Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(6):338-346
To discuss the implementation and contributions of the External Quality Monitoring in the city of Rio de Janeiro and to analyze the performance of the main providers of cervical cytopathology in this city from September 2013 to March 2017, here referred to as “Alpha laboratory” and “Beta laboratory.”
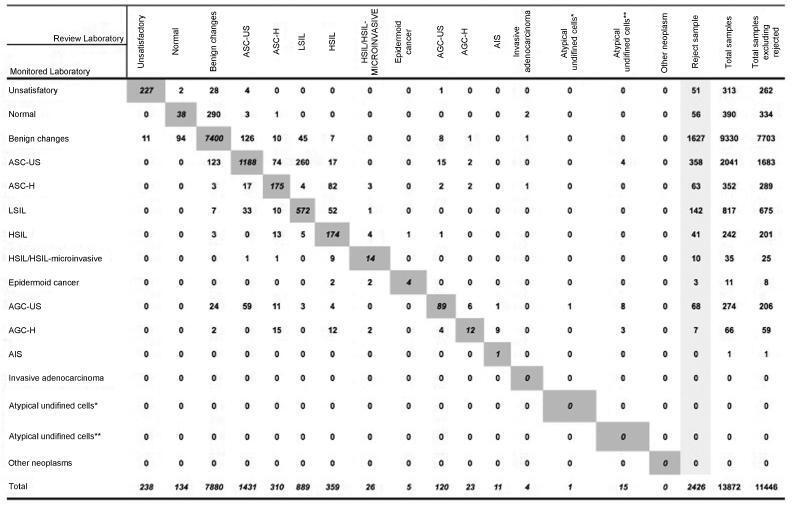
Observational, cross-sectional, retrospective study using information from the Cervical Cancer Control Information System (SISCOLO, in the Portuguese acronym), municipal coordinationmodule, External QualityMonitoring report. The proportions of false positives, false negatives, unsatisfactory samples and rejected samples were estimated. The agreement among the observers was analyzed through the Kappa index and the reduction of disagreements in the period for each laboratory studied, comparing the results of each cycle.
A total of 19,158 examinations were selected, of which 19,130 (99.85%) were monitored, 16.649 (87, 03%) were reviewed by the External Quality Monitoring Unit, 2,481 (12,97%) were rejected and 441 (2,65%) were considered unsatisfactory. The “Beta laboratory” presented excellent concordance in all cycles; the “Alpha laboratory” had good concordance in the first two cycles (K = 0.76 and 0.79), becoming excellent in the following four cycles. The average Kappa index was 0.85, with median of 0.86. The percentage of diagnostic disagreement was 6.63% of the reviewed exams, of which 5.38% required a change of conduct
External Quality Monitoring is an exercise in diagnostic improvement, and its implementation was fundamental to ensure the reliability of the cytopathological exams in the city of Rio de Janeiro.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(2):65-70
The objective of this study is to assess the performance of cytopathology laboratories providing services to the Brazilian Unified Health System (Sistema Único de Saúde - SUS) in the State of Minas Gerais, Brazil.
This descriptive study uses data obtained from the Cervical Cancer Information System from January to December 2012. Three quality indicators were analyzed to assess the quality of cervical cytopathology tests: positivity index, percentage of atypical squamous cells (ASCs) in abnormal tests, and percentage of tests compatiblewith high-grade squamous intraepithelial lesions (HSILs). Laboratories were classified according to their production scale in tests per year≤5,000; from 5,001 to 10,000; from 10,001 to 15,000; and 15,001. Based on the collection of variables and the classification of laboratories according to production scale, we created and analyzed a database using Microsoft Office Excel 97-2003.
In the Brazilian state of Minas Gerais, 146 laboratories provided services to the SUS in 2012 by performing a total of 1,277,018 cervical cytopathology tests. Half of these laboratories had production scales≤5,000 tests/year and accounted for 13.1% of all tests performed in the entire state; in turn, 13.7% of these laboratories presented production scales of > 15,001 tests/year and accounted for 49.2% of the total of tests performed in the entire state. The positivity indexes of most laboratories providing services to the SUS in 2012, regardless of production scale, were below or well below recommended limits. Of the 20 laboratories that performed more than 15,001 tests per year, only three presented percentages of tests compatible with HSILs above the lower limit recommended by the Brazilian Ministry of Health.
The majority of laboratories providing services to the SUS in Minas Gerais presented quality indicators outside the range recommended by the Brazilian Ministry of Health.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(9):398-403
DOI 10.1590/SO100-720320140004996
To evaluate the impact of continued education provided by an external quality control laboratory on the indicators of internal quality control of cytopathology exams.
