-
Original Article09-01-2016
Neurological Outcome in Fetuses with Mild and Moderate Ventriculomegaly
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):436-442
Abstract
Original ArticleNeurological Outcome in Fetuses with Mild and Moderate Ventriculomegaly
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):436-442
Views184See moreAbstract
Introduction
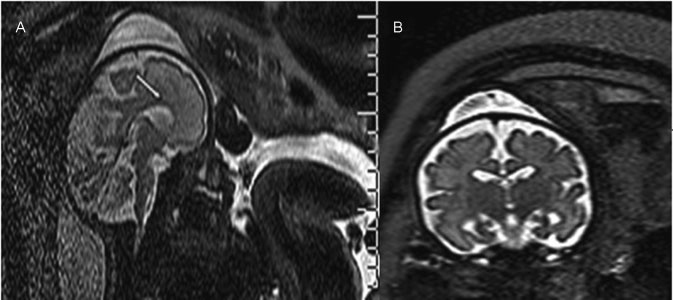
Ventriculomegaly (VM) is one the most frequent anomalies detected on prenatal ultrasound. Magnetic resonance imaging (MRI) may enhance diagnostic accuracy and prediction of developmental outcome in newborns.
Purpose
The aim of this study was to assess the correlation between ultrasound and MRI in fetuses with isolated mild and moderate VM. The secondary aim was to report the neurodevelopmental outcome at 4 years of age.
Methods
Fetuses with a prenatal ultrasound (brain scan) diagnosis of VM were identified over a 4-year period. Ventriculomegaly was defined as an atrial width of 10- 15 mm that was further divided as mild (10.1-12.0 mm) and moderate (12.1-15.0 mm). Fetuses with VM underwent antenatal as well as postnatal follow-ups by brain scan and MRI. Neurodevelopmental outcome was performed using the Griffiths Mental Development Scales and conducted, where indicated, until 4 years into the postnatal period.
Results
Sixty-two fetuses were identified. Ventriculomegaly was bilateral in 58% of cases. A stable dilatation was seen in 45% of cases, progression was seen in 13%, and regression of VM was seen in 4.5% respectively. Fetal MRI was performed in 54 fetuses and was concordant with brain scan findings in 85% of cases. Abnormal neurodevelopmental outcomes were seen in 9.6% of cases.
Conclusion
Fetuses in whom a progression of VM is seen are at a higher risk of developing an abnormal neurodevelopmental outcome. Although brain scan and MRI are substantially in agreement in defining the grade of ventricular dilatation, a low correlation was seen in the evaluation of VM associated with central nervous system (CNS) or non-CNS abnormalities.
-
Original Article07-01-2016
Epidemiological Risk Factors and Perinatal Outcomes of Congenital Anomalies
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):348-355
Abstract
Original ArticleEpidemiological Risk Factors and Perinatal Outcomes of Congenital Anomalies
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(7):348-355
Views236See moreAbstract
Objectives
To identify the epidemiological risk factors for congenital anomalies (CAs) and the impact of these fetal malformations on the perinatal outcomes.
Methods
This prospective cohort study comprised 275 women whose fetuses had CAs. Maternal variables to establish potential risk factors for each group of CA and perinatal outcomes were evaluated. The primary outcome was CA. Secondary outcomes included: fetal growth restriction (FGR); fetal distress (FD); premature rupture of membranes (PROM); oligohydramnios or polyhydramnios; preterm delivery (PTD); stillbirth; cesarean section; low birth weight; Apgar score < 7 at the 1st and 5th minutes; need for assisted ventilation at birth; neonatal infection; need for surgical treatment; early neonatal death; and hospitalization time. Chi-square (x2) test and multilevel regression analysis were applied to compare the groups and determine the effects of maternal characteristics on the incidence of CAs.
Results
The general prevalence of CAs was of 2.4%. Several maternal characteristics were associated to CAs, such as: age; skin color; level of education; parity; folic acid supplementation; tobacco use; and history of previous miscarriage. There were no significant differences among the CA groups in relation to FGR, FD, PROM, 1-minute Apgar score > 7, and need for assisted ventilation at birth. On the other hand, the prevalence of the other considered outcomes varied significantly among groups. Preterm delivery was significantly more frequent in gastrointestinal tract/abdominal wall defects. The stillbirth rate was increased in all CAs, mainly in isolated fetal hydrops (odds ratio [OR]: 27.13; 95% confidence interval [95%CI]: 2.90-253.47). Hospitalization time was higher for the urinary tract and congenital heart disease groups (p < 0.01). Neonatal death was significantly less frequent in the central nervous system anomalies group.
Conclusion
It was possible to identify several risk factors for CAs. Adverse perinatal outcomes were presented in all CA groups, and may differ according to the type of CA considered.
