-
Original Article02-13-2025
Anemia levels in the preconception period and the first trimester of pregnancy: a national, multicentric and cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:-e-rbgo1001
Abstract
Original ArticleAnemia levels in the preconception period and the first trimester of pregnancy: a national, multicentric and cross-sectional study
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:-e-rbgo1001
DOI 10.61622/rbgo/2025rbgo10001
Views278Abstract
Objective
The study aimed to determine the level of anemia in pregnant women in the first trimester and in the preconception period by conducting nationwide research.
Methods
The study was designed as retrospective, cross-sectional, and multicenter research. A total of 17 centers from 13 provinces were included in the study. The study was conducted with the participation of two groups of patients who applied to the obstetrics polyclinic between 1 January 2023 and 1 July 2023, who were in the first trimester of pregnancy and who were in the preconception period planning pregnancy.
Results
In total 4,265 women were included in the study. Of these women, 3,884 (91%) were in the first trimester of their pregnancy and 381 (9%) were in the preconception period. Anemia was detected in 24.1% (n=1030) of the patients. Of these patients, 20.6% (n=877) were pregnant women in the first trimester and 3.6% (n=153) were in the preconception period. A statistically significant and positive relationship was found between anemia and meat consumption frequency, educational status, and socioeconomic status of the patients (p=0.000, p=0.000, p=0.000). In addition, a statistically significant and negative correlation was determined between anemia and the number of pregnancies and the parity number (p=0.001, p=0.000) in both groups.
Conclusion
Anemia is a public health problem. Anemia has been determined to be an important problem both in the preconception period and early periods of pregnancy. It is necessary to revise the programs and interventions to reduce the prevalence of anemia and redesign them in line with current conditions.
Key-words Anemia, iron-deficiencypreconception carePregnancy complications, hematologicPregnancy trimester, firstSee more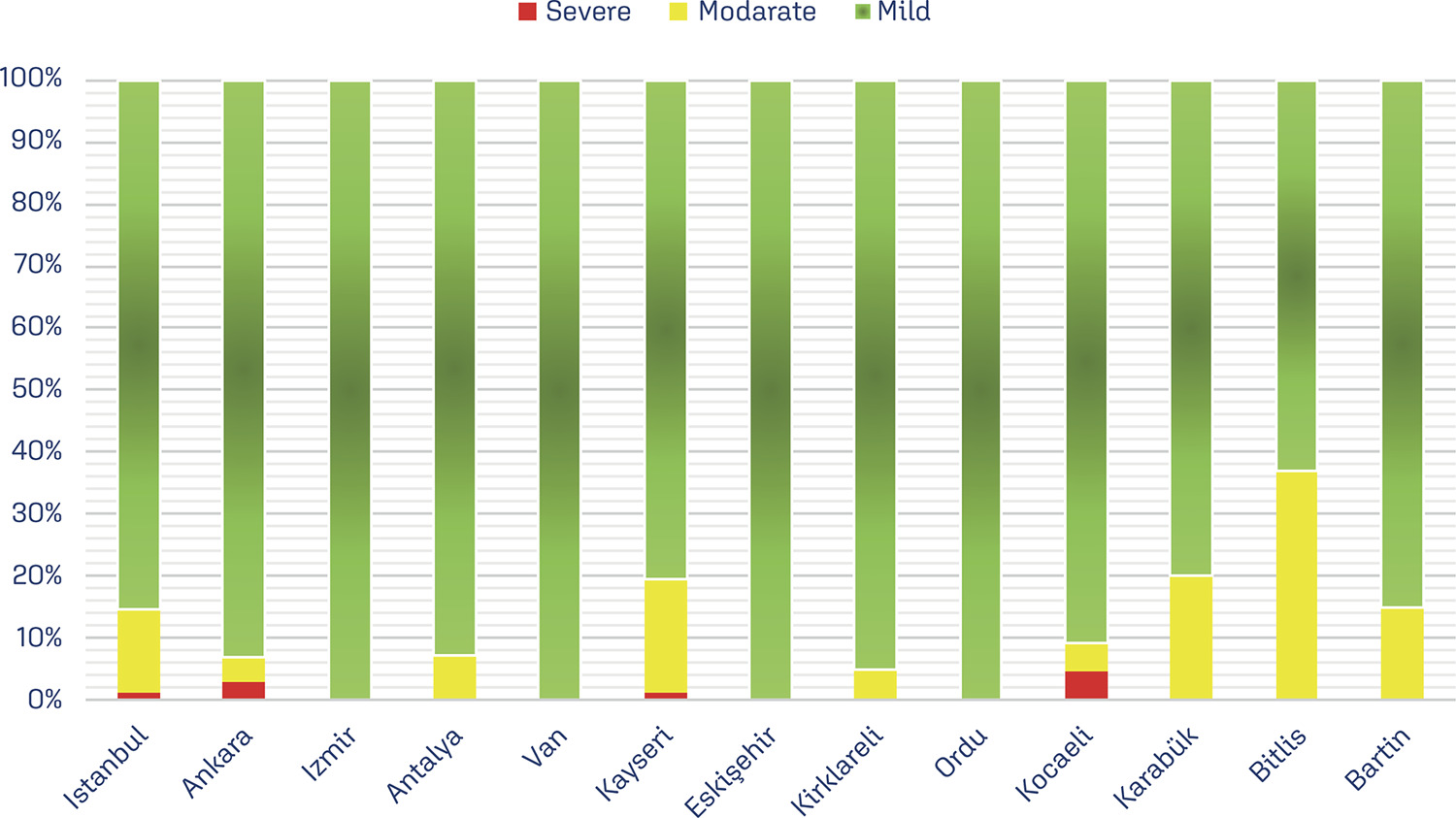
-
Original Article07-26-2024
Effect of subchorionic hematoma on first-trimester maternal serum free β-hCG and PAPP-A levels
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo66
Abstract
Original ArticleEffect of subchorionic hematoma on first-trimester maternal serum free β-hCG and PAPP-A levels
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo66
Views191Abstract
Objective
This study aimed to investigate the effects of the presence of subchorionic hematoma (SH) in early pregnancies with threatened miscarriage (TM) on levels of first-trimester maternal serum markers, pregnancy-associated plasma protein-A (PAPP-A), and free β-human chorionic gonadotropin (β-hCG) levels.
Methods
