-
Original Article08-01-2015
Waiting time for the first colposcopic examination in women with abnormal Papanicolaou test
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(8):381-387
Abstract
Original ArticleWaiting time for the first colposcopic examination in women with abnormal Papanicolaou test
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(8):381-387
DOI 10.1590/SO100-720320150005393
Views128PURPOSE:
To evaluate the waiting times before obtaining the first colposcopic examination for women with abnormal Papanicolaou smears.
METHODS:
Retrospective cohort study conducted on patients who required a colposcopic examination to clarify an abnormal pap test, between 2002 January and 2008 August, in a metropolitan region of Brazil. The waiting times were defined as: Total Waiting Time (interval between the date of the pap test result and the date of the first colposcopic examination); Partial A Waiting Time (interval between the date of the pap test result and the date of referral); Partial B Waiting Time (interval between the date of referral and the date of the first colposcopic examination). Means, medians, relative and absolute frequencies were calculated. The Kruskal-Wallis test and Pearson's chi-square test were used to determine statistical significance.
RESULTS:
A total of 1,544 women with mean of age of 34 years (SD=12.6 years) were analyzed. Most of them had access to colposcopic examination within 30 days (65.8%) or 60 days (92.8%) from referral. Mean Total Waiting Time, Partial A Waiting Time, and Partial B Waiting Time were 94.5 days (SD=96.8 days), 67.8 days (SD=95.3 days) and 29.2 days (SD=35.1 days), respectively.
CONCLUSION:
A large part of the women studied had access to colposcopic examination within 60 days after referral, but Total waiting time was long. Measures to reduce the waiting time for obtaining the first colposcopic examination can help to improve the quality of care in the context of cervical cancer control in the region, and ought to be addressed at the phase between the date of the pap test results and the date of referral to the teaching hospital.
Key-words Appointments and schedulesColposcopyPapanicolaou testReferral and consultationUterine cervical neoplasmsWaiting listsSee more -
Original Article12-01-2014
Recurrent cervical cancer: symptoms at diagnosis are related to a worse prognosis?
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):569-574
Abstract
Original ArticleRecurrent cervical cancer: symptoms at diagnosis are related to a worse prognosis?
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(12):569-574
DOI 10.1590/SO100-720320140005068
Views187See morePURPOSE:
The aim of this study was to evaluate the clinical features and prognostic implications of patients with recurrent cervical cancer.
METHODS:
By reviewing the medical records we evaluated all patients with cervical cancer at stages IA to IVA who started treatment at a specialized hospital in the Southeast region of Brazil from 2007 to 2009. Recurrence episodes were categorized according to location of disease and information was collected regarding the type of treatment and survival of these patients. The sample was characterized by descriptive statistics and association analyses were performed using Fisher's exact test.
RESULTS:
Fifty cases of recurrence were identified among 469 selected records, with 31 patients being symptomatic at diagnosis of recurrence (62%); and 19 being asymptomatic (38%). Among women with symptoms, eight requested anticipation of the previously scheduled appointment because of the presence of clinical complaints. Patients with symptoms at the diagnosis of recurrence had lower rates of overall two-year survival (39.4 versus 67.6%) (p=0.081). None of the patients with recurrence at distance received curative intent treatment, but all received surgical treatment or radiotherapy aiming at full remission of the disease. Women who requested anticipation of the appointment because of the presence of symptoms had a significant reduction of overall two-year survival after recurrence (0 versus 60.4%; p<0.001) compared to those who attended the consultation on the scheduled date, and none of them received curative intent treatment. As expected, the patients who underwent palliative treatment with the main objective of improving quality of life and increasing survival but with no perspective of cure had a significant reduction in overall survival compared to those who were treated with curative intent (76.7 versus 35.4%; p<0.001).
CONCLUSION:
The benefit of detecting asymptomatic recurrence of cervical cancer has the potential to improve the prognosis of patients with local and regional recurrence, but studies on larger series are necessary to confirm this possibility.