-
Case Report05-02-1998
Congenital parvovirus infection: case report
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(1):47-49
Abstract
Case ReportCongenital parvovirus infection: case report
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(1):47-49
DOI 10.1590/S0100-72031998000100008
Views100We report a case in which there was spontaneous regression of hydrops fetalis. Hydrops was probably caused by fetal infection with parvovirus B19. Anemia and hypokinesia of the heart were also observed. Diagnosis was accomplished by the ultrasound, virus detection in maternal serum, complete fetal blood count, and analysis of hepatic enzymes.
Key-words infection during pregnancynon-immune hydrops fetalisParvovirus B19prenatal diagnosisultrasoundSee more -
Original Article04-09-1998
Ultrasound screening for Down syndrome using a multiparameter score
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(9):525-531
Abstract
Original ArticleUltrasound screening for Down syndrome using a multiparameter score
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(9):525-531
DOI 10.1590/S0100-72031998000900006
Views139See morePurpose: to calculate sensitivity, specificity and positive and negative predictive values for multiparameter ultrasound scores for Down's syndrome. Patients and Methods: sensitivity and specificity for Down syndrome were calculated for ultrasound scores in a prospective study of ultrasound signs from 16 to 24 weeks in a high-risk population who denied invasive procedures after genetic counselling. The signs and scores were: femur/foot length < 0,9 (1), nuchal fold > 5 mm (2), pyelocaliceal diameter > 5 mm (1), nasal bones < 6 mm (1), absent or hypoplastic fifth median phalanx (1) and major structural malformations (2). Complete follow-up was obtained in each case. Genetic amniocentesis was proposed in the case of score 2 or more. Results: a total of 963 patients were examined from October 93 to December 97 at a mean gestational age of 19.6 (range 16 -24) weeks. Women's age ranged from 35 to 47 years (mean 38.8) and 18 Down syndrome cases were observed (1.8%). Sensitivity was 94.5% (17/18) for score 1 and 73% (13/18) for score 2 (false positive rate of 9.8% for score 1 and 4.1% for score 2). Individual sign sensitivity and specificity were: femur/foot = 16.7% (3/18) and 96.8% (915/945); nasal bones = 22.2% (4/18) and 92.1% (870/945); nuchal fold = 44.4% (8/18) and 96.5% (912/945); pyelic diameter = 38.9% (7/18) and 94.3% (891/945); absent phalanx = 22.2% (4/18) and 98.5% (912/945); malformation = 22.2% (4/18) and 98.2% (928/945). Conclusions: the overall sensitivity for score 1 was high but false positive rates were also high. For score 2, sensibility was still good (73%) and false positive rate was acceptable (4.1%). Positive and negative predictive values can be calculated for each prevalence (women's age). More cases are needed to reach final conclusions about this screening method (specially in a low-risk population) although this system has been useful for high-risk patients who deny invasive procedures.
-
Original Article03-15-1999
Biophysical triple test: a new ultrasonographic parameter for prognostic evaluation in early pregnancies
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(1):18-24
Abstract
Original ArticleBiophysical triple test: a new ultrasonographic parameter for prognostic evaluation in early pregnancies
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(1):18-24
DOI 10.1590/S0100-72031999000100004
Views133See morePurpose: it has been demonstrated that delays in gestational sac development, in crown-rump length and low embryonic heart rate could be indicators of poor pregnancy outcome. The purpose was to evaluate the use of these three parameters together, which we named Biophysical Triple Test (BTT). Method: thirty-five singleton pregnancies following IVF treatment with intracytoplasmatic sperm injection (ICSI) were studied. All ultrasonographic scans were performed by the same examiner, 4-5 weeks after embryo transference (6-7 week gestation), using a Diasonics equipment, model Synergy, with a 7.0-MHz transvaginal transducer. The gestational sac (GS) was measured at the longest transverse diameter; the crown-rump length (CRL) was measured at the sagittal plan and the embryonic heart rate (EHR) was calculated from frozen B and M-mode and Doppler. The statistical test used was Fisher's test. Results: the following parameters were considered abnormal: GS < 15.4 mm, CRL < 3.9 mm, EHR < 100 bpm. The parameters were calculated from the means less one standard deviation for the ongoing pregnancies. The patients with a positive BTT, i.e., with a high risk of miscarriage, were those with at least 2 altered parameters. In 35 pregnancies, a positive BTT was found in 5, all of those who miscarrided and 2 of those who had no miscarriage. The difference between the two groups was highly significant (p = 0.0015; t-Fisher). The sensitivity of the method was is 100%, with a specificity of 93.75 %, which resulted in a 96.87% efficacy. Conclusion: the BTT is an ultrasonographic noninvasive method that presents high efficacy as an indicator of poor pregnancy outcome.