The data of TM cases with SH in the first trimester between 2015 and 2021 were evaluated retrospectively. The data of age and gestational age-matched TM cases without SH were also assessed to constitute a control group. Demographic characteristics, obstetric histories, ultrasonographic findings, and free β-hCG and PAPP-A levels of the groups were compared.
Results
There were 119 cases in the study group and 153 cases in the control group. The median vertical and longitudinal lengths of the SH were 31 mm and 16 mm. The median age of both groups was similar (p=0.422). The MoM value of PAPP-A was 0.088 (.93) in the study group and 0.9 (0.63) in the control group (p=0.519). Similarly, the MoM value of free β-hCG was 1.04 (0.78) in the study group and 0.99 (0.86) in the control group (p=0.66). No significant relationship was found in the multivariate analysis between free β-hCG MoM, PAPP-A MoM, age, gravida, and vertical and longitudinal lengths of the hematoma (p>0.05).
Conclusion
The level of PAPP-A and free β-hCG were not affected by the SH. Therefore, these markers can be used reliably in TM cases with SH for the first-trimester fetal aneuploidy screening test.
Key-words Abortion, threatenedAneuploidybiomarkersChorionic gonadotropinPregnancy trimester, firstPregnancy-associated plasma protein-ASubchorionic hematomaSee more -
Original Article06-30-2023
Changing Paradigms in the Initial Treatment of Ectopic Pregnancy at a University Hospital in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(4):192-200
Abstract
Original ArticleChanging Paradigms in the Initial Treatment of Ectopic Pregnancy at a University Hospital in Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(4):192-200
Views161See moreAbstract
Objective
To evaluate the use of different treatment options for ectopic pregnancy and the frequency of severe complications in a university hospital.
Methods
Observational study with women with ectopic pregnancy admitted at UNICAMP Womeńs Hospital, Brazil, between 01/01/2000 and 12/31/2017. The outcome variables were the type of treatment (first choice) and the presence of severe complications. Independent variables were clinical and sociodemographic data. Statistical analysis was carried out by the Cochran–Armitage test, chi-square test, Mann–Whitney test and multiple Cox regression.
Results
In total 673 women were included in the study. The mean age was 29.0 years (± 6.1) and the mean gestational age was 7.7 (± 2.5). The frequency of surgical treatment decreased significantly over time (z = -4.69; p < 0.001). Conversely, there was a significant increase in the frequency of methotrexate treatment (z = 4.73; p < 0.001). Seventy-one women (10.5%) developed some type of severe complication. In the final statistical model, the prevalence of severe complications was higher in women who were diagnosed with a ruptured ectopic pregnancy at admission (PR = 2.97; 95%CI: 1.61–5.46), did not present with vaginal bleeding (PR = 2.45; 95%CI: 1.41–4.25), had never undergone laparotomy/laparoscopy (PR = 6.69; 95%CI: 1.62–27.53), had a non-tubal ectopic pregnancy (PR = 4.61; 95%CI: 1.98–10.74), and do not smoke (PR = 2.41; 95%CI: 1.08–5.36).
