-
Original Article
Effect of COVID-19 on Brazilian cesarean and prematurity rates: a cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo6
03-18-2025
Summary
Original ArticleEffect of COVID-19 on Brazilian cesarean and prematurity rates: a cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo6
03-18-2025Views77See moreAbstract
Objective:
To investigate the relationship between prematurity and cesarean section rate in Brazil during the beginning of COVID-19 pandemic.
Methods:
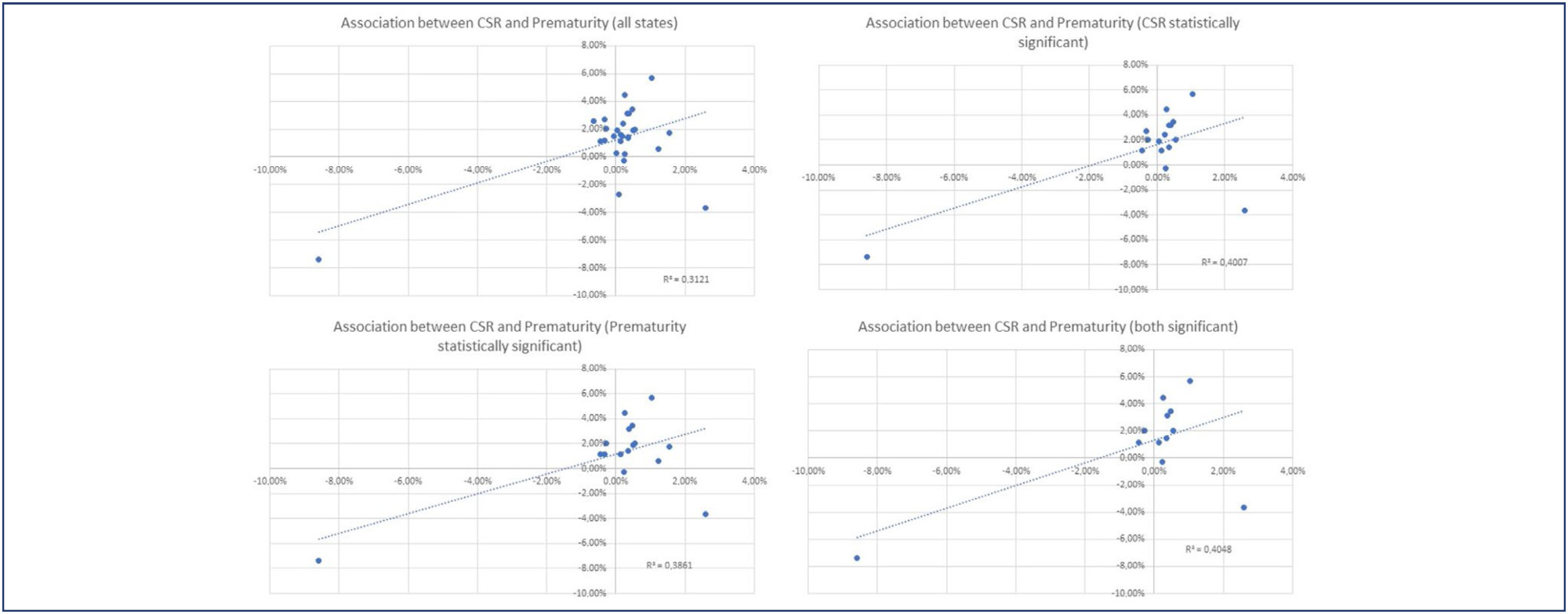
Utilizing the Robson Classification, this study analyzed data from the Brazilian Ministry of Health's Live Births Panel, comparing CSR) and group 10 (preterm deliveries) between 2019 (pre-pandemic) and 2021 (pandemic) in each of Brazilian states and the overall country. The prematurity and CSR were compared using prevalence ratio and confidence interval, and p-value was obtained. The variation of prematurity and CSR were compared through the coefficient of determination (R2).
