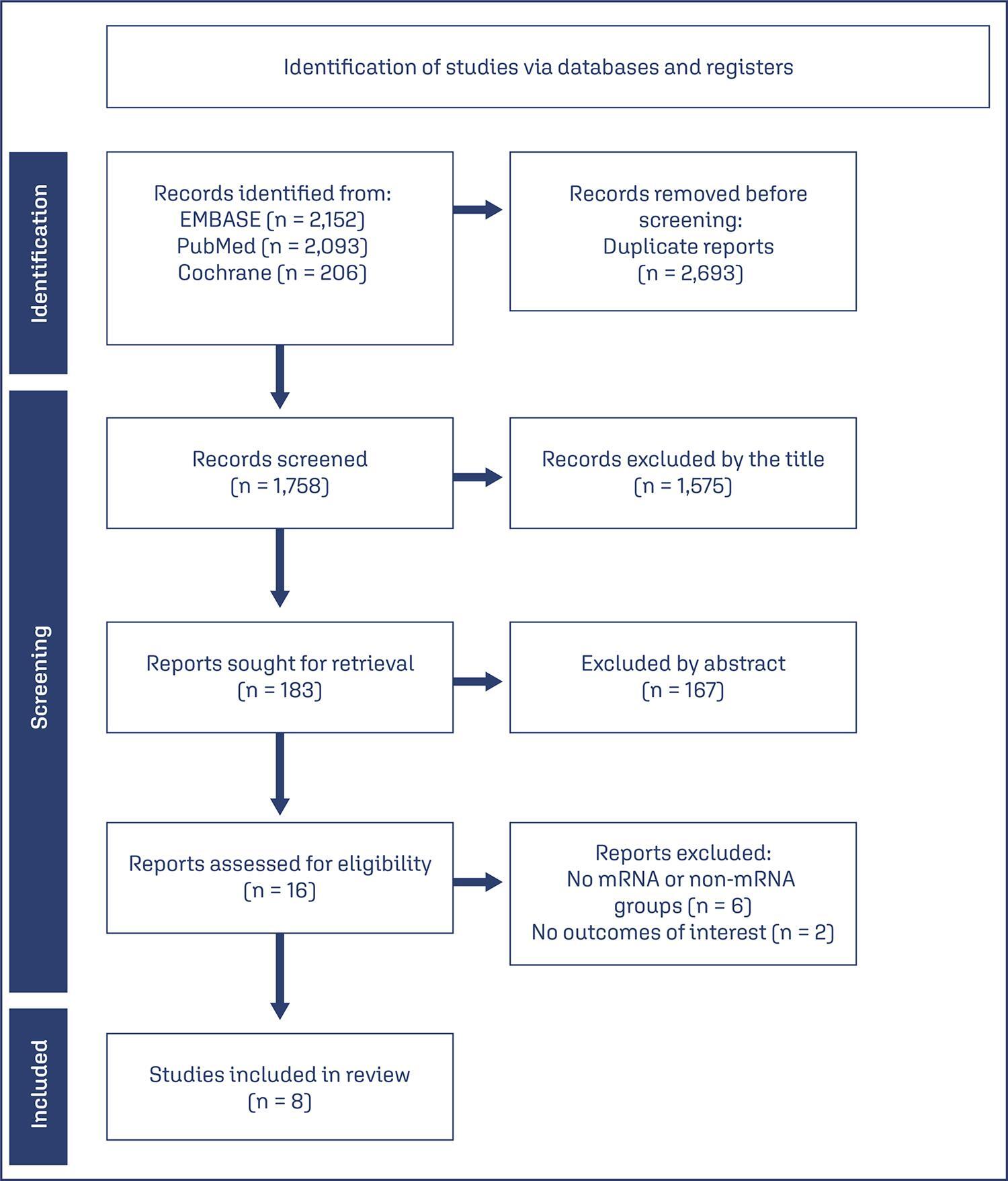
We searched PubMed, Embase, and Cochrane Central in May 2023.
The search strategy yielded 4451 results, 16 studies were fully reviewed. We selected case-control studies analysing non-mRNA versus mRNA vaccines. Data collection and analysis: we assessed the risk of bias using the Cochrane Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool. Standardised mean differences were pooled using random-effect models.