-
Original Article06-01-2014
Determinants of late stage diagnosis of cervical cancer in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(6):237-243
Abstract
Original ArticleDeterminants of late stage diagnosis of cervical cancer in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(6):237-243
DOI 10.1590/S0100-720320140005010
Views116See morePURPOSE:
To assess the determinants of late stage in women with cervical cancer in Brazil.
METHODS:
A cross-sectional study of secondary basis. Women with invasive cervical cancer enrolled in the Cancer Hospital Registry between January 2000 and December 2009 were included. Late clinical stage (≥IIB) was the outcome considered. The following variables were studied: age at diagnosis, race or ethnicity, years of education, marital status, alcohol consumption, smoking status, place of residence, year of diagnosis, initial treatment received, and status after the first treatment. Odds ratio (OR) with 95% confidence intervals (95%CI) and a logistic regression model were used. P values<0.05 were considered statistically significant.
Results:
37,638 cases were included, with a mean age of 52.4±14.1 years. Late clinical stages were observed in 70.6% of cases and were associated with the presence of squamous cell carcinoma (OR=1.8; 95%CI 1.7-2.0), age ≥50 years (OR=1.5; 95%CI 1.4-1.6), living with a partner (OR=1.3; 95%CI 1.2-1.4), black skin color (OR=1.2; 95%CI 1.1-1.4), and low educational level (OR=1.2; 95%CI 1.1-1.3).
CONCLUSION:
In Brazil, the diagnosis of cervical cancer is a delayed event. Although the main factor associated with late stage of cervical cancer identified in this study is a biological factors (histological type) and, consequently, not eligible for intervention, it was confirmed that socioeconomic disparities in the country are associated with late stage disease.
-
Original Article05-01-2014
PTEN expression in patients with carcinoma of the cervix and its association with p53, Ki-67 and CD31
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(5):205-210
Abstract
Original ArticlePTEN expression in patients with carcinoma of the cervix and its association with p53, Ki-67 and CD31
