Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(4):435-441
Antenatal recognition of severe cases of congenital diaphragmatic hernia (CDH) by ultrasound (US) and magnetic resonance imaging (MRI) may aid decisions regarding the indication of fetal endoscopic tracheal occlusion.
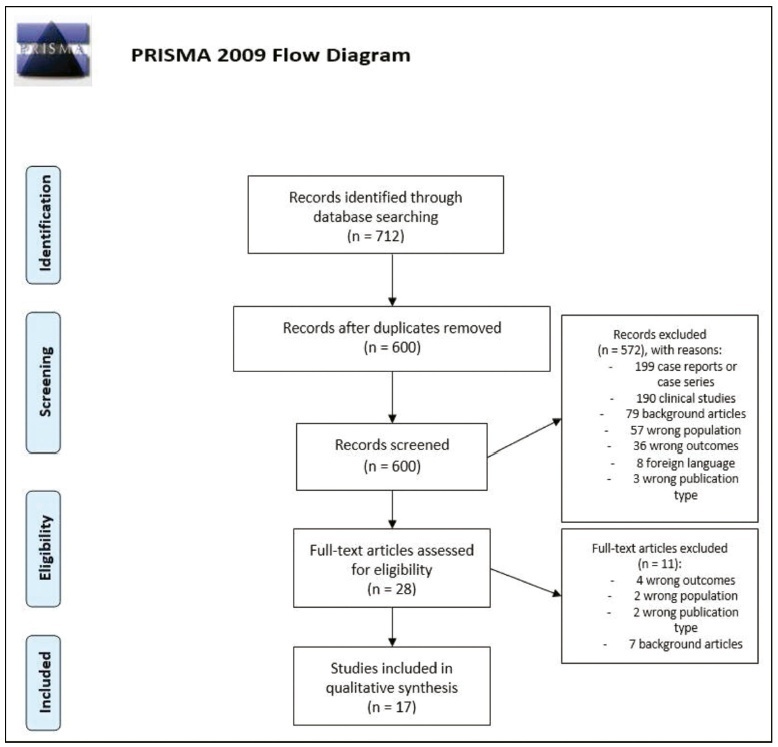
An integrative review was performed. Searches in MEDLINE and EMBASE used terms related to CDH, diagnosis, MRI, and US. The inclusion criteria were reviews and guidelines approaching US and MRI markers of severity of CDH published in English in the past 10 years.
The search retrieved 712 studies, out of which 17 publications were included. The US parameters were stomach and liver positions, lung-to-head ratio (LHR), observed/expected LHR (o/e LHR), and quantitative lung index. The MRI parameters were total fetal lung volume (TFLV), observed/expected TFLV, relative fetal or percent predicted lung volumes, liver intrathoracic ratio, and modified McGoon index. None of the parameters was reported to be superior to the others.
The most mentioned parameters were o/e LHR, LHR, liver position, o/e TFLV, and TFLV.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(10):455-459
DOI 10.1590/SO100-720320150005271
To analyze the obstetrical and neonatal outcomes of pregnancies with small for gestation age fetuses after 35 weeks based on umbilical cord nucleated red blood cells count (NRBC).
NRBC per 100 white blood cells were analyzed in 61 pregnancies with small for gestation age fetuses and normal Doppler findings for the umbilical artery. The pregnancies were assigned to 2 groups: NRBC≥10 (study group, n=18) and NRBC<10 (control group, n=43). Obstetrical and neonatal outcomes were compared between these groups. The χ2 test or Student's t-test was applied for statistical analysis. The level of significance was set at 5%.
The mean±standard deviation for NRBC per 100 white blood cells was 25.0±13.5 for the study group and 3.9±2.2 for the control group. The NRBC≥10 group and NRBC<10 group were not significantly different in relation to maternal age (24.0 versus 26.0), primiparity (55.8 versus 50%), comorbidities (39.5 versus55.6%) and gestational age at birth (37.4 versus 37.0 weeks). The NRBC≥10 group showed higher rate of caesarean delivery (83.3 versus 48.8%, p=0.02), fetal distress (60 versus 0%, p<0.001) and pH<7.20 (42.9 versus 11.8%, p<0.001). The birth weight and percentile of birth weight for gestational age were significantly lower on NRBC≥10 group (2,013 versus 2,309 g; p<0.001 and 3.8 versus 5.1; p=0.004; respectively). There was no case described of 5th minute Apgar score below 7.