Results:
A total of 5,522,910 deliveries were evaluated during the period. The CSR increased from 56.34% to 57.05% (p<0.01), and the frequency of preterm deliveries rose from 8.99% to 9.13% (p<0.01). The CSR increased in 23 States and decreased in 4 States, while the prematurity rate increased in 16 States and decreased in 10 States. A positive relationship between the increase of CSR and prematurity was observed during COVID-19, with an R2 value of 0.3121, suggesting a moderate association between these two variables.
Conclusion:
Between 2019 (pre-COVID-19 pandemic) and 2021 (the first full year of the COVID-19 pandemic), there was an increase in prematurity and CSR in Brazil. These increases were observed in most Brazilian states and may be correlated. However, it is impossible to establish a cause-effect relationship given the design of this study.
-
Original Article
Amniotic Sludge and Prematurity: Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(8):489-498
10-09-2023
Summary
Original ArticleAmniotic Sludge and Prematurity: Systematic Review and Meta-analysis
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(8):489-498
10-09-2023Views199See moreAbstract
Objective
To perform a systematic review and meta-analysis of studies on maternal, fetal, and neonatal outcomes of women with singleton pregnancies, after spontaneous conception, and with the diagnosis of amniotic sludge before 37 weeks of gestational age.
Data Sources
We conducted a search on the PubMed, Cochrane, Bireme, and Theses databases until June 2022.
Selection of Studies
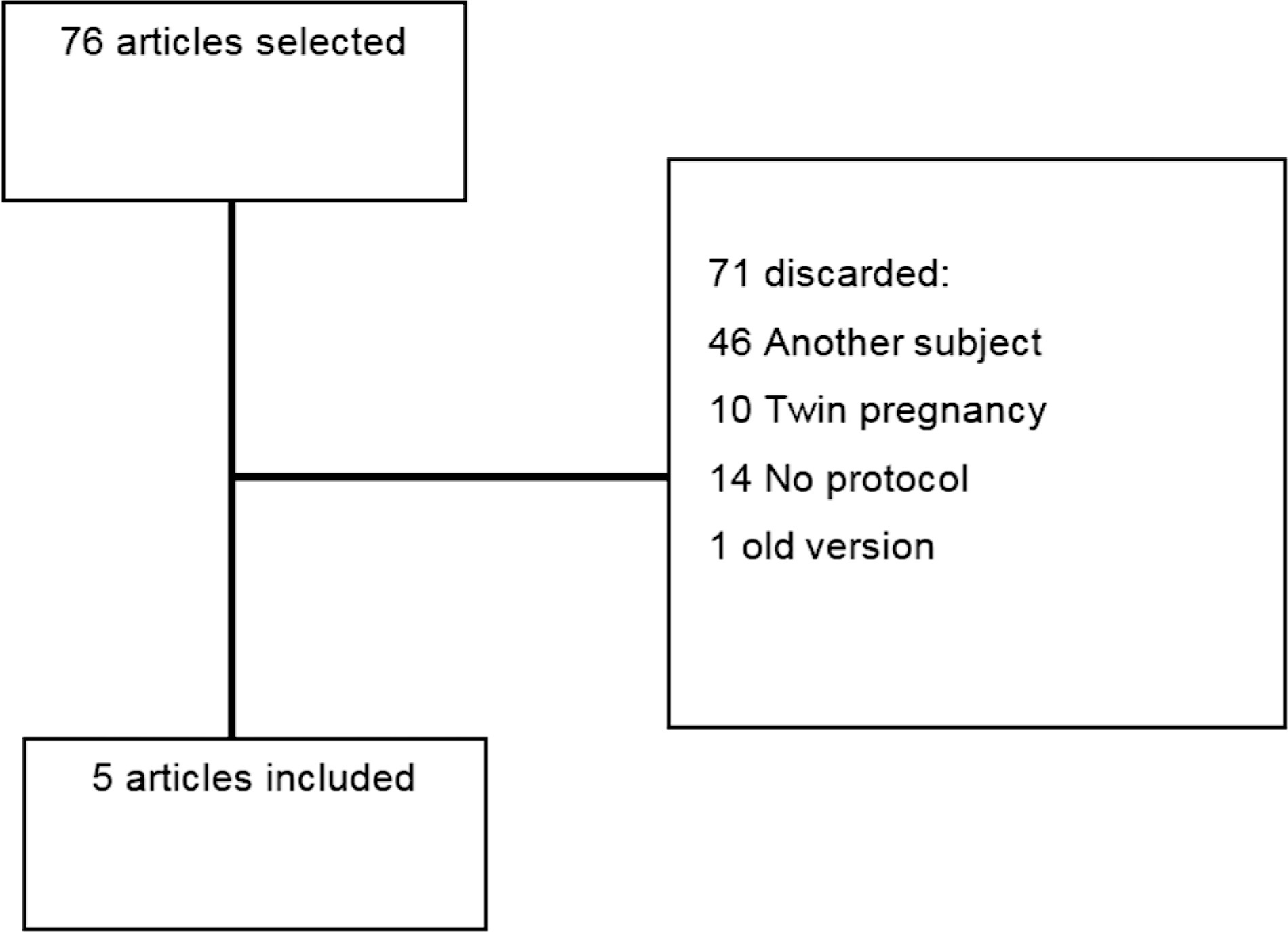
Using the keywords intra-amniotic sludge or fluid sludge or echogenic particles, we found 263 articles, 132 of which were duplicates, and 70 were discarded because they did not meet the inclusion criteria.
Data Collection
The articles retrieved were analyzed by 2 reviewers; 61 were selected for full-text analysis, 18 were included for a qualitative analysis, and 14, for a quantitative analysis.
Data Synthesis
Among the maternal outcomes analyzed, there was an increased risk of preterm labor (95% confidence interval [95%CI]: 1.45–2.03), premature rupture of ovular membranes (95%CI: 1.99–3.79), and clinical (95%CI: 1.41–6.19) and histological chorioamnionitis (95%CI: 1.75–3.12). Regarding the fetal outcomes, there was a significant increase in the risk of morbidity (95%CI: 1.80–3.17), mortality (95%CI: 1.14–18.57), admission to the Neonatal Intensive Care Unit (NICU; 95%CI: 1.17–1.95), and neonatal sepsis (95%CI: 2.29–7.55).
