-
Original Article10-09-2023
Recommendations for the Screening of Breast Cancer of the Brazilian College of Radiology and Diagnostic Imaging, Brazilian Society of Mastology and Brazilian Federation of Gynecology and Obstetrics Association
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(8):480-488
Abstract
Original ArticleRecommendations for the Screening of Breast Cancer of the Brazilian College of Radiology and Diagnostic Imaging, Brazilian Society of Mastology and Brazilian Federation of Gynecology and Obstetrics Association
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(8):480-488
Views276See moreAbstract
Objective
To present the update of the recommendations of the Brazilian College of Radiology and Diagnostic Imaging, the Brazilian Society of Mastology and the Brazilian Federation of Associations of Gynecology and Obstetrics for breast cancer screening in Brazil.
Methods
Scientific evidence published in Medline, EMBASE, Cochrane Library, EBSCO, CINAHL and Lilacs databases between January 2012 and July 2022 was searched. Recommendations were based on this evidence by consensus of the expert committee of the three entities.
Recommendations
Annual mammography screening is recommended for women at usual risk aged 40–74 years. Above 75 years, it should be reserved for those with a life expectancy greater than seven years. Women at higher than usual risk, including those with dense breasts, with a personal history of atypical lobular hyperplasia, classic lobular carcinoma in situ, atypical ductal hyperplasia, treatment for breast cancer or chest irradiation before age 30, or even, carriers of a genetic mutation or with a strong family history, benefit from complementary screening, and should be considered individually. Tomosynthesis is a form of mammography and should be considered in screening whenever accessible and available.
-
Review Article01-23-2022
How to Reach the Best Ultrasound Performance in the Delivery Room
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(11):1070-1077
Abstract
Review ArticleHow to Reach the Best Ultrasound Performance in the Delivery Room
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(11):1070-1077
Views248See moreAbstract
Ultrasonography is an instrument that is present in the maternal-fetal assessment throughout pregnancy and with widely documented benefits, but its use in intrapartum is becoming increasingly relevant. From the assessment of labor progression to the assessment of placental disorders, ultrasound can be used to correlate with physiological findings and physical examination, as its benefit in the delivery room cannot yet be proven. There are still few professionals with adequate training for its use in the delivery room and for the correct interpretation of data. Thus, this article aims to present a review of the entire applicability of ultrasound in the delivery room, considering the main stages of labor. There is still limited research in evidence-based medicine of its various possible uses in intrapartum, but it is expected that further studies can bring improvements in the quality of maternal and neonatal health during labor.
-
Original Article05-18-2020
Frequency of Congenital Anomalies in the Brazilian Midwest and the Association with Maternal Risk Factors: Case-control Study
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(4):188-193
Abstract
Original ArticleFrequency of Congenital Anomalies in the Brazilian Midwest and the Association with Maternal Risk Factors: Case-control Study
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(4):188-193
Views169See moreAbstract
Objective
To evaluate the frequency of structural congenital anomalies (CAs) in the midwest of Brazil and its association with maternal risk factors.
Methods
This was a prospective, observational, case-control study based on a hospital population. Pregnant women attended at a fetal medicine service in Brazil were analyzed in the period from October 2014 to February 2016.A total of 357 pregnant women were included, 223 of whom had fetuses with structural anomalies (group case), and 134 of whom had structurally normal fetuses (control group). The clinical history was made previous to prenatal consultation, and the diagnosis of the structural CA was performed through ultrasound.
Results
A frequency of 64.27% (n = 223) of pregnant women with fetuses with structural anomalies was observed. The most frequent structural CAs were those of the central nervous system (30.94%), followed by anomalies of the genitourinary system (23.80%), and, finally, by multiple CAs (16.60%). The background of previous children with CAs (odds ratio [OR]: 3.85; p = 0.022), family history (OR: 6.03; p = < 0.001), and consanguinity between the progenitors (OR: 4.43; p = 0.034) influenced the occurrence of structural CA.
Conclusion
The most frequent CAs are those of the central nervous system, followed by those of the genitourinary system, and then multiple anomalies. The maternal risk factors that may have influenced the occurrence of structural CA were previous children with CA, family history, and consanguinity among the parents.
-
Original Article12-20-2019
Intraoperative Ultrasound Leads to Conservative Management of Benign Ovarian Tumors: A Retrospective, Single-Center Study
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(11):673-678
Abstract
Original ArticleIntraoperative Ultrasound Leads to Conservative Management of Benign Ovarian Tumors: A Retrospective, Single-Center Study
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(11):673-678
Views164See moreAbstract
Objective
To evaluate whether the use of intraoperative ultrasound leads to more conservative surgeries for benign ovarian tumors.