An NRBC higher than 10 per 100 white blood cells in umbilical cord was able to identify higher risk for caesarean delivery, fetal distress and acidosis on birth in small for gestational age fetuses with normal Doppler findings.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(7):333-338
DOI 10.1590/S0100-720320150005373
To describe the prevalence of malformations found in fetuses with trisomy of chromosomes 13, 18 and 21 by identifying the most frequent within each condition.
A retrospective cross-sectional study with the analysis of trisomy cases of chromosomes 13, 18 and 21 diagnosed through fetal karyotype obtained by amniocentesis/cordocentesis, between October 1994 and May 2014, at a Teaching Hospital in Brazil Southern Region. Malformations identified through morphological ultrasonography were described and, subsequently, confirmed in newborn examinations and/or fetal autopsy. The results were analyzed using Fisher's test and analysis of variance (ANOVA), with a 5% level of significance (p=0.05).
Sixty-nine cases of trisomy were diagnosed among 840 exams; nine were excluded due to outcome outside Hospital de Clínicas de Porto Alegre or incomplete records, remaining 60 cases (nine cases of chromosome 13 trisomy, 26 of chromosome 18, and 25 of chromosome 21). In all three groups, heart disease occurred in most cases; the ventricular septal defect was more prevalent and occurred in 66.7% of the trisomy 13 group. Gastrointestinal abnormalities were more prevalent in the trisomy 18 group, especially omphalocele (38.5%; p<0.01). Genitourinary anomalies were more significantly frequent in the trisomy 13 group (pyelectasis, 55.6% - p<0.01; ambiguous genitalia, 33.3% - p=0.01). Central nervous system defects were identified in all cases of trisomy 13. Facial cracks were significantly more prevalent among fetuses with trisomy 13 (66.7%; p<0.01). Hand and feet malformations significantly differed among the trisomy groups. Hand defects occurred in 50% of trisomy 18 cases, and in 44.4% of all trisomy 13 cases (p<0.01); congenital clubfoot was more common in the trisomy 18 group, being detected in 46.2% of fetuses (p<0.01). The abnormalities were found in 50.9, 27.3 and 21.7% of trisomy 18, 13 and 21 cases respectively.
Many fetal malformations identified at ultrasound are suggestive of trisomy and represent an important tool for etiologic diagnosis and prenatal and pre-conception genetic counseling.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(6):264-268
DOI 10.1590/S0100-720320140004935
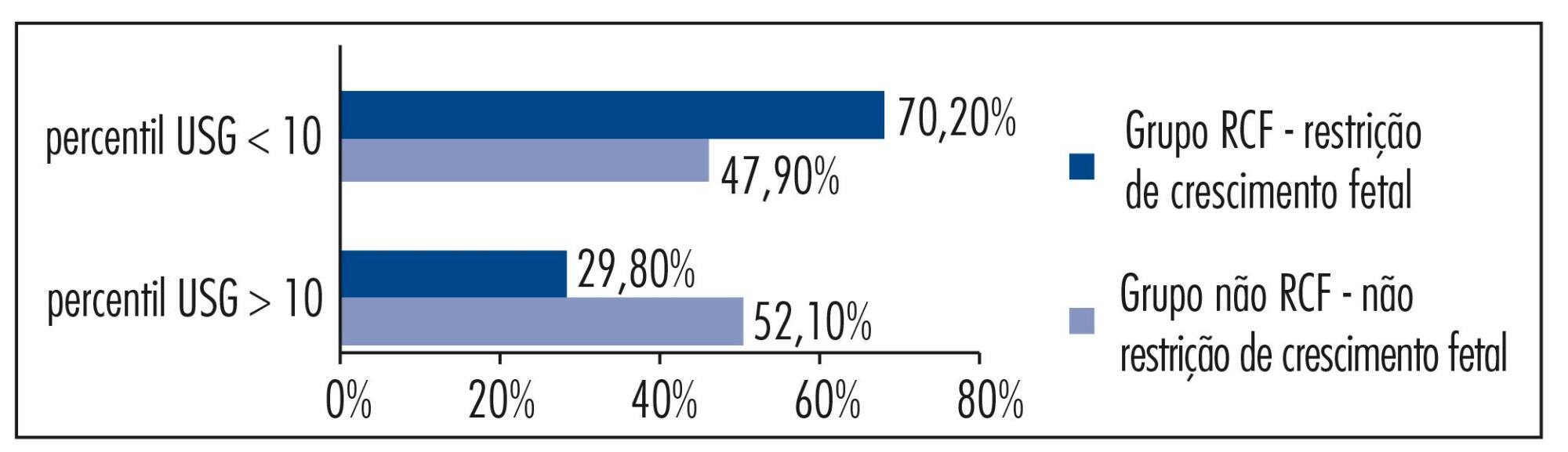
The aim of this study was to analize and describe some characteristics related to a false diagnosis of intrauterine growth restriction (IUGR).