We identified 8 prospective and retrospective studies with a total of 32,153 patients. Non-mRNA vaccines were associated with a higher incidence of fever (OR 2.67; 95% CI 2.08-3.43; p<0.001), and a lower incidence of fetal or neonatal death (OR 0.16; 95% CI 0.08-0.33; p<0.001). In subgroup analyses, the Jansen vaccine (Ad26.COV2.S) was found to have a higher rate of premature labor/delivery (OR 4.48; 95% CI 1.45-13.83; p=0.009) and missed/spontaneous abortion (OR 1.90; 95% CI 1.09-3.30; p=0.02), as compared with the Pfizer (BNT162b2) vaccine.
non-mRNA vaccines are associated with a lower incidence of fetal or neonatal death among pregnant women who receive a Covid19 vaccine, although at an increased rate of pyrexia compared with mRNA vaccines. Other studies are required for better assessment.
CRD42023421814
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo50
To determine the relationship between early age at menarche, late age at menopause with specific subtypes of breast cancer (BC).
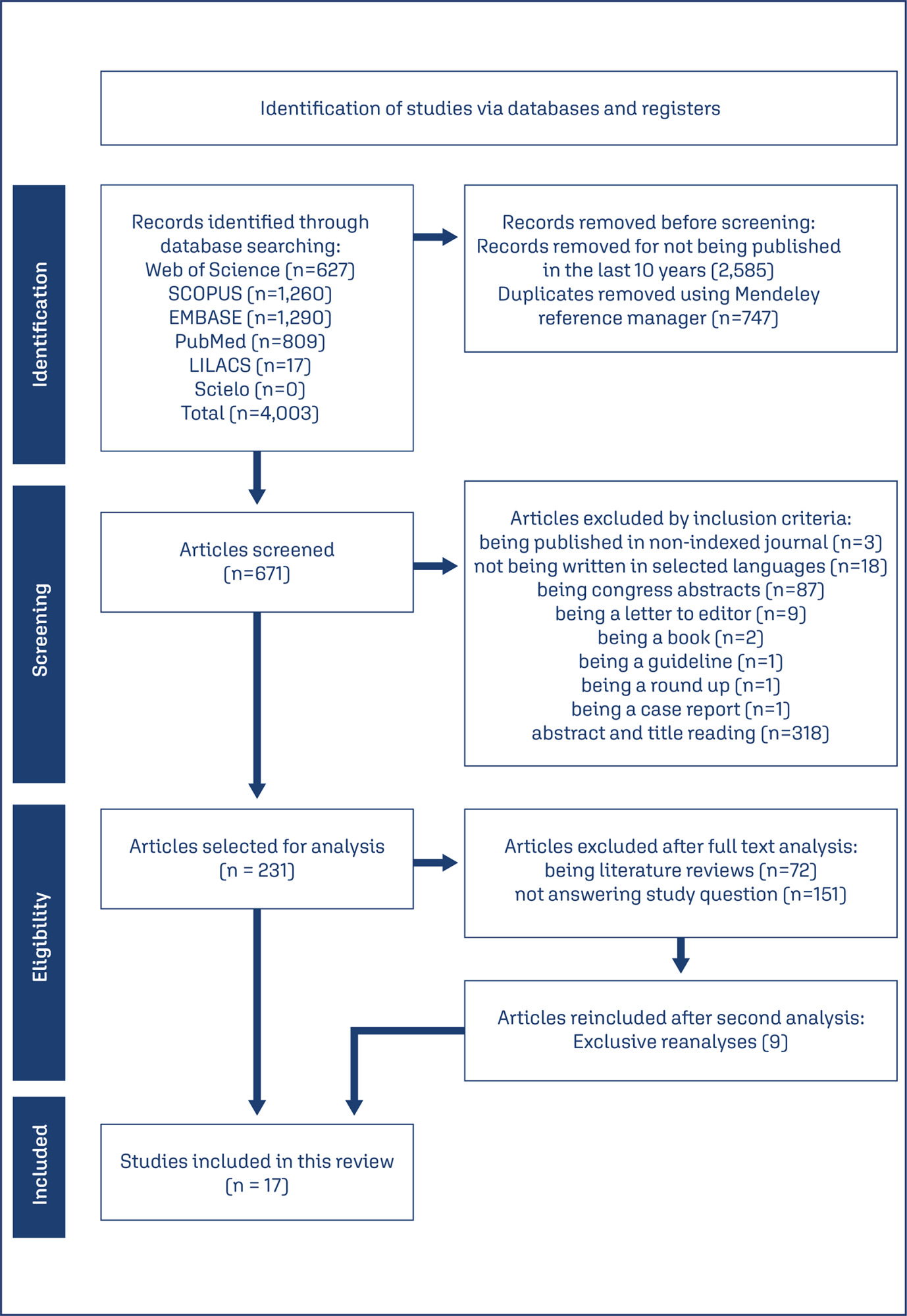
A literature search was conducted in Embase, Lilacs, PubMed, Scopus, and Scielo databases, following the Joanna Briggs Institute scoping review protocol and answering the question “How early age at menarche or late age at menopause are related to different breast cancer subtypes?”.