Methods
Women who underwent surgery between 2007 and 2017 for benign ovarian tumors were retrospectively analyzed. The women were classified into two groups: those who underwent intraoperative ultrasound (group A) and those who did not (group B). In group A, minimally-invasive surgery was performed for most patients (a specific laparoscopic ultrasound probe was used), and four patients were submitted to laparotomy (a linear ultrasound probe was used). The primary endpoint was ovarian sparing surgery (oophoroplasty).
Results
Among the 82 cases identified, only 36 met the inclusion criteria for the present study. Out of these cases, 25 underwent intraoperative ultrasound, and 11 did not. There were no significant differences in arterial hypertension, diabetes, smoking history, and body mass index for the two groups (p=0.450). Tumor diameter was also similar for both groups, ranging from 1 cm to 11 cm in group A and from 1.3 cm to 10 cm in group B (p=0.594). Tumor histology confirmed mature teratomas for all of the cases in group B and for 68.0% of the cases in group A. When the intraoperative ultrasound was performed, a more conservative surgery was performed (p<0.001).
Conclusion
The use of intraoperative ultrasound resulted in more conservative surgeries for the resection of benign ovarian tumors at our center.
-
Original Article04-15-2019
Assessment of Sensitivity and Specificity of Ultrasound and Magnetic Resonance Imaging in the Diagnosis of Placenta Accreta
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(1):17-23
Abstract
Original ArticleAssessment of Sensitivity and Specificity of Ultrasound and Magnetic Resonance Imaging in the Diagnosis of Placenta Accreta
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(1):17-23
Views268See moreAbstract
Objective
To assess and compare the sensitivity and specificity of ultrasonography and magnetic resonance imaging in the diagnosis of placenta accreta in patients with placenta previa.
Methods
This retrospective cohort study included 37 women, and was conducted between January 2013 and October 2015; 16 out of the 37 women suffered from placenta accreta. Histopathology was considered the gold standard for the diagnosis of placenta accreta; in its absence, a description of the intraoperative findings was used. The associations among the variables were investigated using the Pearson chi-squared test and the Mann-Whitney U-test.
Results
The mean age of the patients was 31.8 ± 7.3 years, the mean number of pregnancies was 2.8 ± 1.1, the mean number of births was 1.4 ± 0.7, and the mean number of previous cesarean sections was 1.2 ± 0.8. Patients with placenta accreta had a higher frequency of history of cesarean section than those without it (63.6% versus 36.4% respectively; p < 0.001). The mean gestational age at birth among women diagnosed with placenta previa accreta was 35.4 ± 1.1 weeks. The mean birth weight was 2,635.9 ± 374.1 g. The sensitivity of the ultrasound was 87.5%, with a positive predictive value (PPV) of 65.1%, and a negative predictive value (NPV) of 75.0%. The sensitivity of the magnetic resonance imaging was 92.9%, with a PPV of
Conclusion
The ultrasound and the magnetic resonance imaging showed similar sensitivity and specificity for the diagnosis of placenta accreta.
-
Original Article10-01-2018
Analysis of the Performance of 11 Formulae for Fetal Weight Estimation in Preterm Fetuses with Abnormal Doppler Velocimetry – A Retrospective Multicenter Study
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):580-586
Abstract
Original ArticleAnalysis of the Performance of 11 Formulae for Fetal Weight Estimation in Preterm Fetuses with Abnormal Doppler Velocimetry – A Retrospective Multicenter Study
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):580-586
Views205Abstract
Objective
To assess 11 formulae commonly used to estimate fetal weight in a population of premature fetuses who had abnormal Doppler velocimetry due to early-onset placental insufficiency. The performance of each formula was evaluated in subgroups of fetuses with expected growth and intrauterine growth restriction.
Methods
Data were collected fromfetuses andmothers who delivered at three Brazilian hospitals between November 2002 and December 2013.We used the following formulae: Campbell; Hadlock I, II, III, IV and V; Shepard; Warsof; Weiner I and II; and Woo III.
Results
We analyzed 194 fetuses. Of these, 116 (59.8%) were considered appropriate for gestational age (AGA), and 103 (53.1%) were male. The amniotic fluid volume was reduced in 87 (44.8%) fetuses, and the umbilical artery Doppler revealed absence or inversion of diastolic flow in 122 (62.9%) cases, and the analysis of the ductus venosus revealed abnormal flow in 60 (34.8%) fetuses. The Hadlock formulae using three or four fetal biometric parameters had low absolute percentage error in the estimated fetal weight among preterm fetuses with abnormal Doppler studies who were born within 5 days of the ultrasound evaluation. The results were not influenced by the clinical and ultrasound parameters often found in early-onset placental insufficiency.
