Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(12):800-802
To describe a case of radiation-induced uterine carcinosarcoma 6 years after a cervical squamous cell carcinoma treatment, which imposed some diagnostic and management challenges.
A 57-year-old woman with a history of pelvic chemoradiotherapy ~ 6.5 years before the event described in this study, following an International Federation of Gynecology and Obstetrics (FIGO) stage IIB cervical cancer, presented with a cervical mass, involving the uterine cavity, the cervical canal and the upper two thirds of the vagina. The biopsy showed a poorly differentiated carcinoma, and a positron emission tomography (PET) scan excluded distant metastasis, although it was unable to define the origin of the tumor as either a new primary malignancy of the endometrium/cervix or as a cervical recurrence. Surgical staging procedure was performed, and the diagnosis was endometrial carcinosarcoma, FIGO stage IIB. The patient was not able to complete the adjuvant therapy, and the progression of the disease was remarkable.
The present case highlights one of the less common but more serious consequences of radiotherapy for cervical cancer, which has an increasing incidence in younger women, raising concerns about the long-termconsequences of its management.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(6):285-289
DOI 10.1590/S0100-72032012000600008
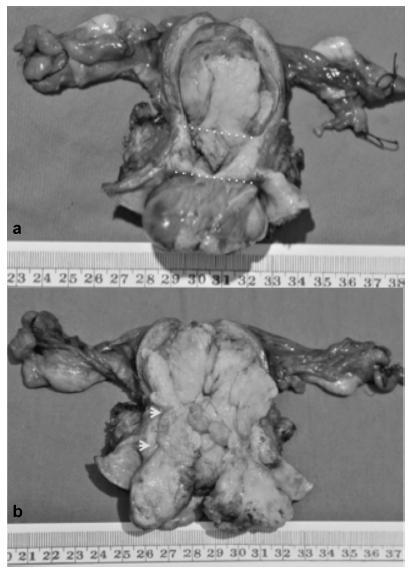
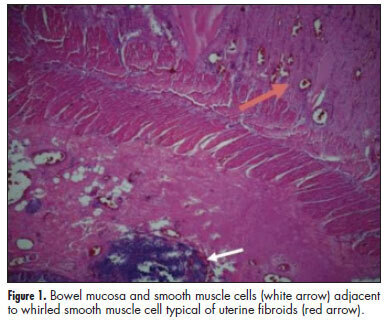
Extrauterine leiomyomas are rare, benign, and may arise in any anatomic sites. Their unusual growth pattern may even mimic malignancy and can result in a clinical dilemma. Occasionally, uterine leiomyomas become adherent to surrounding structures. They also develop an auxiliary blood supply, and lose their original attachment to the uterus, thus becoming 'parasitic'. Parasitic myomas may also be iatrogenically created after uterine fibroid surgery, particularly if morcellation is used. This report presented two cases of parasitic myomas with sepsis, both requiring right hemicolectomy. It reviewed the pertinent literature.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(8):201-206
DOI 10.1590/S0100-72032011000800006
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(3):128-132
DOI 10.1590/S0100-72032011000300005
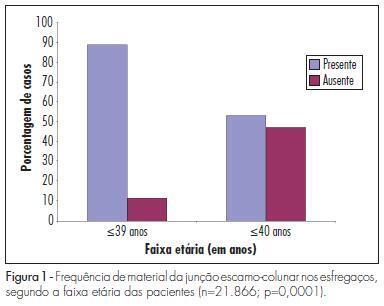
PURPOSE: to evaluate the frequency of cells of the cervical transitional zone (CTZ) in cervicovaginal smears of women older than 40 years. METHODS: we conducted a retrospective study with review of 24,316 Pap smear reports during the period from January 2005 to December 2008, to evaluate the cases without material of the CTZ. Exclusion criteria were: total hysterectomy, smears with severe atrophy or unsatisfactory for analysis, cases without visualization of the cervix or the external orifice of the cervix closed during examination and records without the patient's age. A total of 21,866 cervical-vaginal cytology reports were included in this study. We evaluated the relationship between the presence of material of the CTZ and use of hormone replacement therapy (HRT) in patients aged 40 years or more and the relationship between presence of material of the CTZ and a moderate to intense inflammatory process in patients aged 39 years or less. Data were analyzed statistically by the χ2 test and Odds Ratio. RESULTS: only 11.2% of patients younger than 40 years had no material from the CTZ in their smears, while 47% patients older than 40 years had no material from the CTZ (p=0.0001). Most patients aged 40 years or more (92.1%) did not use HRT and this was not a predictor of incidence of CTZ material in these patients (p> 0.05). In contrast, most patients younger than 40 years without CTZ material (74.5%) had abundant inflammation in the smears (p=0.0001). CONCLUSION: patients aged 40 years or more had a lower incidence of material from the CTZ in cervicovaginal smears, and inflammation was a factor that contributed to the absence of CTZ material in the smears from patients younger than 40 years.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(10):476-485