A number of 4,003 studies were identified, of which 17 were selected. Most of the included articles found a clear relationship between early menarche, late menopause and some subtypes of BC, mainly, PR+, ER+, luminal, and HER-2 tumors. However, some studies have found a contradictory relationship and one study didn’t find any relationship between them.
A relationship between early age at menarche and advanced age at menopause was observed with some subtypes of breast cancer, since other factors must be considered in its understanding.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo72
26% of all pregnancies end in miscarriage, and up to 10% of clinically diagnosed pregnancies, and recurrent pregnancy loss is 5% among couples of childbearing ages. Although there are several known causes of pregnancy loss in the first half, including recurrent pregnancy loss, including parental chromosomal abnormalities, uterine malformations, endocrinological disorders, and immunological abnormalities, about half of the cases of pregnancy loss in its first half remain unexplained.
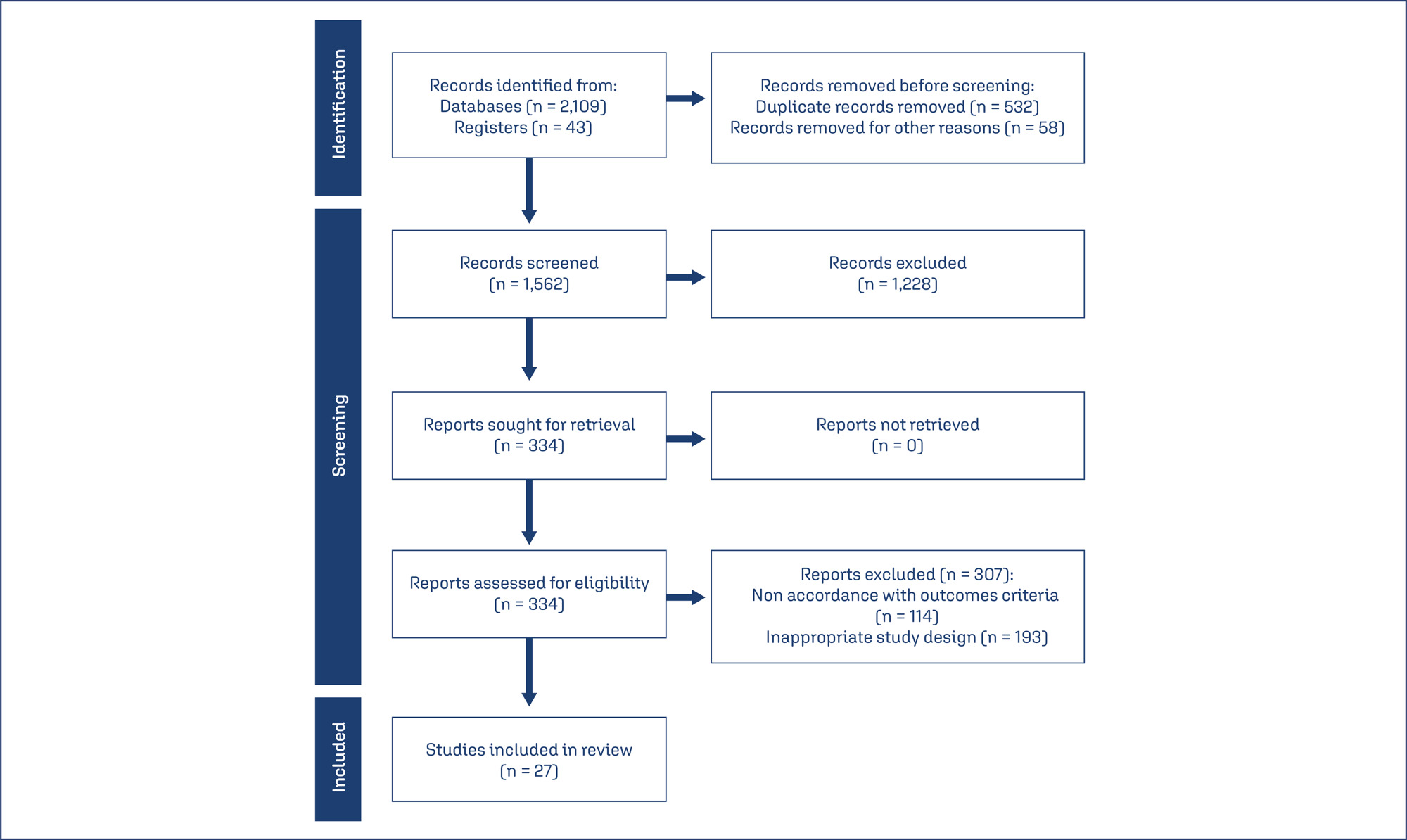
The review includes observational controlled studies (case-control or cohort, longitudinal studies, reviews, meta-analyses), which include the study of biochemical factors for predicting pregnancy losses in the first half, in singlet pregnancy. The Newcastle-Ottawa Scale (NOS) was used to assess the research quality.
