-
Case Report06-01-2017
Prenatal Diagnosis of Galen Vein Aneurysm Using Ultrasonography and Magnetic Resonance Imaging and Perinatal and LongTerm Neurological Outcomes: A Case Series
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(6):309-314
Abstract
Case ReportPrenatal Diagnosis of Galen Vein Aneurysm Using Ultrasonography and Magnetic Resonance Imaging and Perinatal and LongTerm Neurological Outcomes: A Case Series
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(6):309-314
Views213See moreAbstract
Objective
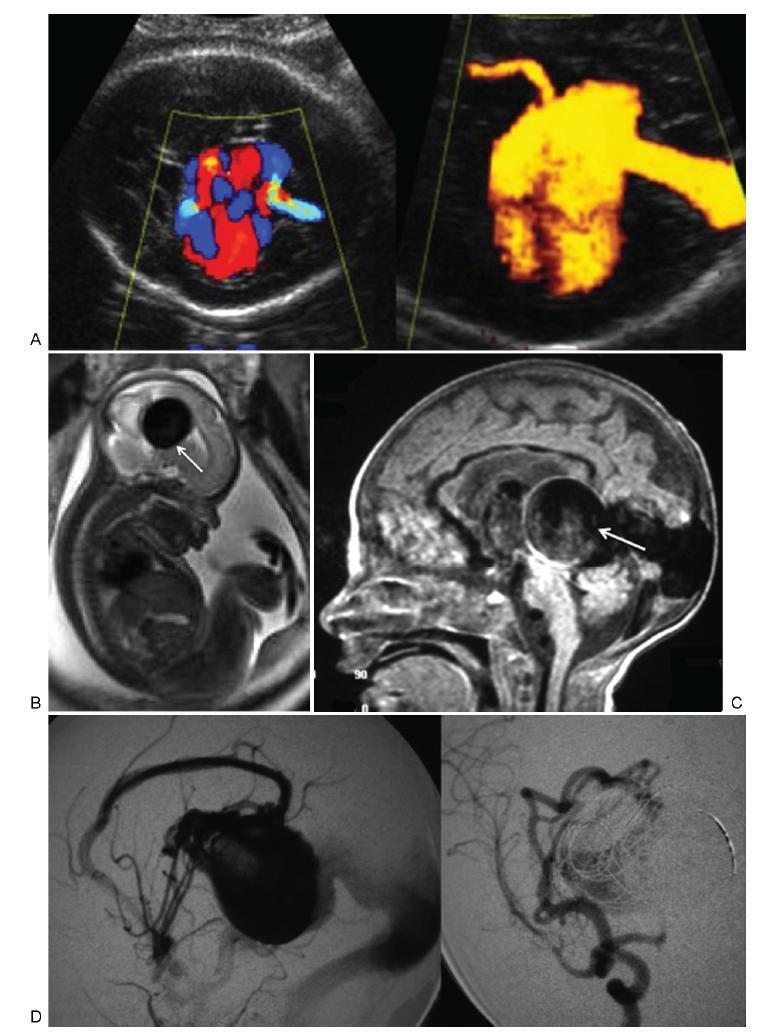
To describe the prenatal diagnosis of Galen vein aneurysm (GVA) based on ultrasonography and magnetic resonance imaging (MRI) in a series of cases, as well as its postnatal outcomes and follow-up until 4 years of age.
Methods
A retrospective longitudinal study was performed, analyzing a database comprising seven cases of prenatal diagnosis of GVA at two Brazilian institutions from February of 2000 to May of 2012. The following data were evaluated: gestational age at diagnosis, GVA dimensions on ultrasonography, associated fetal changes, findings on fetal echocardiography, gestational age at delivery, type of delivery, birth weight, Apgar score at the 1st and 5th minutes, neonatal outcomes, and survival with follow-up until 4 years of age.
