Summary
Revista Brasileira de Ginecologia e Obstetrícia. 09-06-2024;46:e-rbgo39i
This study aims to create a new screening for preterm birth < 34 weeks after gestation with a cervical length (CL) ≤ 30 mm, based on clinical, demographic, and sonographic characteristics.
This is a post hoc analysis of a randomized clinical trial (RCT), which included pregnancies, in middle-gestation, screened with transvaginal ultrasound. After observing inclusion criteria, the patient was invited to compare pessary plus progesterone (PP) versus progesterone only (P) (1:1). The objective was to determine which variables were associated with severe preterm birth using logistic regression (LR). The area under the curve (AUC), sensitivity, specificity, and positive predictive value (PPV) and negative predictive value (NPV) were calculated for both groups after applying LR, with a false positive rate (FPR) set at 10%.
The RCT included 936 patients, 475 in PP and 461 in P. The LR selected: ethnics white, absence of previous curettage, previous preterm birth, singleton gestation, precocious identification of short cervix, CL < 14.7 mm, CL in curve > 21.0 mm. The AUC (CI95%), sensitivity, specificity, PPV, and PNV, with 10% of FPR, were respectively 0.978 (0.961-0.995), 83.4%, 98.1%, 83.4% and 98.1% for PP < 34 weeks; and 0.765 (0.665-0.864), 38.7%, 92.1%, 26.1% and 95.4%, for P < 28 weeks.
Logistic regression can be effective to screen preterm birth < 34 weeks in patients in the PP Group and all pregnancies with CL ≤ 30 mm.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 07-26-2024;46:e-rbgo58
To assess a panel of cytokines and placental insufficiency with the risk of preterm delivery (PTD).
Nested case-control study into the BRISA birth cohort. Eighty-two mother-infant-placenta pairs were selected at 20+0 to 25+6 weeks. Circulating biomarker levels were performed using Luminex flowmetric xMAP technology. Cytokines classified as Th1, Th2 or Th17 and other biomarkers were selected. The ratio between birth weight and placental weight (BW/PW) was used as a proxy for placental efficiency. Spearman correlation, univariate analyses and logistic regression models were calculated. Sensitivity, specificity, positive and negative likelihood ratios were calculated using the Receiver Operating Characteristic curve.
Mean gestational age was 250 days, 14,6% were small for gestational age, 4,8% large for gestational age and 13,4% stunted. Placental efficiency was higher for term newborns (p<0,001), and 18/22 (81%) preterm biomarker values were higher than the control group. Th1 cytokines were highly correlated, while the weakest correlation was observed in other biomarkers. Less education was associated with a higher risk of PTD (p = 0.046), while there was no appreciable difference in the risk of PTD for placental insufficiency. Biomarkers showed negligible adjusted OR of PTD (0.90 to 1.02). IL-6, IL-8, IL-1β, TNFβ, IL-4, IL-13, GCSF, MIP1A, VEGF, EGF, and FGF2 presented a higher sensitivity ranging from 75.56% to 91.11%.
IL-8, IL-12p40, IL-4, IL-13, GCSF, MIP1B, and GMSF in asymptomatic pregnant women were associated with PTD. This finding suggests an activation of maternal inflammatory response.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 04-09-2024;46:e-rbgo32
To ascertain how screening for preterm birth is performed among obstetricians working in public and private practice in a middle-income country.
Cross-sectional study of 265 obstetrician-gynecologists employed at public and private facilities. An online questionnaire was administered, with items designed to collect data on prematurity screening and prevention practices.
The mean age of respondents was 44.5 years; 78.5% were female, and 97.7% had completed a medical residency program. Universal screening (i.e., by ultrasound measurement of cervical length) was carried out by only 11.3% of respondents in public practice; 43% request transvaginal ultrasound if the manual exam is abnormal, and 74.6% request it in pregnant women with risk factors for preterm birth. Conversely, 60.7% of respondents in private practice performed universal screening. This difference in screening practices between public and private practice was highly significant (p < 0.001). Nearly all respondents (90.6%) reported prescribing vaginal progesterone for short cervix.