Finally, 27 studies were included in the review, which has 134904 examined patients. The results of the review include estimates of β-human chorionic gonadotropin, progesterone, pregnancy-associated protein – A, angiogenic vascular factors, estradiol, α-fetoprotein, homocysteine and CA-125 as a predictors or markers of the first half pregnancy losses.
It may be concluded that to date, research data indicate the unavailability of any reliable biochemical marker for predicting pregnancy losses in its first half and require either a combination of them or comparison with clinical evidence. A fairly new model shall be considered for the assessment of α-fetoprotein in vaginal blood, which may have great prospects in predicting spontaneous miscarriages.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo71
To conduct a systematic review of external validation studies on the use of different Artificial Intelligence algorithms in breast cancer screening with mammography.
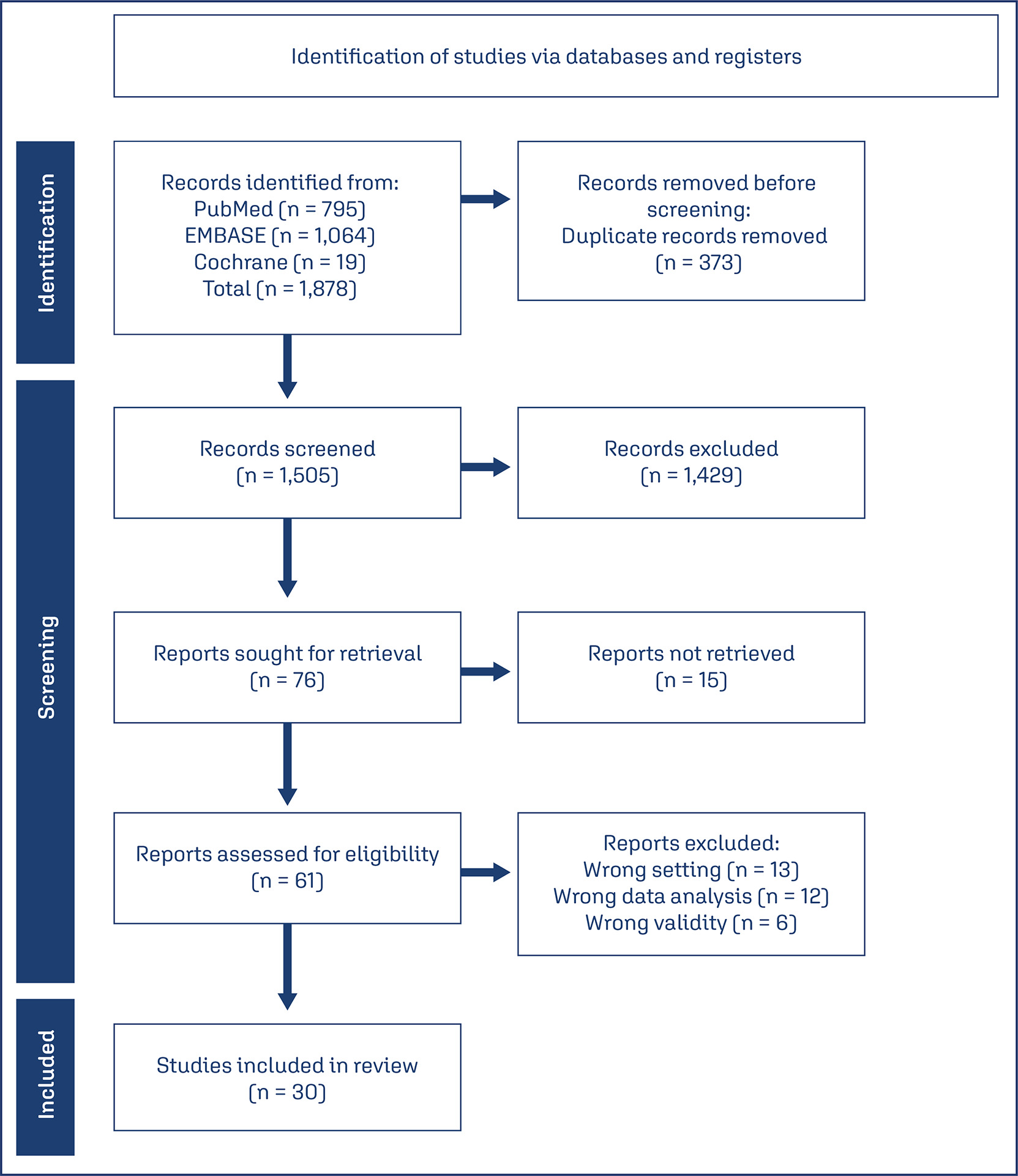
Our systematic review was conducted and reported following the PRISMA statement, using the PubMed, EMBASE, and Cochrane databases with the search terms “Artificial Intelligence,” “Mammography,” and their respective MeSH terms. We filtered publications from the past ten years (2014 – 2024) and in English.
A total of 1,878 articles were found in the databases used in the research. After removing duplicates (373) and excluding those that did not address our PICO question (1,475), 30 studies were included in this work.
The data from the studies were collected independently by five authors, and it was subsequently synthesized based on sample data, location, year, and their main results in terms of AUC, sensitivity, and specificity.