-
Original Article03-13-1999
Transvaginal ultrasonography with color doppler to select the patients for conservative treatment of unruptured ectopic pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(3):153-157
Abstract
Original ArticleTransvaginal ultrasonography with color doppler to select the patients for conservative treatment of unruptured ectopic pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(3):153-157
DOI 10.1590/S0100-72031999000300006
Views115See morePurpose: to evaluate the efficacy of color Doppler in the prediction of results of the systemic treatment of unruptured ectopic pregnancy with a single dose of methotrexate. Methodology: twenty patients with a diagnosis of ectopic pregnancy were included in the study. The inclusion criteria were: hemodynamic stability, adnexal mass < 5.0 cm and decline of the titers of beta-hCG less than 15% in an interval of 24 h. The exclusion criteria were hepatic or renal disease and blood dyscrasias. Follow-up was by serial determinations of beta-hCG on days 4 and 7 after the beginning of the treatment, and weekly until the titers were negative. The patients were classified into 3 groups according to color Doppler: high risk (trophoblastic flow covering more than 2/3 of the mass), medium risk (when trophoblastic flow compromised 1/3 to 2/3 of tubal mass) and low risk (when trophoblastic flow covered less than 1/3 of the mass). Results: the success of the treatment with a single dose was 75% (15/20); when a second dose of MTX was used, the success rate was 85%. When comparing color Doppler with the results of the medical treatment, we had high risk in 4 patients and in all the treatment failed; medium and low risk in 16 patients, and in 15 the treatment was successful. Conclusion: color Doppler showing high risk indicated an unfavorable situation for the medical treatment with MTX, while medium and low risk in color doppler were favorable situations for the clinical treatment. However, these results should always be analyzed in association with the evolution curve of the beta-hCG titers.
-
Original Article05-22-1999
Evolution of Ultrasound Characteristics of Placenta and Fetal Position and Presentation in Normal Pregnancies.
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(9):499-504
Abstract
Original ArticleEvolution of Ultrasound Characteristics of Placenta and Fetal Position and Presentation in Normal Pregnancies.
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(9):499-504
DOI 10.1590/S0100-72031999000900002
Views129See morePurpose: to evaluate the ultrasound characteristics of normal pregnancies, according to the placental maturity, local of insertion and thickness, fetal presentation and position during the second half of pregnancy. Methods: a descriptive study was perfomed, including at least 120 measures in each gestational age, in 2,868 normal pregnant women from Campinas, Brazil, studied through routine obstetric ultrasound examinations, with fetal biometry and placental evaluation, applying Grannum, Berkowitz, Hobbins (1979) criteria for placental maturity. Placental thickness was measured at the cord insertion site. Results: grade 0 placentas were more frequent up to 31 weeks and grade I after 32 weeks. Grade II did not appear until 32 weeks and grade III was more frequent after 36 weeks. The placental thickness significantly increased with gestational age and the most frequent placental locations were anterior and posterior. The cephalic presentation was the most frequent all gestational ages, with only 1% of breech presentation at term. The most frequent fetal position was fetal spine left side, followed by right side. Conclusions: the studied factors showed a similar distribution to that expected for normal populations and could be used as a standard for the Brazilian population.
-
Original Article09-02-2004
The changing clinical presentation of molar pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(6):483-488
Abstract
Original ArticleThe changing clinical presentation of molar pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(6):483-488
DOI 10.1590/S0100-72032004000600010
Views80See moreOBJECTIVE: to determine whether the clinical presentation of hydatidiform mole has changed in the recent years (1992-1998) when compared with historic controls (1960-1981). METHODS: medical records of 80 patients with hydatidiform mole attended in the 1960-1981 period (Group I) were reviewed and compared to data from 801 patients followed in the 1992-1998 period (Group II). The clinical signals and symptoms analyzed were: age distribution, number of pregnancies, vaginal bleeding, hyperemesis, edema, hypertension, large uterus for gestation date and theca lutein cysts of the ovaries. Statistical analyses employed chi-square tests and odds ratio (OR) estimate with the confidence interval (CI) of 95%. RESULTS: concerning age, the disease occurred more frequently in group II than in group I, in patients under 15 and over 40 years old. As to the number of pregnancies, there was no statistical difference only in those patients who were in their third or fourth pregnancies. Arterial hypertension was the only symptom that occurred with similar frequency in both groups. Enlarged uterus was more frequent in group II (41.4 X 31.2% - p <0.05; OR: 1.5; IC: 1.0-2.3). Bleeding remained the most common symptom, occurring in 76.9% of patients (Group II), although it has occurred in 98.7% of the historic controls (p<0.05; OR: 0.04; IC: 0.03 0.04). The following symptoms were also less frequent in group II as compared to group I: hyperemesis (36.5% X 45% - p<0.05; OR: 0.7; IC: 0.4 0.9), edema (12.7% X 20% - p<0.05, OR: 0.5, IC: 0.3 0.8), enlarged uterus for gestational age (41.4% x 31.2% - p<0.05; OR: 1.5; IC: 1.0 2.3) and theca lutein cysts (16.4% X 41.2% - p<0.05; OR: 0.3; IC: 0.2 0.4). Ultrasound has become the commonest method of diagnosis (89.2% - p<0.05), allowing early detection of hydatidiform moles. CONCLUSION: there was a decrease of the traditional symptoms in current patients with hydatidiform mole as compared to historic controls, due to early diagnosis through ultrasonography.