In the setting of this study, universal ultrasound screening to prevent preterm birth was used by just over half of doctors in private practice. In public facilities, screening was even less common. Use of vaginal progesterone in cervical shortening was highly prevalent. There is an unmet need for formal protocols for screening and prevention of preterm birth in middle-income settings.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 01-12-2022;43(11):811-819
To investigate the characteristics of women who had preterm birth (PTB) and related outcomes according to ethnicity.
A secondary analysis of a multicenter cross-sectional study conducted in Brazil. Women who had PTB were classified by self-report as white and non-white. Clinical, pregnancy, and maternal data were collected through postpartum interviews and reviews of medical charts. The sociodemographic, obstetric and clinical characteristics of the women, as well as the mode of delivery and the neonatal outcomes among different ethnic groups were compared through a bivariate analysis.
Of the 4,150 women who had PTB, 2,317 (55.8%) were non-white, who were more likely: to be younger than 19 years of age (prevalence ratio [PR]: 1.05; 95% confidence interval [95%CI]: 1.01-1.09); to be without a partner; to live on low income; to have lower levels of schooling; to have ≥ 2 children; to perform strenuous work; to be fromthe Northeastern region of Brazil rather than the from Southern region; to have a history of ≥ 3 deliveries; to have an interpregnancy interval<12 months; to have pregnancy complications such as abortion, PTB, preterm premature rupture of membranes (pPROM), and low birth weight; to initiate antenatal care (ANC) visits in the second or third trimesters; to have have an inadequate number of ANC visits; to be under continuous overexertion; to smoke in the first and second or third trimesters; and to have anemia and gestational hypertension. The maternal and neonatal outcomes did not differ between the groups, except for the higher rate of low birth weight (73.7% versus 69.0%) in infants born to non-white women, and the higher rate of seizures (4.05% versus 6.29%) in infants born to white women.
Unfavorable conditions weremore common in non-whites than inwhites. Proper policies are required to decrease inequalities, especially in the context of prematurity, when women and their neonates have specific needs.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 06-18-2021;43(4):264-274
To evaluate the applicability and usefulness of second-trimester TUCL to predict PTB in a cohort of Portuguese pregnant women.
Retrospective cross-sectional cohort study including all singleton pregnant women who performed their second-trimester ultrasound (between weeks 18 and 22þ6 days) from January 2013 to October 2017 at Centro Hospitalar Universitário São João.
Our cohort included 4,481 women. The prevalence of spontaneous PTB was of 4.0%, with 0.7% occurring before the 34th week of gestation. The mean TUCL was of 33.8mm,and percentiles 3, 5 and 10 corresponded toTUCLs of 25.0mm, 27.0mmand 29.0mmrespectively. The multiple logistic regression analysis, including maternal age, previous PTB and cervical surgery showed a significant negative association between TUCL and PTB, with an odds ratio (OR) of 0.92 (95% confidence interval [95%CI]: 0.90-0.95; p<0.001). The use of a TUCL of 20mm is the best cut-off, when compared with the 25-mm cut-off, improving the prediction of risk.
The present study showed an inverse association between TUCL and PTB, and that the inclusion of other risk factors like maternal age, previous PTB and cervical surgery can improve the screening algorithm. Furthermore, it emphasizes that the TUCL cut-off that defines short cervix can differ according to the population.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 12-21-2020;42(10):621-629
The present study aims to determine if the use of cervical pessary plus progesterone in short-cervix (≤ 25 mm) dichorionic-diamniotic (DC-DA) twin pregnancies is equivalent to the rate of preterm births (PBs) with no intervention in unselected DC-DA twin pregnancies.