DOI 10.1590/S0100-72032010001000002
PURPOSE: to analyze the characteristics of viral infection and the risk factors for high-grade squamous intraepithelial lesion and cervical carcinoma in women with cervical HPV infection. METHODS: a case-control study was conducted on women with cervical HPV at a Gynecology reference service enrolled at the Public Health System, located in Recife, Northeastern Brazil. The groups of cases (72 women with high-grade squamous intraepithelial lesion or cervical cancer) and controls (176 women with normal Pap smear or benign alterations) were investigated for six viral genotypes (HPV 16, 18, 31, 33, 6, 11) in ecto- and endocervical material using MY09/MY11 primers. The independent variables were ranked in three levels of determination: distal (sociodemographic), intermediate (behavioral) and proximal (previous Pap smear). The homogeneity of proportions was tested (χ2), unadjusted Odds Ratios (OR) were obtained and hierarchical logistic regression was applied to the final model, with adjustment of the effect of each variable to the outcome based on the variables in the same and previous levels of causality. RESULTS: the viral genotype of cervical infection was identified in 76.6% of the 248 women participating in the study. High-risk HPV genotypes (83.4% of cases and 67.1% of controls) were predominant, especially HPV 16 and 31. The distal risk factors identified were: living in a rural area (OR=2.71, 95%CI: 1.18-6.23), less than three years of study (OR=3.97, 95%CI: 2.09-7.54) and family income below two minimum wages (OR=3.30, 95%CI: 1.04-10.51); intermediate: four or more pregnancies (OR=2.00, 95%CI: 1.06-3.76); and proximal: absence of a previous Pap smear (OR=9.74, 95%CI: 2.48-38.28). CONCLUSIONS: genotypes 16 and 31 of cervical HPV infection are predominant among women assisted by the Public Health System in Northeastern Brazil. Socioeconomic and reproductive factors, as well as the absence of cytological screening, represent risk factors for the progression of infection to high-grade squamous intraepithelial lesion and cervical cancer.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(12):598-603
DOI 10.1590/S0100-72032009001200004
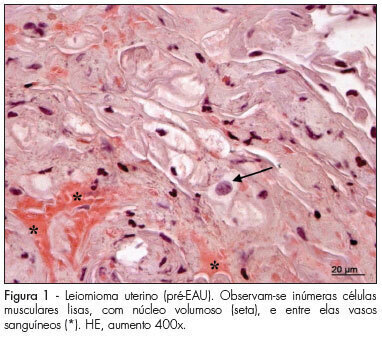
PURPOSE: to analyze histomorphometric consequences of the uterine arteries embolization (UAE) in the uterine tissue, especially by collagen tissue quantification through uterine biopsy, before and after treatment of uterine leiomyoma. METHODS: 15 patients with symptomatic leyomioma and/or infertility, submitted to UAE, participated in the study according to the study exclusion criteria, after having signed an informed consent. Uterine biopsy was performed in the secretory phase of the menstrual cycle, before and three months after the procedure, to evaluate the collagen. After the histological processing of the material, 3 µ slices were prepared, some of them dyed with hematoxiline-eosin (HE) and others with the specific dye for collagen fibers (Picrosirius red). Then, the slides were examined and interpreted, and the collagen quantified. The amount was calculated as the percent of the area composed by collagen, and the result expressed in mean±standard