Results
The mean gestational age ± standard deviation on the prenatal diagnosis of GVA based on ultrasonography was 25±4.9 weeks. The mean length of GVA was 3.2±0.4 cm. The mean gestational age at birth was 37.5±0.7 weeks, and a cesarean section was performed in 85.7% of the cases (6/7). The mean birth weight was 3,070±240.4 g. The total survival rate was 42.8% (4/7), with three neonatal deaths. Of the four survivors, three presented with normal neuropsychomotor development until 4 years of age and only one showed serious neurological sequelae. Ultrasonography and MRI showed similar findings for all seven cases.
Conclusions
Galen Vein Aneurysm is associated with a high neonatal death rate. Therefore, its prenatal diagnosis is essential for parent counseling and follow-up at tertiary care institutions.
-
Original Article04-01-2017
Ultrasonographic Evaluation of Uterine Involution in the Early Puerperium
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(4):149-154
Abstract
Original ArticleUltrasonographic Evaluation of Uterine Involution in the Early Puerperium
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(4):149-154
Views216See moreAbstract
Purpose
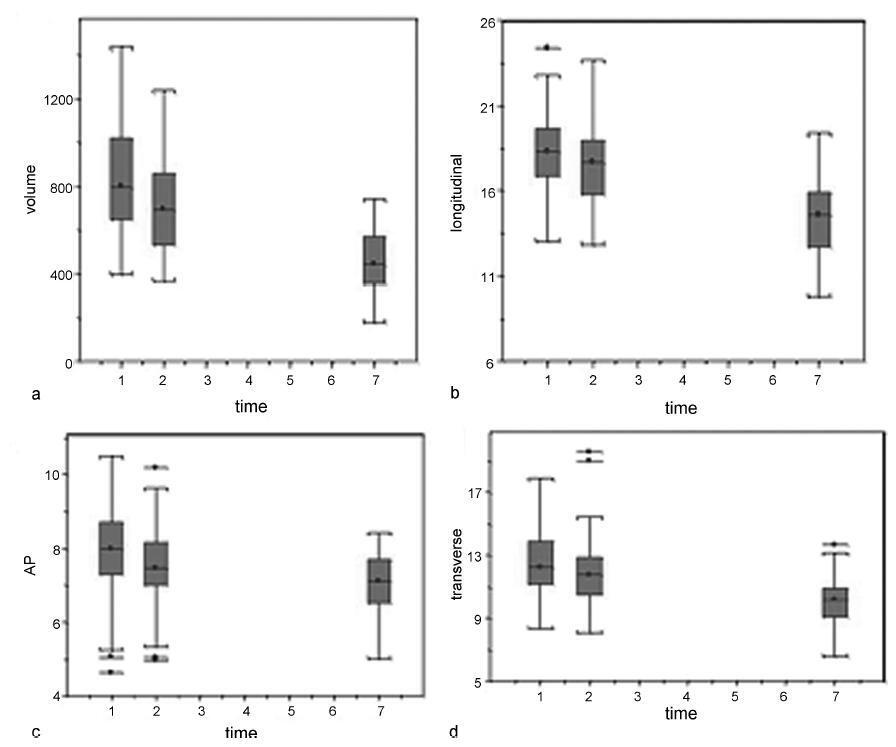
Our aim was to describe the changes observed by ultrasonography in uterine dimensions during the early puerperium among women who experienced an uncomplicated puerperium. Additionally, the influence of parity, mode of delivery, breastfeeding and birth weight on uterine involution was evaluated.
Methods
Ninety-one patients underwent an ultrasound examination on days 1 (D1), 2 (D2) and 7 (D7) of the postpartum period. The longitudinal, anteroposterior and transverse uterine diameters were measured, and the uterine volume was calculated by the formula: longitudinal diameter (LD) X anteroposterior diameter (APD) X transverse diameter (TD) X 0.45. The thickness and length of the uterine cavity were also measured.
Results
The uterine volume and the LD, APD and TD decreased by 44.8%, 20.9%, 11.8% and 20.0% respectively. The uterine cavity thickness was reduced by 23%, and the length of the cavity was reduced by 27.2% on D7. Uterine involution was correlated inversely with parity when the day of the postpartum period was not taken into account (p= 0.01). However, when the uterine involution was correlated to parity separately, with D1, D2 or D3, no correlations were found. A significant difference occurred at D2, when it was found that the uterus had a smaller volume following cesarean section compared with vaginal delivery (p= 0.04). The high birth weight and breastfeeding were significantly related to uterine involution (p ≤ 0.01 and p= 0.04).