Conclusion
The results of the present study indicate that the presence of amniotic sludge is a risk marker for preterm delivery. Despite the heterogeneity of the studies analyzed, even in patients with other risk factors for prematurity, such as short cervix and previous preterm delivery, the presence of amniotic sludge increases the risk of premature labor. Moreover, antibiotic therapy seems to be a treatment for amniotic sludge, and it may prolong pregnancy.
-
Review Article
Comparison between Protocols for Management of Fetal Growth Restriction
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(2):096-103
07-10-2023
Summary
Review ArticleComparison between Protocols for Management of Fetal Growth Restriction
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(2):096-103
07-10-2023Views175See moreAbstract
This comprehensive review compares clinical protocols of important entities regarding the management of fetal growth restriction (FGR), published since 2015. Five protocols were chosen for data extraction. There were no relevant differences regarding the diagnosis and classification of FGR between the protocols. In general, all protocols suggest that the assessment of fetal vitality must be performed in a multimodally, associating biophysical parameters (such as cardiotocography and fetal biophysical profile) with the Doppler velocimetry parameters of the umbilical artery, middle cerebral artery, and ductus venosus. All protocols reinforce that the more severe the fetal condition, the more frequent this assessment should be made. The timely gestational age and mode of delivery to terminate the pregnancy in these cases can vary much between the protocols. Therefore, this paper presents, in a didactic way, the particularities of different protocols for monitoring FGR, in order to help obstetricians to better manage the cases.
-
Original Article
Tocolysis among Women with Preterm Birth: Associated Factors and Outcomes from a Multicenter Study in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):171-179
04-01-2018
Summary
Original ArticleTocolysis among Women with Preterm Birth: Associated Factors and Outcomes from a Multicenter Study in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):171-179
04-01-2018Views171See moreAbstract
Objective
To evaluate the use of tocolysis in cases of preterm birth due to spontaneous preterm labor in a Brazilian sample.
