Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):531-537
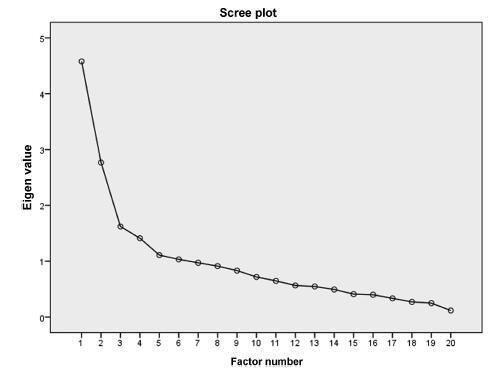
To analyze the internal consistency and the construct validity of the State-Trait Anxiety Inventory (STAI) State-Anxiety (S-Anxiety) scale for pregnant women during labor.
A study of measurement property including 150 pregnant women aged between 15 and 45 years old, during the first period of labor and with term pregnancies. The questionnaire used was the STAI S-Anxiety scale. In order to assess the internal consistency, Cronbach’s α was calculated through an exploratory factor analysis. The correlation between the factors was calculated using the Pearson coefficient. The state of significance used for this analysis was 0.05.
The STAI S-Anxiety scale used in the context of labor showed two factors represented as the absence (factor 1) and the presence of anxiety (factor 2); item 4 (“I regret it”) did not show a representative value. Both factors showed high indications of Cronbach’s α, varying from 0.830 for factor 1, and 0.723 for factor 2. In the results of the Pearson coefficient between the two factors, a significant but weak correlation was observed (r = -0.188; p = 0.021).
The STAI S-Anxiety scale used in pregnant women during labor presented appropriate values of internal consistency; however, item 3 did not show a significant factorial value. Therefore, this questionnaire must be applied cautiously and carefully without the use of the item 4 in the clinical practice and in researches about labor.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):538-544
Toxoplasmosis a parasitic zoonosis of global distribution, responsible for disorders during gestation can cause fetal death or congenital anomalies.
To evaluate the knowledge of toxoplasmosis among pregnant and postpartum women treated at the University Hospital of the city of Rio Grande, Rio Grande do Sul, Brazil.
This was a cross-sectional study of 100 pregnant and postpartum women at the University Hospital. Participants answered a self-administered questionnaire and gave consent for data relating to serological examinations to be abstracted from their medical records.
The proportion of women who received information about toxoplasmosis was higher among those who received care in the private health care system (52.9%) than among those cared for in the public health care system (25.0%). Only 55.7% of women reported having some knowledge about toxoplasmosis. Of these, 53.7% received information during the prenatal period. However, most participants were unable to answer questions about preventive measures and modes of infection. Of the 100 patients in the study, only 46 underwent serologic testing for toxoplasmosis, 65.2% of whom tested negative (IgG).
Findings from this study are relevant to the training of health professionals regarding toxoplasmosis education and prevention. Improved education for health care providers and patients can lead to earlier diagnoses and reductions in adverse outcomes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):545-551
To determine methods of contraception used by adolescents before and after pregnancy.
A cross-sectional study was performed, and data were collected from medical records of all teens in puerperal consultation at the Hospital da Mulher - José Aristodemo Pinotti (Caism), Universidade Estadual de Campinas (CAISM), São Paulo, Brazil, between July 2011 and September 2013. The inclusion criterionwas being 10 to 19 years old, and the exclusion criterion was having a first consultation 90 days after childbirth. Statistical analyseswere performed with averages, standard deviations, percentages, correlations and Fisher's exact tests using the SAS program, version 9.4.
A total of 196 adolescents in postpartum consultation were included (44 days after childbirth on average). The majority was older than 14 years (89%), with an average age of 16.2 years, and the most were exclusively breast-feeding (70%). Before pregnancy, the use of any contraceptive methods was mentioned by 74% adolescents; the most frequent use was combined oral contraceptive followed by condom. The main reason for abandoning the use of contraception was the occurrence of an unintended pregnancy (41%), followed by reports of side effects (22%), behavior issues (18%) and desire for pregnancy (16%). A positive correlation was found between the age of the adolescent at the moment of childbirth, the age of menarche (r = 0.3), and the first sexual intercourse (r = 0.419). Vaginal delivery occurred in 76% of the cases. After birth, depot medroxyprogesterone acetate (DMPA) was the contraception method most frequently used (71%), followed by oral contraceptives (11.8%) and intrauterine devices (IUDs, 11.2%).
The most prescribed contraceptive method before pregnancy in adolescents who had childbirth was combined oral contraceptives. Many of the study participants had an unintended pregnancy. After childbirth, the most used contraceptive method was DMPA. To improve contraception and reduce the chance of unintended pregnancies among adolescents, we should promote the use of long-acting reversible contraceptives (LARCS).