The internal quality assurance indicators for cytopathology exams from 12 laboratories monitored by the External Quality Control Laboratory were evaluated. Overall, 185,194 exams were included, 98,133 of which referred to the period preceding implementation of a continued education program, while 87,061 referred to the period following this intervention. Data were obtained from the Cervical Cancer Database of the Brazilian National Health Service.
Following implementation of the continued education program, the positivity index (PI) remained within recommended limits in four laboratories. In another four laboratories, the PI progressed from below the limits to within the recommended standards. In one laboratory, the PI remained low, in two laboratories, it remained very low, and in one, it increased from very low to low. The percentage of exams compatible with a high-grade squamous intraepithelial lesion (HSIL) remained within the recommended limits in five laboratories, while in three laboratories it progressed from below the recommended levels to >0.4% of the total number of satisfactory exams, and in four laboratories it remained below the standard limit. Both the percentage of atypical squamous cells of undetermined significance (ASC-US) in relation to abnormal exams, and the ratio between ASC-US and intraepithelial lesions remained within recommended levels in all the laboratories investigated.
An improvement was found in the indicators represented by the positivity index and the percentage of exams compatible with a high-grade squamous intraepithelial lesion, showing that the role played by the external quality control laboratory in providing continued education contributed towards improving laboratory staff skills in detecting cervical cancer precursor lesions.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(5):192-197
DOI 10.1590/S0100-7203201400050002
To analyze the prevalence of cervical cytopathological results for the screening of cervical cancer with regard to women's age and time since the last examination in Maceió and Rio de Janeiro, Brazil, among those assisted by the Brazilian Unified Health System.
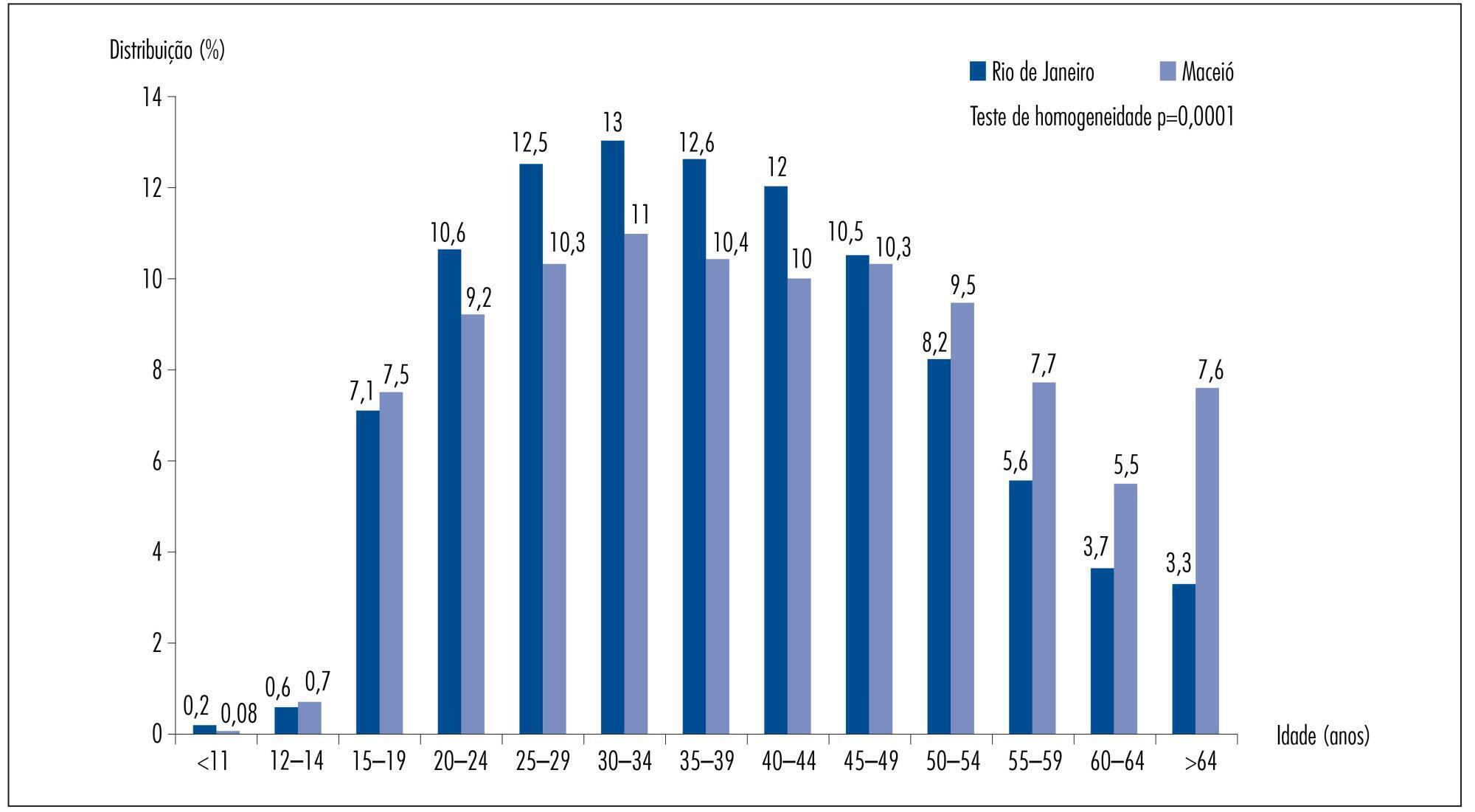
Cervical cytopathological results available in the Information System of Cervical Cancer Screening for the year 2011 were analyzed, corresponding to 206,550 for Rio de Janeiro and 45,243 for Maceió.