Methods
A sample of 1,491 women with preterm birth due to spontaneous preterm labor were assessed, considering treatment with tocolysis or expectant management, according to gestational age at birth (< 34 weeks and 34 to 36 þ 6 weeks) and drugs prescribed. The study took place in 20 Brazilian hospitals from April 2011 to July 2012. Bivariate analyses were conducted to evaluate associations with sociodemographic and obstetric characteristics and odds ratios with their respective 95% confidence intervals were estimated for maternal and neonatal outcomes.
Results
A total of 1,491 cases of preterm birth were considered. Tocolysis was performed in 342 cases (23%), 233 of which (68.1%) were delivered before 34 weeks. Within the expectant management group, 73% was late preterm and with more advanced labor at the time of admission. The most used drugs were calcium channel blockers (62.3%), followed by betamimetics (33%). Among the subjects in the tocolysis group, there were more neonatal and maternal complications (majority non-severe) and an occurrence of corticosteroid use that was 29 higher than in the expectant management group.
Conclusion
Tocolysis is favored in cases of earlier labor and also among thosewith less than 34 weeks of gestation, using preferably calcium channel blockers, with success in achieving increased corticosteroid use. Tocolysis, in general, was related to higher maternal and neonatal complication rates, which may be due to the baseline difference between cases at admission. However, these results should raise awareness to tocolysis use.
-
Systematic Review
Preterm Preeclampsia and Timing of Delivery: A Systematic Literature Review
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):622-631
11-01-2017
Summary
Systematic ReviewPreterm Preeclampsia and Timing of Delivery: A Systematic Literature Review
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(11):622-631
11-01-2017Views76See moreAbstract
Introduction
Preeclampsia, a multifactorial disease with pathophysiology not yet fully understood, is a major cause of maternal and perinatal morbidity and mortality, especially when preterm. The diagnosis is performed when there is an association between arterial hypertension and proteinuria or evidence of severity. There are unanswered questions in the literature considering the timing of delivery once preterm preeclampsia has been diagnosed, given the risk of developingmaternal complications versus the risk of adverse perinatal outcomes associated with prematurity. The objective of this systematic review is to determine the best timing of delivery for women diagnosed with preeclampsia before 37 weeks of gestation.
Methods
Systematic literature review, performed in the PubMed database, using the terms preeclampsia, parturition and timing of delivery to look for studies conducted between 2014 and 2017. Studies that compared the maternal and perinatal outcomes of women who underwent immediate delivery or delayed delivery, in the absence of evidence of severe preeclampsia, were selected.
Results
A total of 629 studies were initially retrieved. After reading the titles, 78 were selected, and their abstracts, evaluated; 16 were then evaluated in full and, in the end, 6 studies (2 randomized clinical trials and 4 observational studies) met the inclusion criteria. The results were presented according to gestational age range (< 34 weeks and between 34 and 37 weeks) and by maternal and perinatal outcomes, according to the timing of delivery, considering immediate delivery or expectant management. Before 34 weeks, thematernal outcomeswere similar, but the perinatal outcomes were significantly worse when immediate delivery occurred. Between 34 and 37 weeks, the progression to severe maternal disease was slightly higher among women undergoing expectant management, however, with better perinatal outcomes.
Conclusions
When there is no evidence of severe preeclampsia or impaired fetal wellbeing, especially before 34 weeks, the pregnancy should be carefully surveilled, and the delivery, postponed, aiming at improving the perinatal outcomes. Between 34 and 37 weeks, the decision on the timing of delivery should be shared with the pregnant woman and her family, after providing information regarding the risks of adverse outcomes associated with preeclampsia and prematurity.