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):552-558
Whether preconception elevated concentrations of thyroid-stimulating hormone (TSH) compromises reproductive outcomes in patients undergoing assisted reproduction techniques (ARTs) remains unclear. This study therefore compared the reproductive outcomes in patients with TSH concentrations of < 2.5 mIU/L, 2.5-4.0 mIU/L, and 4.0-10.0mIU/L undergoing controlled ovarian stimulation (COS) for in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI).
This retrospective cohort study evaluated the medical records of all women with measured TSH concentrations who underwent IVF/ICSI between January 2011 and December 2012. The patients were divided into three groups: TSH < 2.5mIU/L (group 1); THS ≥2.5 and < 4.0 mIU/L (group 2); and THS ≥4 mIU/L and < 10.0 mIU/L (group 3). Patients who were administered levothyroxine for treating hypothyroidism were excluded from the analysis. The primary endpoints were clinical pregnancy,miscarriage, live birth and multiple pregnancy rates.
During the study period, 787 women underwent IVF/ICSI. Sixty were excluded because their TSH concentrations were unavailable, and 77 were excluded due to their use of levothyroxine. The prevalence of patients presenting elevated concentrations of TSHwas of 5.07% (using a TSH threshold of 4.0 mIU/L) and of 29.99% (using a TSH threshold of 2.5 mIU/L). Patient characteristics, type of COS, and response to COS did not differ among the three groups, and there were no differences in clinical pregnancy (24.4% versus 25.9% versus 24.2%, p = 0.93); miscarriage (17.1% versus 14.3% versus 12.5%, p = 0.93); live birth (20.2% versus 22.2% versus 21.2%, p = 0.86); and multiple pregnancy rates (27.0% versus 21.4% versus 25.0%, p = 0.90) respectively.
Response to COS, live birth, and miscarriage rates were not altered in women with elevated concentrations of TSH undergoing IVF/ICSI, regardless of using a TSH threshold of 2.5mIU/L or 4.0mIU/L. These findings reinforce the uncertainties related to the impact of subclinical hypothyroidism on reproductive outcomes in women undergoing COS for ARTs.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(11):559-563
To identify pregnancy as a causative factor of sexual dysfunction among expectant women.
A prospective study with 225 expectant mothers seen in the prenatal clinic of a federal university. Sexual function was evaluated by means of the Female Sexual Function Index (FSFI), and all domains were analyzed (desire, arousal, lubrication, orgasm, satisfaction, and pain). Initially, a univariate analysis of the sample was done. The averages for each domain according to the risk of sexual dysfunction (FSFI ≤ 26.5) were compared using the Student’s t-test for independent samples. The strength of the correlation between sexual dysfunction and all sociodemographic, clinical and behavioral variables was measured by the Chi-Square (X2) test. Then, odds ratios (ORs) and their confidence intervals were assigned to perform a bivariate analysis. Any p values less than 0.05 were considered significant.
Approximately two-thirds of the women (66.7%) showed signs of risk of sexual dysfunction (FSFI ≤ 26.5). Within these cases, all sexual dysfunction domains (desire, arousal, lubrication, orgasm, satisfaction, and pain) were found to be statistically significant (p < 0.001). The domains most affected were desire (2.67), satisfaction (2.71) and arousal (2.78).
Pregnancy appears to be an important causative factor of sexual dysfunction among pregnant women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):373-380
The placenta, translates how the fetus experiences the maternal environment and is a principal influence on birth weight (BW).
To explore the relationship between placental growth measures (PGMs) and BW in a public maternity hospital.
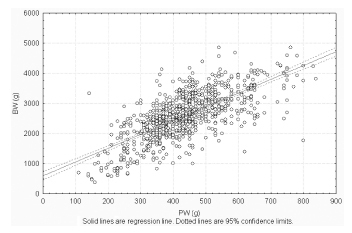
Observational retrospective study of 870 singleton live born infants at Hospital Maternidad Sardá, Universidad de Buenos Aires, Argentina, between January 2011 and August 2012 with complete data of PGMs. Details of history, clinical and obstetrical maternal data, labor and delivery and neonatal outcome data, including placental measures derived from the records, were evaluated. The following manual measurements of the placenta according to standard methods were performed: placental weight (PW, g), larger and smaller diameters (cm), eccentricity, width (cm), shape, area (cm2), BW/PW ratio (BPR) and PW/BW ratio (PBR), and efficiency. Associations between BW and PGMs were examined using multiple linear regression.