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(5):205-210
DOI 10.1590/S0100-7203201400050004
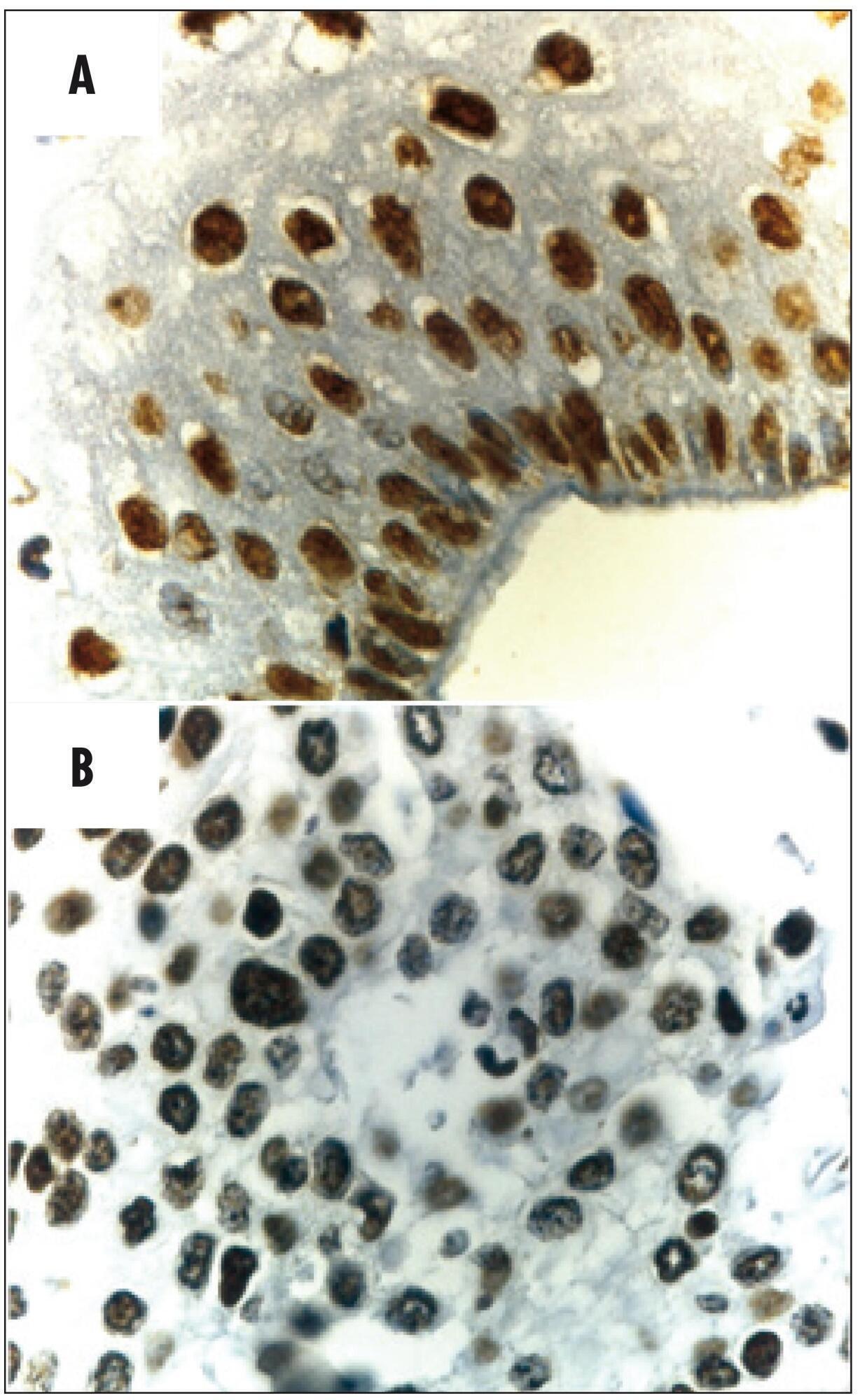
Views155See morePURPOSE:
To investigate protein expression and mutations in phosphatase and tensin homolog (PTEN) in patients with stage IB cervical squamous cell carcinoma (CSCC) and the association with clinical-pathologic features, tumor p53 expression, cell proliferation and angiogenesis.
METHODS:
Women with stage IB CSCC (n=20 - Study Group) and uterine myoma (n=20 - Control Group), aged 49.1±1.7 years (mean±standard deviation, range 27-78 years), were prospectively evaluated. Patients with cervical cancer were submitted to Piver-Rutledge class III radical hysterectomy and pelvic lymphadenectomy and patients in the Control Group underwent vaginal hysterectomy. Tissue samples from the procedures were stained with hematoxylin and eosin for histological evaluation. Protein expression was detected by immunohistochemistry. Staining for PTEN, p53, Ki-67 and CD31 was evaluated. The intensity of PTEN immunostaining was estimated by computer-assisted image analysis, based on previously reported protocols. Data were analyzed using the Student's t-test to evaluate significant differences between the groups. Level of significance was set at p<0.05.
RESULTS:
The PTEN expression intensity was lower in the CSCC group than in the Control (benign cervix) samples (150.5±5.2 versus 204.2±2.6; p<0.001). Our study did not identify any mutations after sequencing all nine PTEN exons. PTEN expression was not associated with tumor expression of p53 (p=0.9), CD31 (p=0.8) or Ki-67 (p=0.3) or clinical-pathologic features in patients with invasive carcinoma of the cervix.
CONCLUSIONS:
Our findings demonstrate that the PTEN protein expression is significantly diminished in CSCC.
-
Original Article05-01-2014
Why does the prevalence of cytopathological results of cervical cancer screening can vary significantly between two regions of Brazil?
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(5):192-197
Abstract
Original ArticleWhy does the prevalence of cytopathological results of cervical cancer screening can vary significantly between two regions of Brazil?