Conclusion
The sonographic evaluation of the uterus in the early puerperium should consider birth weight, breastfeeding and parity, as well as the delivery route on D2, to identify abnormalities related to uterine involution.
-
Case Report03-01-2017
Limb Body Wall Complex Associated with Placenta Accreta: A Mere Coincidence or a Sign of an Etiopathogenic Link?
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(3):142-146
Abstract
Case ReportLimb Body Wall Complex Associated with Placenta Accreta: A Mere Coincidence or a Sign of an Etiopathogenic Link?
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(3):142-146
Views208See moreAbstract
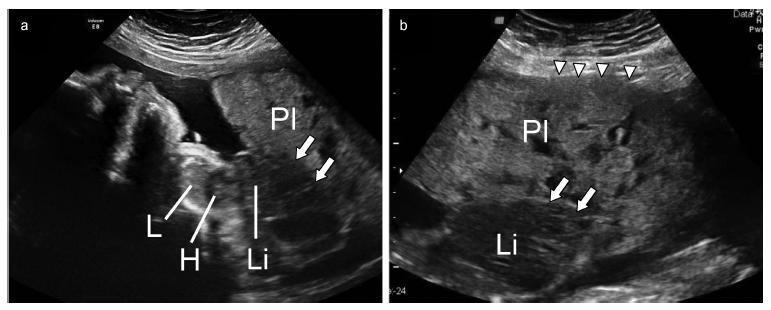
A case was reported of a fetus with the anomaly of limb body wall complex associated with placenta accreta. To date, only one account of this condition has been published in the world literature. Due to the low frequency of both complications, the hypothesis has been raised that this association may have happened not by mere coincidence, but rather by a possible common etiopathogenic mechanism. For the first time, a study proposes the existence of a possible etiopathogenic connection between the anomaly of limb body wall complex and hypoxic disorders caused by inadequate placentation in previous uterine scarring.
-
Original Article09-01-2016
Reference Ranges of Fetal Cerebral Lateral Ventricle Parameters by Ultrasonography
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):428-435
Abstract
Original ArticleReference Ranges of Fetal Cerebral Lateral Ventricle Parameters by Ultrasonography
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):428-435
Views202See moreAbstract
Objectives
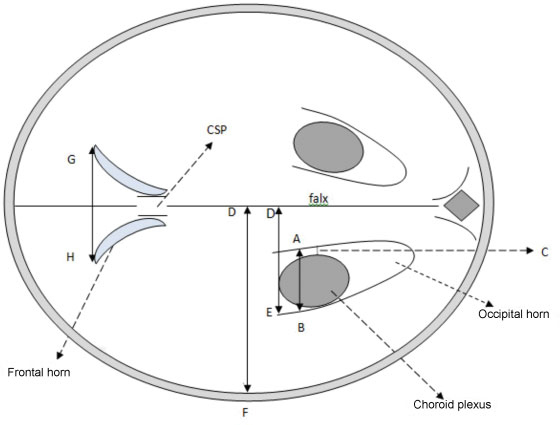
This study was done to evaluate the normal fetal cerebral lateral ventricle dimensions with transabdominal ultrasonography. The atrial width (AW), ventricle-tochoroid measurement (V-C), ventricle-to-hemisphere ratio (VHR), and combined anterior horn measurement (CAHM) were taken.
Methods
This was a cross-sectional study involving 400 normal singleton pregnant subjects whose gestational ages were between 14 and 40 weeks. Transabdominal sonography was performed to obtain the values of the fetal cerebral lateral ventricle (FCLV) parameters. Data were reported as mean standard deviation (SD) for continuous variables. The degrees of correlation between FCLV parameters and the estimated gestational age (EGA) were obtained using Pearson's correlation. Regression equations were used to generate the reference limits for the FCLV measurements.