Conclusion
In this study, the formulae with the best performance for fetal weight estimation in the analyzed population were Hadlock I and IV, which use four and three fetal biometric parameters respectively to estimate the weight of preterm fetuses with abnormal Doppler studies.
Key-words Birth weightDoppler ultrasoundFetal growth retardationFetal weightPlacental insufficiencyPremature birthprenatal ultrasoundultrasoundSee more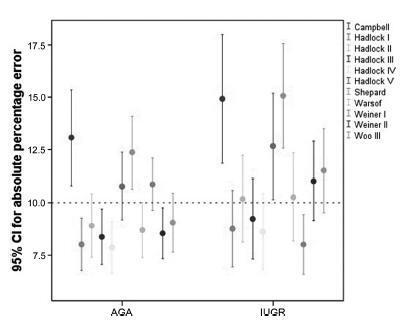
-
Original Article09-01-2017
Reference Ranges for Ultrasonographic Measurements of the Uterine Cervix in Low-Risk Pregnant Women
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(9):443-452
Abstract
Original ArticleReference Ranges for Ultrasonographic Measurements of the Uterine Cervix in Low-Risk Pregnant Women
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(9):443-452
Views280See moreAbstract
Objective
To define transvaginal ultrasound reference ranges for uterine cervix measurements according to gestational age (GA) in low-risk pregnancies.
Methods
Cohort of low-risk pregnantwomen undergoing transvaginal ultrasound exams every 4 weeks, comprisingmeasurements of the cervical length and volume, the transverse and anteroposterior diameters of the cervix, and distance fromthe entrance of the uterine artery into the cervix until the internal os. The inter- and intraobserver variabilities were assessed with the linear correlation coefficient and the Student t-test. Within each period of GA, 2.5, 10, 50, 90 and 97.5 percentiles were estimated, and the variation by GA was assessed with analysis of variance for dependent samples. Mean values and Student t-test were used to compare the values stratified by control variables.
Results
After confirming the high reproducibility of the method, 172 women followed in this cohort presented a reduction in cervical length, with an increase in volume and in the anteroposterior and transverse diameters during pregnancy. Smaller cervical lengths were associated with younger age, lower parity, and absence of previous cesarean section (C-section).
Conclusion
In the studied population, we observed cervical length shortening throughout pregnancy, suggesting a physiological reduction mainly in the vaginal portion of the cervix. In order to better predict pretermbirth, cervical insufficiency and premature rupture of membranes, reference curves and specific cut-off values need to be validated.

-
Original Article10-01-2016
Value of the Ultrasound in the Study of Ovarian Reserve for Prediction of Oocyte Recovery
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):499-505
Abstract
Original ArticleValue of the Ultrasound in the Study of Ovarian Reserve for Prediction of Oocyte Recovery
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(10):499-505
Views157See moreAbstract
Purpose
To identify which methods used in the assessment of the ovarian reserve are exclusive or complementary to identify the best response to follicle development.
Methods
Retrospective cohort study, involving patients undergoing assisted reproduction treatment at the Instituto de Medicina Reprodutiva e Fetal, from April 2009 to July 2014. Age, biochemical tests, and ultrasound were assessed. The data were analyzed to predict the follicular development and the relation between them, using, for statistical analysis, Statistical Package for Social Sciences software.
Results
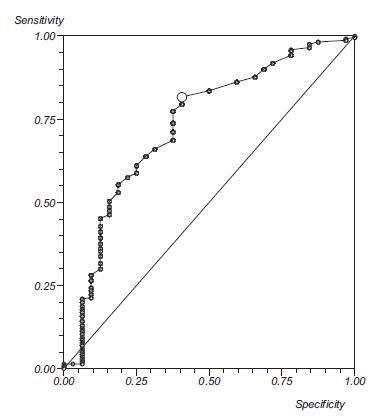
Out of the 293 couples included, 50.2% presented infertility by ovarian factor. Considering the age as the main variable, a significant negative correlation with the volume of both ovaries was observed (right ovary, r = 0.21; left ovary, r =0.22; both p< 0.0001), and with the antral follicle count (right ovary, r =0.38; left ovary, r =0.47; both p< 0.0001). Considering the antral follicle count as the main variable, a significant positive correlation with the total recruited oocytes was observed. When we correlated the antral follicle count with the recruited follicles larger than 18 mm, we observed that, with a cutoff of 12 antral follicles, there is a positive predictive value of 99%, and an area under the ROC curve of 0.76.
Conclusion
We concluded from our study that age and antral follicle count are effective predictors of ovarian response in cycles of assisted reproduction. The ovarian volume, as well as the anti-Müllerian hormone dosage, seem to be adequate markers of the ovarian reserve.