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(5):192-197
DOI 10.1590/S0100-7203201400050002
Views97See morePURPOSE:
To analyze the prevalence of cervical cytopathological results for the screening of cervical cancer with regard to women's age and time since the last examination in Maceió and Rio de Janeiro, Brazil, among those assisted by the Brazilian Unified Health System.
METHODS:
Cervical cytopathological results available in the Information System of Cervical Cancer Screening for the year 2011 were analyzed, corresponding to 206,550 for Rio de Janeiro and 45,243 for Maceió.
RESULTS:
In Rio de Janeiro, examination at one and two year intervals predominated, while in Maceió examination at one and three year intervals had a higher predominance. Women who underwent cervical smear screening in Maceió were older than those in Rio de Janeiro. The prevalence of invasive squamous cell carcinoma was similar for the two cities, but all the other results presented a higher prevalence in Rio de Janeiro: ASCUS (PR=5.32; 95%CI 4.66-6.07); ASCH (PR=4.27; 95%CI 3.15-5.78); atypical glandular cells (PR=10.02; 95%CI 5.66-17.76); low-grade squamous intraepithelial lesions (PR=6.10; 95%CI 5.27-7.07); high-grade squamous intraepithelial lesions (PR=8.90; 95%CI 6.50-12.18) and adenocarcinoma (PR=3.00; 95%CI 1.21-7.44). The rate of unsatisfactory cervical samples was two times higher in Maceió and that of rejected samples for analysis was five times higher in Maceió when compared to Rio de Janeiro.
CONCLUSIONS:
The prevalence rates of altered cervical cytopathological results was significantly higher in Rio de Janeiro than in Maceió. There is no objective information that may justify this difference. One hypothesis is that there may be a difference in the diagnostic performance of the cervical cancer screening, which could be related to the quality of the Pap smear. Thus, these findings suggest that it would be necessary to perform this evaluation at national level, with emphasis on the performance of cervical cancer screening in order to improve the effectiveness of cervical cancer control.
-
Original Article04-01-2014
Impact of training about cervical cancer screening on health professionals working in basic health care units
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(4):182-187
Abstract
Original ArticleImpact of training about cervical cancer screening on health professionals working in basic health care units
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(4):182-187
DOI 10.1590/S0100-7203201400040004
Views131PURPOSE:
To evaluate the impact of training professionals involved in the screening for cervical cancer in Basic Health Units in the city of Goiânia (GO).
METHODS:
This was and intervention study in which the following data contained in the cervical cytopathology test form were examined: the woman's personal data, anamnesis, clinical examination and identification of the professional responsible for the collection. Professional training was evaluated by comparing the forms referring to the period from January 2007 to April 2009, before training, with the forms referring to the period from July 2010 to December 2012, after training. The Pearson χ2 test was used to analyze the results of training, with the 5% level of significance.
RESULTS:
After training, there was a significantly increased frequency of recording patient schooling (from 67.2 to 92.6%, p<0.001), telephone number (from 78.9 to 98.7%, p<0.001), cervical inspection (from 86.8 to 96.6%, p<0.001), and signs suggestive of sexually transmitted diseases (from 80.8 to 93.5%, p<0.001). There was a reduction in the frequency of performing the exam within an interval of less than one year (p<0.001) and of one year (p<0.001). There was a reduction in the frequency of Pap smear testing in women under 25 years of age, from 22.0 to 17.9% (p<0.001). There was a significant increase in the proportion of satisfactory samples from 70.4 to 80.2% (p<0.001). A reduction of confounding factors was observed. The desiccation frequency was 2.9% before training and 2.0% after training (p<0.001). There was an increase in the frequency of representation of endocervical cells from 79.5 to 88.5% (p<0.001).
CONCLUSION:
After training, there was a significant improvement in completing the application form, the performance of such tests regarding frequency and the age range recommended by the Ministry of Health, and the adequacy of the sample.