Results
The values of AW, V-C measurements and CAHM increased with advancing gestation. The mean values of the AW, V-C and CAHM from 14 to 40 weeks increased from 6.60 0.94 mm to 9.75 0.07 mm (R2 = 0.114), 0.80 0.00 mm to 1.90 0.14 mm (R2= 0.266), and 6.95 0.06 mm to 23.07 4.02 mm (R2= 0.692) respectively, while the mean VHR decreased from 61.20 1.60% to 42.84 2.91% (R2 = 0.706) over the same period.
Conclusion
The AW, V-C, and CAHM increase, while VHR decreases with advancing gestation.
-
Original Article01-01-2016
Variability of Three-dimensional Automatic Ovarian Follicle Count in Menstrual Cycle
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(1):35-40
Abstract
Original ArticleVariability of Three-dimensional Automatic Ovarian Follicle Count in Menstrual Cycle
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(1):35-40
Views158See moreObjective
To evaluate the variability of three-dimensional automatic counts of ovarian follicles measuring 2-6 to 2-10 mm during the menstrual cycle and to determine if this test can be applied outside the early follicular phase of the menstrual cycle.
Methods
in a prospective observational study, serial transvaginal ultrasound scans were performed from April 20, 2013, to October 30, 2014, on infertile patients. Inclusion criteria: age between 18 and 35 years, BMI 18-25 kg/m2, regular menstrual cycles, no history of ovarian surgery and no hormonal changes in TSH, prolactin, fasting insulin or glucose. We excluded patients with ovarian cysts or who did not complete one or more days of the serial transvaginal ultrasound scans. The follicle count was performed in 3D mode ultrasound with a Sono AVC system. Visits were scheduled for the early follicular, mid-follicular, periovulatory and luteal phases of the menstrual cycle.
Results
Forty-five women were included. The Friedman test showed that the total number of follicles measuring 2-6 mmvaried significantly (p = 0.001) across the four periods of the menstrual cycle. The Paired Student t-test showed a significant increase in 2-6 mm follicle count from the mid-follicular and periovulatory phase to the luteal phase. We found no significant intra-cycle variation between the small follicles (2-6 mm) in the early follicular, mid-follicular and periovulatory phases. The Friedman test showed that the total number of follicles measuring 2-10 mm varied significantly (p = 0.003) across the menstrual cycle.
Conclusions
The variation of three-dimensional automatic counts of 2-6 mm follicles in the early follicular, mid-follicular and periovulatory phases was not statistically significant. The significant variability in the counts of follicles measuring 2-10 mm across the menstrual cycle does not permit this examination to be performed side the early follicular phase.
-
Original Article06-01-2015
Right subclavian artery evaluation during first trimester ultrasound scan
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(6):252-257
Abstract
Original ArticleRight subclavian artery evaluation during first trimester ultrasound scan
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(6):252-257
DOI 10.1590/SO100-720320150005278
Views148PURPOSE:
To determine the feasibility of evaluation of the right subclavian artery during
the first trimester ultrasound scan, as well as to describe the technique for its
evaluation and, in case of aberrant right subclavian artery (ARSA) identification,
to determine its association with chromosomal abnormalities and/or cardiac
malformations and its management.METHODS:
A prospective study for evaluation of the right subclavian artery during the
first trimester ultrasound scan (crown-to-rump length between 45 and 84 mm), in
all consecutive single pregnancies, by a single examiner, using a Voluson E8
system (GE Healthcare, Zipf, Austria) with a 2 to 8 MHz RAB 4-8-D transabdominal
probe, within a short period of time (less than 2 minutes), in a general low risk
population. Color and/or power Doppler flow mapping was used to classify the right
subclavian artery as normal or aberrant. Regression analysis with the IBM SPSS
Statistics software for Windows, version 20.0 was used to determine the
significance of the association between failure to examine/classify the right
subclavian artery and both fetal crown-rump length and maternal body mass index.RESULTS :
Median maternal age was 30 years (range: 17-43 years) and median gestational age
at the time of evaluation of the right subclavian artery was 12 weeks (range:
11-13 weeks). The evaluation of the right subclavian artery was successful in
138/176 (78.4%) of the cases. ARSA was diagnosed in a single case (0.7%). This
fetus with ARSA also presented a hyperechogenic focus on the left cardiac
ventricle. Fetal echocardiography at 16 weeks of gestation was performed and
confirmed ARSA and the hyperechogenic focus. Amniocentesis revealed a normal 46,
XX karyotype.CONCLUSION:
ARSA can be identified during a routine first trimester ultrasound scan. Our
single ARSA case had a normal karyotype and no associated cardiac
malformations.Key-words Aorta, thoracicPregnancy trimester, firstprenatal diagnosisSubclavian arteryUltrasonographySee more -
Original Article09-23-2014
Number of antral follicles and the success of in vitro fertilization: a multivariate analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):473-479
Abstract
Original ArticleNumber of antral follicles and the success of in vitro fertilization: a multivariate analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(10):473-479
DOI 10.1590/S0100-720320140005046
Views96See morePURPOSE:
To determine whether the antral follicle count can predict the number of retrieved oocytes in patients undergoing in vitro fertilization (IVF) and to correlate it with maternal age and pregnancy rate.