We retrospectively included 48 pregnant women referred to our service with a suspected diagnosis of IUGR that was not confirmed after birth and we compared them to another group with confirmed IUGR. We then analyzed the characteristics of the false-positive results. The results of the study were divided into continuous and categorical variables for analysis. The χ2test or Fisher exact test was applied to compare proportions. The level of significance was set at p<0.05 for all tests.
In our sample, pregnant women with a false diagnosis of IUGR had the following characteristics: they were referred earlier (mean gestational age of 32.8 weeks); were submitted to 2 to 6 ultrasound examinations before been registered in our service; in 25% of cases ultrasound examination was performed before 12 weeks; in 66.7% of cases the symphysis-fundal height measurement was normal; in 52.1% of cases they had at least 1 sonographic exam above the 10th percentile; on average, the last ultrasound examination (performed on average at 36 weeks) was above the 18th percentile; the women were submitted to a mean number of 5 ultrasound examinations and to a mean number of 4.6 vitality exams.
The false diagnosis of IUGR involves high hospital costs and higher demand for specialists. The symphysis-fundal height measurement must be valued, and the diagnosis of IUGR must be confirmed with ultrasonography in the last weeks of pregnancy before any obstetric management is taken.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(6):274-280
DOI 10.1590/S0100-72032013000600007
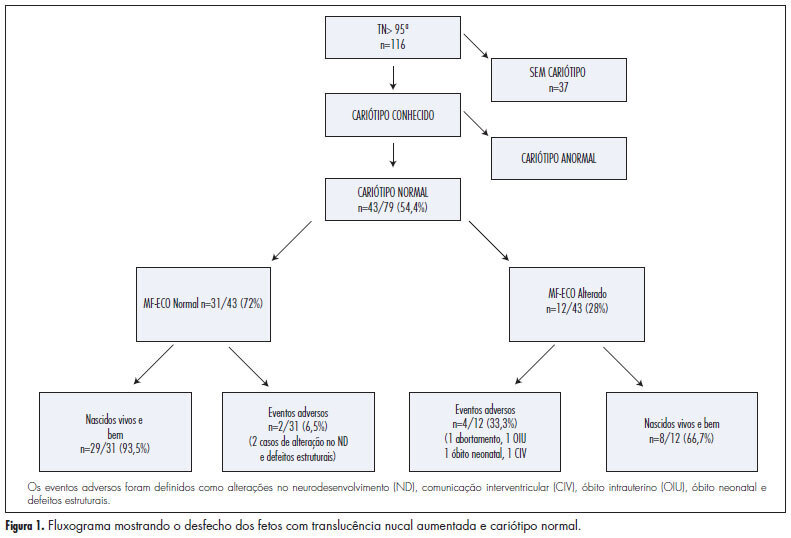
PURPOSE: To analyze the perinatal and pediatric outcome of fetuses that showed nuchal translucency (NT) above the 95th percentile (P95) and a normal karyotype in order to obtain data allowing better maternal prenatal counseling. METHODS: fetuses from a tertiary obstetric service with an NT above P95 and a normal karyotype were analyzed between 2005 and 2011. We analyzed gestational ultrasound follow-up, fetal and postnatal echocardiography (ECHO), weight, length and Apgar score at birth, and neuropsychomotor development by the Ages and Stages Questionnaire (ASQ) up to July 2012. RESULTS: During this period, there were 116 cases of nuchal translucency above the 95th percentile, and the fetal karyotype was determined in 79 of them (68%). Forty-three analyses were normal (54.4%) and 36 were altered (45.6%). Among the fetuses with a normal karyotype, one was miscarried at 15 weeks of gestation with Cantrel pentalogy and one died at 24 weeks with several structural abnormalities. There was one neonatal death of unknown cause and two cases of intraventricular communication (IVC) detected by fetal ECHO. Postnatal echocardiography revealed the persistence of IVC in one case and one case of atrial septal defect (ASD) and patent ductus arteriosus (PDA). Of the 40 surviving children, only 1 showed delayed speech development and another presented autism. The remaining cases resulted in normal neurodevelopment. CONCLUSION: During the monitoring of fetuses with increased NT and a normal karyotype, parents can be best advised that when a 2nd trimester morphological-echocardiography ultrasound study is normal, the probability of the child being born alive and well is high (93.5%).