It was demonstrated that the Area Under the ROC Curve (AUC) and sensitivity were similar to those of radiologists when using independent Artificial Intelligence. When used in conjunction with radiologists, statistically higher accuracy in mammogram evaluation was reported compared to the assessment by radiologists alone.
AI algorithms have emerged as a means to complement and enhance the performance and accuracy of radiologists. They also assist less experienced professionals in detecting possible lesions. Furthermore, this tool can be used to complement and improve the analyses conducted by medical professionals.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo22
RhD alloimmunization in pregnancy is still the main cause of hemolytic disease of the fetus and neonate (HDFN). Nevertheless, there are other antigens that may be associated with the occurrence of this phenomenon and that have been growing in proportion, given that current prevention strategies focus only on anti-RhD antibodies. Although not widespread, the screening and diagnostic management of the disease caused by these antibodies has recommendations in the literature. For this reason, the following review was carried out with the objective of listing the main red blood cell antigen groups described — such as Rh, ABO, Kell, MNS, Duffy, Kidd, among others — addressing the clinical importance of each one, prevalence in different countries, and recommended management when detecting such antibodies during pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo49
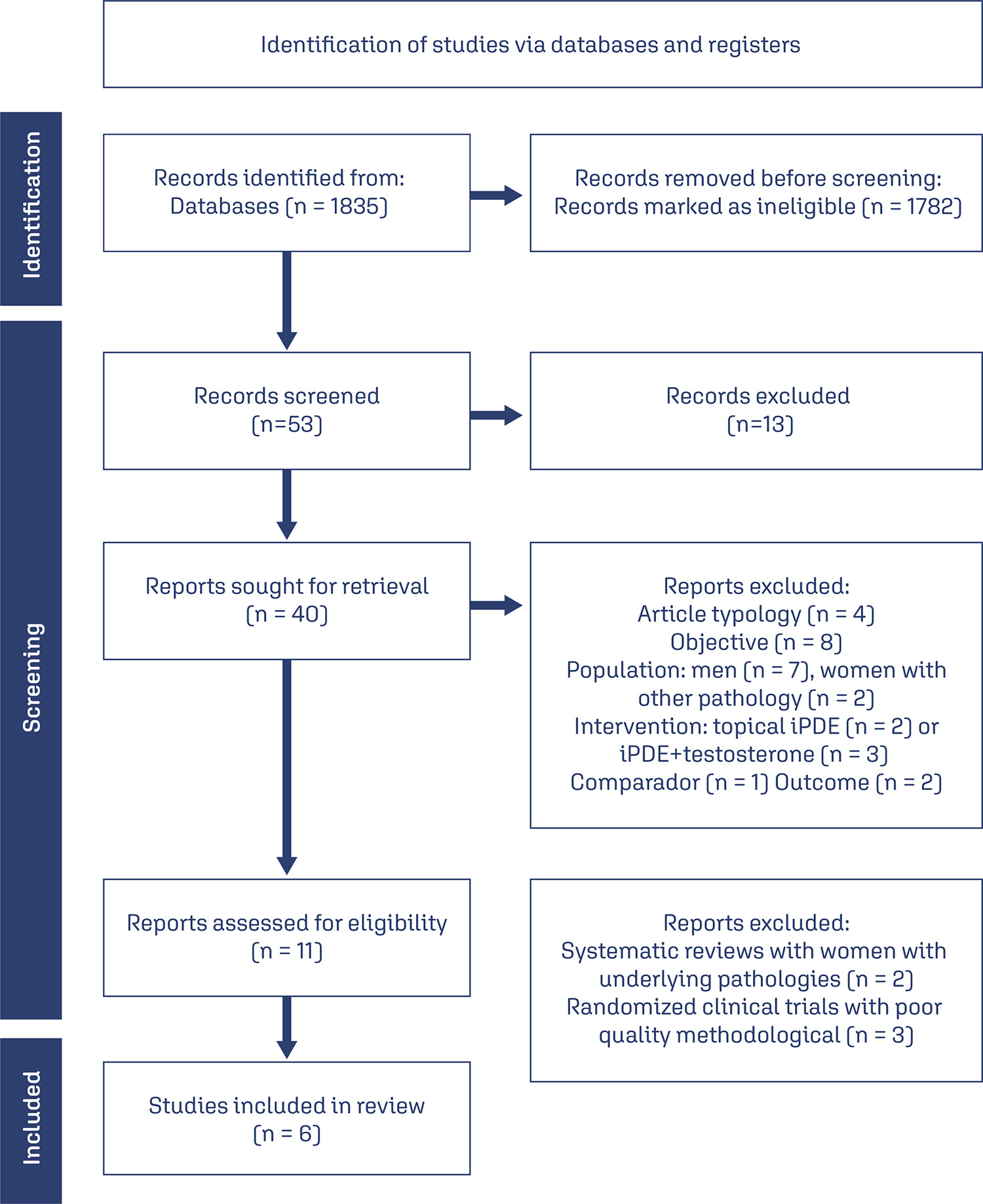
The purpose of this study was to analyze the available evidence regarding the efficacy of iPDE5 in the treatment of female sexual dysfunction (FSD).
A comprehensive literature search was conducted in March 2023 through the main scientific databases.