METHODS:
This was a retrospective observational study based on a review of medical records from 193 patients who underwent assisted reproduction techniques between September 2010 and September 2012 in a Clinic for Human Reproduction. The study included women indicated for IVF who had follicle-stimulating hormone levels below 10 mIU/mL on third day of the menstrual cycle, with oocyte recipients being excluded. The patients were divided into three groups according to the number of antral follicle (up to 10 follicles, 11–22 follicles, and 23 or more follicles). To compare these three groups with the group of patients who became pregnant, patients who had not developed oocytes and had not undergone embryo transfer were also excluded. Spearman's correlation coefficient was used to measure the level of association between the numerical variables, and χ2 test was used to compare pregnancy rates with antral follicle count. To assess the likelihood of pregnancy, we used multivariate logistic regression, with the level of significance set at 5%.
RESULTS:
The pregnancy rate of the sample was 35.6%. There was a positive significant correlation (sc) between antral follicle count and number of retrieved oocytes (sc=0.5; p<0.05) and a negative correlation between antral follicle count and age (sc= -0.5; p<0.05). There was no significant difference (p=0.16) when groups with different numbers of follicles were compared to the positive pregnancy test group; however, a cutoff of 27 antral follicles was observed in multivariate analysis, after which the probability of successful gestation tended to remain constant.
CONCLUSIONS:
The antral follicle count decreases over the years, is a predictor of the number of retrieved oocytes and can predict the likelihood of the success of in vitro fertilization.
-
Original Article12-09-2013
Evaluation of image parameters of pelvic adnexal masses in tele-echography
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(10):464-468
Abstract
Original ArticleEvaluation of image parameters of pelvic adnexal masses in tele-echography
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(10):464-468
DOI 10.1590/S0100-72032013001000007
Views119See morePURPOSE: To evaluate the sonographic parameters related to morphological characteristics of pelvic adnexal masses by obtaining two-dimensional images by an observer presence, forwarded electronically (via tele-ultrasound) in static and dynamic modes observers do not face (distance) for comparative analyzes inter intraobserver and to the validation of a second opinion. METHODS: From March to August 2010 were selected 50 patients with adnexal mass viewing of the pelvic ultrasound. They were subjected to ultrasound for abdominal and transvaginal routes. The images were captured in static and dynamic modes, electronically forwarded for evaluation of non-presence and two examiners evaluated according to morphological ultrasonographic parameters previously determined. RESULTS: The evaluators did not face in static and dynamic modes obtained almost perfect agreement for all morphological parameters with Kappa values between 0.6 and 0.8. There was no difference between the methods employed, except for the morphological parameter papillary projection in the static mode , in which the agreement was almost perfect ( 0.8 ) while in dynamic mode was substantial (0.6). CONCLUSIONS: The sonographic parameters of the features of adnexal masses pelvic sent by tele-ultrasound are capable of being validated for issuing a second opinion. There were no significant differences in the methodology used in the issue of tele-ultrasound images (static or dynamic) to characterize the composition of pelvic adnexal masses.