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(2):55-59
DOI 10.1590/S0100-72032013000200003
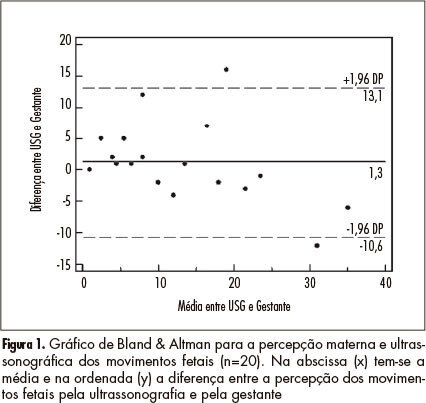
PURPOSE: To determine the agreement between maternal perception of fetal movements and the movements recorded simultaneously by ultrasound in low-risk pregnancies. METHODS: Twenty pregnant women were evaluated with the following inclusion criteria: single pregnancy, alive fetus, maternal age between 18 and 35 years; between 36 and 40 weeks gestation; normal fetal morphology at ultrasound, and absence of maternal comorbidities. The pregnant women were evaluated for 10 minutes, during which cardiotocography was used to record fetal movements triggered with the event marker, with the paper speed set at 3 cm/min. At the same time, fetal movements were observed by ultrasonography. RESULTS: The kappa index for interobserver agreement analysis was 0.62, showing good agreement (95%CI 0.45 - 0.79). The intraclass correlation coefficient was 0.82 (95%CI 0.61 - 0.92). Analysis by the Bland & Altman graph indicated good agreement. A linear regression analysis showed a significant correlation between maternal perception (x) and ultrasound (y) observation (r²=0.71, p<0.001; equation: y=5.31+0.66x). CONCLUSIONS: The agreement between ultrasound and maternal perception of fetal movement is good, allowing the use of fetal movement counting in the assessment of fetal wellbeing.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(7):310-315
DOI 10.1590/S0100-72032012000700004
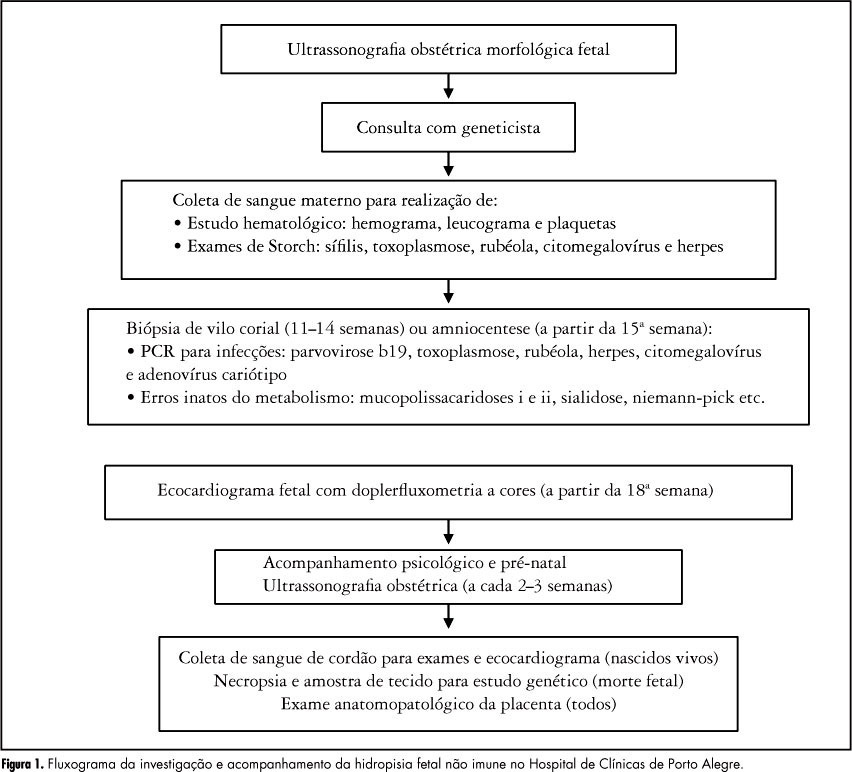
PURPOSE: To identify the etiology of nonimmune hydrops fetalis cases in pregnant women diagnosed and referred for prenatal care. METHODS: Retrospective analysis of cases with nonimmune hydrops fetalis that were monitored between March 1992 and December 2011. Diagnosis was confirmed by the presence of fetal subcutaneous edema (≥5 mm) with effusion in at least one serous cavity using obstetric ultrasound, and etiological investigation was conducted with cytogenetic (karyotype), infectious (syphilis, parvovirus B19, toxoplasmosis, rubella, cytomegalovirus, adenovirus and herpes simplex), hematologic and metabolic (inborn errors) analysis and fetal echocardiography. Twin pregnancies were excluded. Statistical analysis was performed using the χ² test for adhesion (software R 2.11.1). RESULTS: We included 116 patients with nonimmune hydrops fetalis; the etiology was elucidated in 91 cases (78.5%), while 25 cases (21.5%) were classified as idiopathic. Most cases had a chromosomal etiology, for a total of 26 cases (22.4%), followed by lymphatic etiology with 15 cases (12.9% with 11 cases of cystic hygroma), and cardiovascular and infectious etiology with 14 cases each (12.1%). In the remaining cases, the etiology was thoracic in 6.9% (eight cases), malformation syndromes in 4.3% (five cases), extrathoracic tumors in 3.4% (four