A total of 53 articles were identified, out of which, 6 met the predefined inclusion criteria. All of these were randomized controlled trials. Among the included studies, 4 demonstrated the effectiveness of sildenafil in improving sexual response and addressing FSD, while 2 studies failed to establish its efficacy in this context.
Overall, the efficacy of sildenafil in the treatment of FSD remains controversial and inconclusive based on the available evidence. Further research is necessary to clarify the therapeutic potential of iPDE5 in addressing FSD and to better understand the factors that influence treatment outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo57
High-risk human papillomavirus (HPV) infection is associated with cervical cancer while low-risk HPV strains mostly cause benign lesions. Multiple studies have also associated HPV with coronary artery (CAD) disease in women. Furthermore, the climacteric period in women, triggers chronic inflammation and has major implications for CAD and associated lipid disorders. The association of HPV with coronary artery disease in climacteric women has few studies, and the objective of this review is to gather and analyse scientific data on the subject. This is an integrative review performed on PubMed and Google Scholar using the keywords “HPV”, “coronary heart disease” and “climacteric”, among these keywords the boolean operator AND and the publication date filter. (2018 onwards). Five articles were found, whose main results show presence of high-risk vaginal HPV in climacteric women. Climacterium and HPV were associated with a three-fold increased risk of CAD, as well as with factors related to menopause that promote atheroma formation, lipid disorders and chronic inflammation. Thus, these results support the association between HPV infection and CAD in climacteric women, possibly via chronic inflammation, hormonal factors related to menopause and dyslipidemia.