In Rio de Janeiro, examination at one and two year intervals predominated, while in Maceió examination at one and three year intervals had a higher predominance. Women who underwent cervical smear screening in Maceió were older than those in Rio de Janeiro. The prevalence of invasive squamous cell carcinoma was similar for the two cities, but all the other results presented a higher prevalence in Rio de Janeiro: ASCUS (PR=5.32; 95%CI 4.66-6.07); ASCH (PR=4.27; 95%CI 3.15-5.78); atypical glandular cells (PR=10.02; 95%CI 5.66-17.76); low-grade squamous intraepithelial lesions (PR=6.10; 95%CI 5.27-7.07); high-grade squamous intraepithelial lesions (PR=8.90; 95%CI 6.50-12.18) and adenocarcinoma (PR=3.00; 95%CI 1.21-7.44). The rate of unsatisfactory cervical samples was two times higher in Maceió and that of rejected samples for analysis was five times higher in Maceió when compared to Rio de Janeiro.
The prevalence rates of altered cervical cytopathological results was significantly higher in Rio de Janeiro than in Maceió. There is no objective information that may justify this difference. One hypothesis is that there may be a difference in the diagnostic performance of the cervical cancer screening, which could be related to the quality of the Pap smear. Thus, these findings suggest that it would be necessary to perform this evaluation at national level, with emphasis on the performance of cervical cancer screening in order to improve the effectiveness of cervical cancer control.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(8):351-356
DOI 10.1590/S0100-72032012000800002
PURPOSE: To evaluate the diagnostic agreement between the cytopathology reports issued by accredited laboratories and those obtained by quality control. METHODS: We calculated the overall agreement and Cohen's kappa coefficients of a convenience sample of smears selected monthly by the Information System of Cervical Cancer (SISCOLO) for External Quality Control of the 15 laboratories that performed cytopathological PAP tests for the Brazilian Public Health System (SUS) between 2002 and 2011 in Mato Grosso do Sul, a State of the Midwest Region of the country. A comparison of the reliability values (coefficient of concordance and Kappa coefficient) between the initial and final years was computed by the absolute change (delta) and relative percent difference (RPD). RESULTS: There were 15.989 smears sent for rereading, 48.1% of which had a report of normal/benign changes, followed by atypical/low-grade squamous intraepithelial lesions (36.3%), high grade squamous intraepithelial lesion/carcinoma/adenocarcinoma (4.2%), and unsatisfactory (11.4%). The overall correlation coefficient ranged between 0.2 and 1.0, and the median value increased from 0.7 in 2002 to 1 in 2011 (RPD=+36.6%). During the same period, the median values of the Kappa coefficient increased from 0.5 to 0.9 (RPD=+80.8%). CONCLUSIONS: These results emphasize the feasibility of the External Quality Control of cytopathology at the state level and its implementation results in improvement in the diagnoses performed in the SUS network.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(3):144-149
DOI 10.1590/S0100-72032011000300008
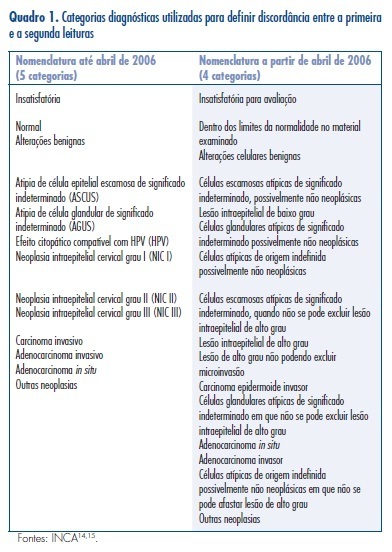
PURPOSE: to identify the nomenclature for reporting cervical cytological diagnoses used by laboratories which render services to the Brazilian Unified Health System (SUS) and which participate in External Quality Monitoring (MEQ). To evaluate the information acquired from gynecologists of the SUS regarding the various diagnostic classifications that they receive in the cervical cytology diagnostic reports. METHODS: we evaluated 94 cytology reports issued by laboratories which participate in the MEQ in the State of São Paulo, Brazil, and 126 questionnaires applied to gynecologists who work for the SUS. RESULTS: out of the 94 laboratories, 81 (86.2%) use one diagnostic classification: 79 (97.6%) use the Brazilian Nomenclature for Cytological Reports (NBLC), 1 (1.2%) uses the Papanicolaou classification and 1 (1.2%) uses the Richart diagnostic classification. Of the 13 (13.8%) laboratories that use more than one classification, 5 use 2 types and 8 use 3 to 4 types, with 9 including the Papanicolau diagnostic classification. The study showed that 52 (55.3%) laboratories presented more than one