deviation (SD). Data has then been submitted to statistical analysis by Student's paired t test (p<0.05). RESULTS: the presence of smooth muscle cells was observed in the biopsies performed before the treatment, surrounded by a rich network of collagen fibers, which are part of the tumor, blood vessels and fibroblast nuclei. On the slides of biopsies performed after the treatment, it was observed the presence of widespread coagulation necrosis, vascular thrombosis, calcification and lymphoplasmocitary infiltration areas and clear reduction of the collagen component. The percentage of collagen fibers was higher in the pre-UAE group (84.07±1.41), than in the post-UAE (81.05±1.50) group, with p<0.0001, and 95% confidence interval (CI95%) from 2.080 to 3.827. CONCLUSION: the quantitative and qualitative collagen reduction clearly shows that the proposed treatment is efficient in reducing the tumoral mass, composed mainly by collagen fibers intermingled with neoplasic smooth muscle cells. Nevertheless, complementary studies are needed to investigate the functional and biological consequences of these histological changes.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(8):411-414
DOI 10.1590/S0100-72032009000800007
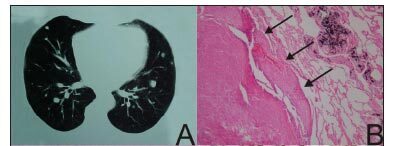
Benign metastazing leiomyomatosis (BML) is a rare disease in which the lung is the most affected extra-uterine organ. The BML histology is compatible with benignity and similar to that found in the myometrial leiomyoma. A history of surgically treated uterine myomatosis is reported by most of the patients with metastatic disease. We report the cases of two patients with uterine metastazing leiomyomatosis. In the first case, a 55-year-old patient presented lung nodes over 20 years after being submitted to hysterectomy due to uterine leiomyoma. The histological and immunohistochemical studies from the lung node revealed that it was an implant of benign leiomyoma. The second patient, a 65-years-old woman, presented lung and retroperitoneal nodes 20 years after being submitted to a hysterectomy due to uterine leiomyoma.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(5):248-255
DOI 10.1590/S0100-72032008000500007
PURPOSE: to describe the socio-demographic characteristics of deaths caused by uterine cervix cancer in women living in Recife, Pernambuco, Brazil, from 2000 to 2004. METHODS: a transversal populational study, including 323 deaths by uterine cervix cancer, among which 261 were recorded in the Information System about Mortality and 62 were identified after investigation on deaths by cancer at non-specified sites of the uterus. Mortality rate for all the variables was obtained and statistics for central tendency and variance were calculated. The χ2 test was performed to obtain the mortality coefficient concerning the living place and age range of the patients. RESULTS: death among women under 60 (54.7%), black (60.5%), single (67.6%), housewives (71.2%) and the ones living in poor neighborhood (53.3%) preponderated. Most of deaths occurred in hospitals (85.1%) and 90.2% of them occurred inside national health system hospitals. The mortality coefficient varied from 0.3 (among women under 30) to 54.9/100.00 (among women over 80). Significant statistical differences (p<0.05) were evidenced when death linked to age range and sanitary district was compared to characteristics of the female population living in the city. CONCLUSIONS: in Recife, death by cervix cancer are more frequent among adult, black, single, housewives, women living in poor neighborhoods and attended to at national health system hospitals, with differences in death risk among age ranges and living place.