-
Trabalhos Originais
Timing and frequency of prenatal visits: impact on the preterm delivery
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(1):25-32
05-02-1998
Summary
Trabalhos OriginaisTiming and frequency of prenatal visits: impact on the preterm delivery
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(1):25-32
05-02-1998DOI 10.1590/S0100-72031998000100005
Views52See moreIt is universally accepted that prenatal care has a beneficial impact on perinatal outcome. However, it is unclear whether access to early and frequent prenatal care influences the impact of pregnancy complications on birth weight. The objective of the present study was to determine the effectiveness of prenatal care, concerning antenatal visits (number and time of the first one), on gestational age and fetal weight at birth. We assessed prospectively the effect of the antenatal care in a group of 648 infants born consecutively at the University Hospital of Santa Maria, weighing from <1000 to >4000 g, and from <28 to >40 weeks of gestational age. Preterm delivery (<37 weeks) accounted for 17.7% of all deliveries, low birth-weight infants (<2500 g) for 20.5%, and very low birth-weight infants (<1000 g) for 2.8%. When the first antenatal visit was performed before the 12th week, only 5.1% of the babies were born with <37 weeks of gestational age or weight at birth of <2500 g. However, when the first visit was after the 28th week, the percentage of preterm delivery was 41.3% and of birth weight <2500 g was 43.5%. A significant association between higher frequency of antenatal visits, early care and decrease in preterm delivery frequency and low birth-weight infants was noted (p <0.001). We conclude that increase in the number of antenatal visits and early care can reduce the preterm delivery and low-birth weight infant rates.
-
Trabalhos Originais
Perinatal complications in pregnant women with and without bacterial vaginosis
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(8):437-441
04-05-1998
Summary
Trabalhos OriginaisPerinatal complications in pregnant women with and without bacterial vaginosis
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(8):437-441
04-05-1998DOI 10.1590/S0100-72031998000800002
Views98Purpose:to compare the incidence of preterm labor and birth, premature rupture of membranes (PROM) and low birth-weight newborns (< 2,500 g) between two groups of pregnant women (with or without BV). To verify the adequacy of including a regular prenatal BV investigation. Methods:a total of 217 women between 28 and 32 weeks of pregnancy (35 with BV and 182 without BV) were studied. The diagnosis of BV was established according to Amsel's criteria. The data were analyzed by the chi² test, Fisher's test, Mann-Whitney test and the relative risk. Results:the incidence of preterm labor, preterm birth, PROM and low birth-weight was statistically higher in the group of women with BV than in the control group (29.4% vs. 3.8%; 28.6% vs. 3.3%; 22.9% vs. 10.4%; 20.0% vs. 3.3%; respectively). The means of gestational age and birth-weight were significantly lower in the newborns from mothers with BV (265.8 days vs. 279.9 days; 2,958 g vs. 3,294 g, respectively). Conclusion:all perinatal complications studied were significantly associated with the presence of untreated BV during pregnancy. Therefore, the diagnosis and adequate treatment should be included in the routine prenatal assistance at Brazilian Obstetrics Services. Such measure may be effective in the reduction of these perinatal complications.
Key-words Bacterial vaginosisPregnancy complicationsPremature rupture of membranesPrematurityVulvovaginitisSee more -
Trabalhos Originais
Prevention of Preterm Birth: Role of Uterine Contraction Monitoring
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(9):509-515
05-22-1999
Summary
Trabalhos OriginaisPrevention of Preterm Birth: Role of Uterine Contraction Monitoring
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(9):509-515
05-22-1999DOI 10.1590/S0100-72031999000900003
Views36See morePurpose: to evaluate the relationship between uterine contractions and premature delivery. Methods: between February 1996 and July 1998, 73 high risk pregnant women for preterm delivery, between the 24th and 34th weeks of gestation, were submitted to uterine contraction monitoring with tokodynamometers for 1 hour twice a week. The positive test was the presence of 4 contractions/h before the 30th week of gestation, and after this time, 6 contractions/h. Result: of 73 women, 17 patients (23.28%) were excluded from the final analysis because they presented obstetric problems or unfavorable development for the final result. The rate of preterm delivery was 21.23% (13/56). The mean frequency of uterine contractions was greater in women with preterm delivery than in those with term delivery. The test presented sensitivity of 69.23%, specificity of 86.04%, positive predictive value of 60% and negative predictive value of 90.24%. Conclusion: negative tests are associated with a low risk of preterm birth. When the test is positive, association with other premature delivery markers is necessary to improve our ability to efficiently identify patients at risk for preterm delivery.