descriptive diagnosis in the same report. Out of the 126 gynecologists who filled out a questionnaire evaluating the cytopathology reports, 78 (61.9 %) stated that they received laboratory reports with only one diagnostic classification, 48 (38.1%) received reports with more than one classification and 2 received reports with all 4 classifications. Among the 93 (73.8%) gynecologists who prefer only one classification, 56 (60.2%) claimed that the NBLC contributes to clinical practice, 13 (14.0%) opted for the Richart classification, 8 (8.6%) for the Reagan classification and 16 (17.2%) for the Papanicolaou classification. Out of 33 (26.2%) gynecologists who prefer more than one classification, 5 opted for the 4 classifications. CONCLUSIONS: these data suggest that there is still resistance on the part of pathologists about using the official nomenclature in cytology reports for SUS. There is discrepancy between the information that gynecologists would like to see in the reports and the information provided by the pathologists. Greater efforts should be made to stimulate the use of the official nomenclature.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(10):508-512
DOI 10.1590/S0100-72032009001000007
PURPOSE: to check epidemiological data from a breast diagnostic clinic. METHODS: mammographies from 35,041 patients were studied, within a period of 2 years and 7 months, from 2004 to 2006, 32,049 (91.5%) of them from screening, and 2,992 from symptomatic patients (8.5%). The calculated parameters were: detection rate of the screening patients, percentage of cancer among the symptomatic patients, rate of biopsy indication, percentage of minimal, in situ, and stage 0-1 carcinomas, recall rate, and predictive value of mammographies considered as abnormal and of biopsies' indications in screening patients. RESULTS: 228 diagnoses of breast cancer were made, 111 in screening patients (0.34% detection rate) and 117 in symptomatic patients (3.91% detection rate). The number of biopsies' recommendations among screening patients was 544 (1.7% of those patients). There were 28% of minimal carcinomas, 10% of in situ carcinomas and 93% of stage 0-1 carcinomas among the screening patients. Recall rate was 19%. Positivity of mammographies considered as abnormal (VPP1) was 1.65%. The rate of biopsies' positivity (VPP2) was 21.9%. CONCLUSIONS: this study brings important epidemiological data for the audit of mammographic screening, rare among us. Data have been analyzed as compared to what is recommended by the literature, the detection rate and the percentage of minimal and in situ carcinomas found being comparable to the established values, but with the VPP value lower than the ideal.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(7):360-365
DOI 10.1590/S0100-72032008000700007
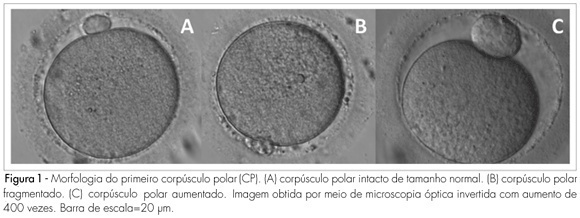
PURPOSE: to determine the relationship between the morphology of the first spindle pole of human oocytes and rates of fertilization, fragmentation and embryo quality in procedures of Intracytoplasmic Sperm Injection (ICSI). METHODS: retrospective study of 582 consecutive ICSI cycles, from July 2003 to July 2005. The morphology of the first spindle pole (SP) was assessed through the analysis of 3,177 oocytes in metaphase II, immediately before the ICSI procedure, always by the same observer. SP has been classified in the following categories: normal size intact, fragmented or augmented SP. Fertilization rate and fragmentation, and the number and rate of good quality embryos in each one of the three groups studied have been evaluated, 48 hours after ICSI (D2). Embryos with four cells, without fragmentation and with symmetric blastomeres in D2 were considered as of good quality. RESULTS: rates of fertilization, fragmentation and of good quality embryo formation, resulting from oocyte insemination, with augmented SP (20.7, 16.7 and 5% respectively) were significantly lower than the ones from intact and normal size SP (70.8, 62.5 and 19%, respectively) or from fragmented SP oocytes (69.7, 60.5 and 17.1%, respectively). CONCLUSIONS: it has been observed that the presence of augmented first spindle pole is related to worse rates of fertilization, fragmentation and bad quality embryo formation. Nevertheless, fragmentation in the first spindle pole of the oocyte does not seem to affect ICSI results.