cases), metabolic in 1.7% (two cases), and hematologic, gastrointestinal and genitourinary in 0.9% (one case each). During the postnatal period, 104 cases were followed up until the 40th day of life, and 12 cases had intrauterine fetal death. The survival rate of these 104 newborns was 23.1% (24 survived). CONCLUSION: An attempt should be made to clarify the etiology of hydrops diagnosed during pregnancy since the condition is associated with a wide spectrum of diseases. It is especially important to determine whether a potentially treatable condition is present and to identify disease at risk for recurrence in future pregnancies for adequate pre-conception counseling.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(4):156-162
DOI 10.1590/S0100-72032010000400002
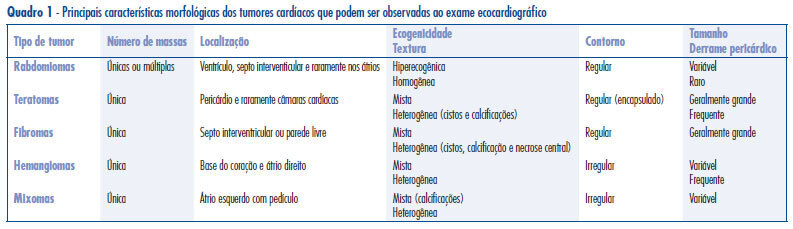
PURPOSE: to analyze the differential diagnosis, follow-up and therapeutic approach in five cases of primary cardiac tumors diagnosed during the prenatal period. METHODS: during the period from January 1997 to December 2008, 7989 pregnant women were submitted to morphological ultrasound due to the presence of risk factors for fetal malformations. Fetuses with hyperechogenic intracardiac masses larger than 1 mm diagnosed by ultrasound evaluation of the fetal heart, were selected for study. The differential diagnosis between the different tumor types was made on the basis of the ultrasound characteristics of the masses. RESULTS: five fetuses with hiperechogenic intracardiac masses were diagnosed, corresponding to a 0.06% prevalence rate. Gestational age ranged from 28 to 36 weeks (mean: 31), and maternal age ranged from 23 to 45 years (mean: 34,2). The most frequent location of the masses was the left ventricle (100%). Echographically, all masses were single or multiple, hyperechogenic, homogeneous and well delimited, compatible with a diagnosis of rhabomyoma. In cases in which the diameters of the masses were less than 20 mm, an expectant conduct was followed and no complications occurred during the prenatal period. One case with a huge tumor presented arrhythmia and cardiac insufficiency during the 35 gestational weeks, and the interruption of pregnancy was indicated. Tuberous sclerosis was associated in four cases (80%) and the diagnosis was confirmed during the postnatal follow-up. CONCLUSIONS: fetal morphological ultrasonography is the main form of early detection of primary cardiac tumors. The fetal cardiac evaluation is of fundamental importance for the differential morphological characterization of cardiac masses and for the evaluation of cardiac function. Rhabdomyomas are the most common type of fetal tumor. An expectant pre and postnatal conduct is followed, with a low risk of complications and with the possibility of spontaneous regression in most cases. Postnatal clinical follow-up is mandatory due to the high frequency of associated tuberous sclerosis.