Birth weight was correlated with placental weight (R2 =0.49, p < 0.001), whereas gestational age was moderately correlated with placental weight (R2 =0.64, p < 0.001). By gestational age, there was a positive trend for PW and BPR, but an inverse relationship with PBR (p < 0.001). Placental weight alone accounted for 49% of birth weight variability (p < 0,001), whereas all PGMs accounted for 52% (p < 0,001). Combined, PGMs, maternal characteristics (parity, pre-eclampsia, tobacco use), gestational age and gender explained 77.8% of BW variations (p < 0,001). Among preterm births, 59% of BW variances were accounted for by PGMs, compared with 44% at term. All placental measures except BPR were consistently higher in females than in males, which was also not significant. Indices of placental efficiency showed weakly clinical relevance.
Reliable measures of placental growth estimate 53.6% of BW variances and project this outcome to a greater degree in preterm births than at term. These findings would contribute to the understanding of the maternal-placental programming of chronic diseases.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):381-390
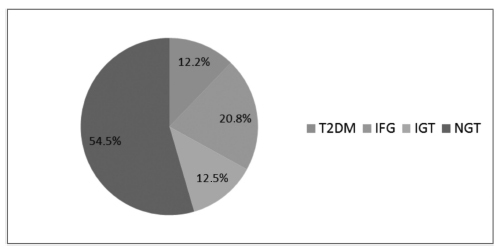
The aims of the study were to evaluate, after pregnancy, the glycemic status of women with history of gestational diabetes mellitus (GDM) and to identify clinical variables associated with the development of type 2 diabetes mellitus (T2DM), impaired fasting glucose (IFG), and impaired glucose tolerance (IGT).
Retrospective cohort of 279 women with GDM who were reevaluated with an oral glucose tolerance test (OGTT) after pregnancy. Characteristics of the index pregnancy were analyzed as risk factors for the future development of prediabetes (IFG or IGT), and T2DM.
T2DM was diagnosed in 34 (12.2%) patients, IFG in 58 (20.8%), and IGT in 35 (12.5%). Women with postpartum T2DM showed more frequently a family history of T2DM, higher pre-pregnancy body mass index (BMI), lower gestational age, higher fasting and 2-hour plasma glucose levels on the OGTT at the diagnosis of GDM, higher levels of hemoglobin A1c, and a more frequent insulin requirement during pregnancy. Paternal history of T2DM (odds ratio [OR] =5.67; 95% confidence interval [95%CI] =1.64-19.59; p =0.006), first trimester fasting glucose value (OR =1.07; 95%CI =1.03-1.11; p =0.001), and insulin treatment during pregnancy (OR =15.92; 95%CI =5.54-45.71; p < 0.001) were significant independent risk factors for the development of T2DM.
A high rate of abnormal glucose tolerance was found in women with previous GDM. Family history of T2DM, higher pre-pregnancy BMI, early onset of GDM, higher glucose levels, and insulin requirement during pregnancy were important risk factors for the early identification of women at high risk of developing T2DM. These findings may be useful for developing preventive strategies.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(8):391-398
This study was conducted to determine the seroprevalence of HIV among pregnant women in Brazil and to describe HIV testing coverage and the uptake of antenatal care (ANC).
Between October 2010 and January 2012, a probability sample survey of parturient women aged 15-49 years who visited public hospital delivery services in Brazil was conducted. Data were collected from prenatal reports and hospital records. Dried blood spot (DNS) samples were collected and tested for HIV.We describe the agespecific prevalence of HIV infection and ANC uptake with respect to sociodemographic factors.
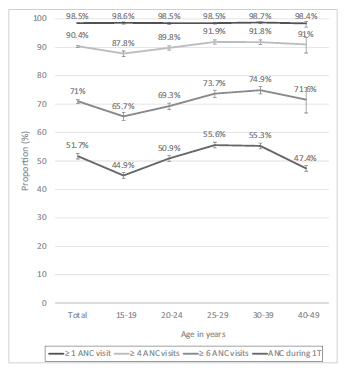
Of the 36,713 included women, 35,444 (96.6%) were tested for HIV during delivery admission. The overall HIV prevalence was of 0.38% (95% confidence interval [CI]: 0.31-0.48), and it was highest in: the 30 to 39 year-old age group (0.60% [0.40- 0.88]), in the Southern region of Brazil (0.79% [0.59-1.04]), among women who had not completed primary (0.63% [0.30-1.31]) or secondary (0.67% [0.49-0.97]) school education, and among women who self-reported as Asian (0.94% [0.28-3.10]). The HIV testing coverage during prenatal care was of 86.6% for one test and of 38.2% for two tests. Overall, 98.5% of women attended at least 1 ANC visit, 90.4% attended at least 4 visits, 71% attended at least 6 visits, and 51.7% received ANC during the 1st trimester. HIV testing coverage and ANC uptake indicators increased with increasing age and education level of education, and were highest in the Southern region.
Brazil presents an HIV prevalence of less than 1% and almost universal coverage of ANC. However, gaps in HIV testing and ANC during the first trimester challenge the prevention of the vertical transmission of HIV. More efforts are needed to address regional and social disparities.