Key-words Education, continuingHealth human resource trainingInservice trainingProfessional trainingUterine cervical neoplasmsSee more -
Original Article09-27-2013
Non adherence to cancer screening guidelines for cervical cancer among women who attended prenatal care
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(7):323-330
Abstract
Original ArticleNon adherence to cancer screening guidelines for cervical cancer among women who attended prenatal care
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(7):323-330
DOI 10.1590/S0100-72032013000700007
Views177See morePURPOSE: To estimate the prevalence and identify the factors associated with delayed pap smear test of the cervix (carried out more than three years ago) among mothers with sons under two years of age, who attended the prenatal care. METHODS: Cross-sectional, population-based household survey. Women with sons under two years old, living in the northern area of the city of Juiz de Fora (MG), Brazil, were interviewed. Stratification and clustering were used in a complex sampling procedure. We applied a survey questionnaire to capture women's demographic and socioeconomic characteristics of women and information about prenatal and practices for preventing cancer of the cervix. For statistical analysis of the possible bivariate association of factors, we used χ² test and a logistic regression model with the explanatory variables that had a significance less than or equal to 0.05 in the bivariate analysis. RESULTS: We found a delayed test prevalence of 26.6% (95%CI 21.3 - 32.6), including women who were never submitted to the exam. The variables associated with the non-adherence to the examination within the stipulated time were: to be married (OR 0.5; 95%CI 0.2 - 0.9), and divorced/widowed (OR 0.1; 95%CI 0.02 - 0,8), having performed gynecological examination in prenatal care (OR 0.3; 95%CI 0.1 - 0.6) and number of prenatal visits (OR 0.09; 95%CI 0.03 - 0.25 for more than 11 visits), being all protection factors. CONCLUSIONS: The prevalence of adherence to Pap smear guidelines is slightly lower than the percentage recommended by the World Health Organization. Apart from that, the fact that the woman was submitted to the prenatal care did not guarantee the adherence to Pap smear frequency guidelines.
-
Original Article12-20-2012
Pap smears among pregnant women in Southern Brazil: a representative cross-sectional survey
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(11):518-523
Abstract
Original ArticlePap smears among pregnant women in Southern Brazil: a representative cross-sectional survey
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(11):518-523
DOI 10.1590/S0100-72032012001100007
Views124PURPOSE: To determine the prevalence and risk factors associated with failure of voluntary screening for cervical cancer during the gestational period in Rio Grande, Rio Grande do Sul State, Southern Brazil. METHODS: Previously trained interviewers applied a standardized questionnaire in the maternity to all mothers from this municipality who had delivered from January 1st to December 31st 2010 to obtain information about the demographic characteristics of the pregnant women, family socioeconomic status, and prenatal care received. The χ² test was used to compare proportions and Poisson regression with robust adjustment of variance was used in the multivariate analysis. RESULTS: Among the 2,288 respondents, 33% were not submitted to the Pap smear during pregnancy. Two thirds of these women stated that they were not aware of the need to perform it, 18% were not screened out of fear or shame, and the rest for other reasons. After adjustment, the highest prevalence ratios (PR) for noncompliance with the Pap smear occurred among young women (PR=1.5; 95%CI 1.25 - 1.80), with lower educational level (PR=1.5; 95%CI 1.12 - 2.12), who were living without a partner (PR=1.4; 95%CI 1.24 - 1.62), smokers (PR=1.2; 95%CI 1.07 - 1.39), who did not plan the current pregnancy (PR=1.3; 95%CI 1,21 - 1.61), who had attended less than six medical visits during the prenatal period (PR=1.4; 95%CI 1.32 - 1.69) and among users of oral contraceptives (PR=1.2; 95%CI 1.04 - 1.38). CONCLUSIONS: The higher the risk for uterine cervical cancer, the less likely a pregnant woman is to undergo a Pap smear. This definitely contributed to the increased morbidity and mortality from this disease in this setting.
Key-words CytodiagnosisHealth services coverageMass screeningPregnant womenRisk factorsUterine cervical neoplasmsVaginal smearsSee more