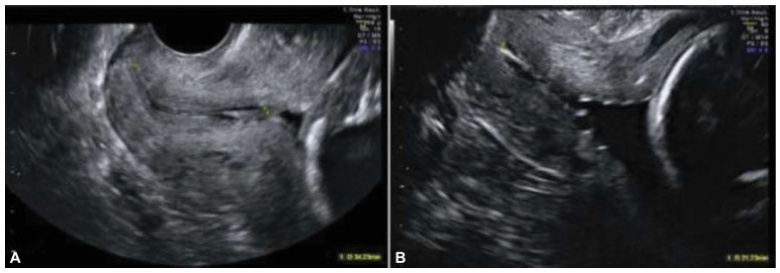
A historical cohort study was performed between 2010 and 2018, including a total of 57 pregnant women with DC-DA twin pregnancies. The women admitted from 2010 to 2012 (n = 32) received no treatment, and were not selected by cervical length (Non-Treated group, NTG), whereas those admitted from 2013 to 2018 (n = 25), were routinely submitted to cervical pessary plus progesterone after the diagnosis of short cervix from the 18th to the 27th weeks of gestation (Pessary-Progesterone group, PPG). The primary outcome analyzed was the rate of PBs before 34 weeks.
There were no statistical differences between the NTG and the PPG regarding PB < 34 weeks (18.8%; versus 40.0%; respectively; p = 0.07) and the mean birthweight of the smallest twin (2,037 ± 425 g versus 2,195 ± 665 g; p = 0.327). The Kaplan-Meyer Survival analysis was performed, and there were no differences between the groups before 31.5 weeks. Logistic regression showed that a previous PB (< 37 weeks) presented an odds ratio (OR) of 15.951 (95%; confidence interval [95%;CI]: 1.294-196.557; p = 0.031*) for PB < 34 weeks in the PPG.
In DC-DA twin pregnancies with a short cervix, (which means a higher risk of PB), the treatment with cervical pessary plus progesterone could be considered equivalent in several aspects related to PB in the NTG, despite the big difference between these groups.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 03-27-2020;42(1):61-64
Premature delivery often complicates multifetal pregnancies, placing neonates at risk of seriousmorbidity andmortality. In select cases, pretermbirth of one sibling may not require delivery of the remaining fetus(es), which may remain in utero for a delayedinterval delivery, consequently improving neonatalmorbidity andmortality. Currently, there is no consensus on the best protocol for the optimalmanagement of these cases. We report one case of delayed-interval delivery of a dichorionic pregnancy assisted in our center. In this case, prophylactic cerclage, tocolytic therapy and administration of broad-spectrum prophylactic antibiotics enabled delivery at 37 weeks, corresponding to 154 days of latency, which is, to our knowledge, the longest interval described in the literature. The attempt to defer the delivery of the second fetus in peri-viability is an option that should be offered to parents after counseling, providing that the clinical criteria of eligibility are fulfilled. The correct selection of candidates, combined with the correct performance of procedures, as well as fetal and maternal monitoring and early identification of complications increase the probability of success of this type of delivery.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 04-15-2019;41(1):53-58
The gestational complication most associated with perinatalmortality and morbidity is spontaneous preterm birth with gestational age < 37 weeks. Therefore, it is necessary to identify its risk factors and attempt its prevention. The benefits of the pessary in prematurity are under investigation. Our objective was to analyze the use of the pessary in the prevention of preterm births in published studies, and to compare its efficacy with other methods.
Randomized clinical trials published between 2010 and 2018 were selected from electronic databases. Studies on multiple gestations were excluded.
Two studies were in favor of the pessary as a preventive method, one study was contrary to the method and another two showed no statistically significant difference. Themeta-analysis showed no statistical difference with the use of a cervical pessary in the reduction of births < 37 (odds ratio [OR]: 0.63; confidence interval [95% CI]: 0.38-1.06) and < 34 weeks (OR: 0.74; 95% CI: 0.35-1.57)
The pooled data available to date seems to show a lack of efficacy of the cervical pessary in the prevention of preterm birth, although the heterogeneity of the studies made comparisons more difficult.