Conclusion
there was a change in the first treatment option for cases of ectopic pregnancy in the hospital during the period of analysis. Factors inherent to a disease that is more difficult to treat are related to a higher frequency of severe complications.
-
Original Article06-01-2015
Right subclavian artery evaluation during first trimester ultrasound scan
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(6):252-257
Abstract
Original ArticleRight subclavian artery evaluation during first trimester ultrasound scan
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(6):252-257
DOI 10.1590/SO100-720320150005278
Views143PURPOSE:
To determine the feasibility of evaluation of the right subclavian artery during
the first trimester ultrasound scan, as well as to describe the technique for its
evaluation and, in case of aberrant right subclavian artery (ARSA) identification,
to determine its association with chromosomal abnormalities and/or cardiac
malformations and its management.METHODS:
A prospective study for evaluation of the right subclavian artery during the
first trimester ultrasound scan (crown-to-rump length between 45 and 84 mm), in
all consecutive single pregnancies, by a single examiner, using a Voluson E8
system (GE Healthcare, Zipf, Austria) with a 2 to 8 MHz RAB 4-8-D transabdominal
probe, within a short period of time (less than 2 minutes), in a general low risk
population. Color and/or power Doppler flow mapping was used to classify the right
subclavian artery as normal or aberrant. Regression analysis with the IBM SPSS
Statistics software for Windows, version 20.0 was used to determine the
significance of the association between failure to examine/classify the right
subclavian artery and both fetal crown-rump length and maternal body mass index.RESULTS :
Median maternal age was 30 years (range: 17-43 years) and median gestational age
at the time of evaluation of the right subclavian artery was 12 weeks (range:
11-13 weeks). The evaluation of the right subclavian artery was successful in
138/176 (78.4%) of the cases. ARSA was diagnosed in a single case (0.7%). This
fetus with ARSA also presented a hyperechogenic focus on the left cardiac
ventricle. Fetal echocardiography at 16 weeks of gestation was performed and
confirmed ARSA and the hyperechogenic focus. Amniocentesis revealed a normal 46,
XX karyotype.CONCLUSION:
ARSA can be identified during a routine first trimester ultrasound scan. Our
single ARSA case had a normal karyotype and no associated cardiac
malformations.Key-words Aorta, thoracicPregnancy trimester, firstprenatal diagnosisSubclavian arteryUltrasonographySee more -
Original Article10-10-2013
Reference range of uterine artery Doppler parameters between the 11th and 14th pregnancy weeks in a population sample from Northeast Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(8):357-362
Abstract
Original ArticleReference range of uterine artery Doppler parameters between the 11th and 14th pregnancy weeks in a population sample from Northeast Brazil
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(8):357-362
DOI 10.1590/S0100-72032013000800004
Views139PURPOSE: To establish reference values for the first trimester uterine artery resistance index (UtA-RI) and pulsatility index (UtA-PI) in healthy singleton pregnant women from Northeast Brazil. METHODS: A prospective observational cohort study including 409 consecutive singleton pregnancies undergoing routine early ultrasound screening at 11 - 14 weeks of gestation was performed. The patients responded to a questionnaire to assess maternal epidemiological characteristics. The left and right UtA-PI and UtA-RI were examined by color and pulsed Doppler by transabdominal technique and the mean UtA-PI, mean UtA-RI and the presence of bilateral protodiastolic notching were recorded. Quartile regression was used to estimate reference values. RESULTS: The mean±standard deviation UtA-RI and UtA-PI were 0.7±0.1 and 1.5±0.5, respectively. When segregated for gestation age, mean UtA-PI was 1.6±0.5 at 11 weeks, 1.5±0.6 at 12 weeks, 1.4±0.4 at 13 weeks and 1.3±0.4 at 14 weeks' gestation and mean UtA-RI was 0.7±0.1 at 11 weeks, 0.7±0.1 at 12 weeks, 0.6±0.1 at 13 weeks and 0.6±0.1 at 14 weeks' gestation. Uterine artery bilateral notch was present in 261 (63.8%) patients. We observed that the 5th and 95th percentiles of the UtA-PI and UtA-RI uterine arteries were 0.7 and 2.3 and, 0.5 and 0.8, respectively. CONCLUSION: Normal reference range of uterine artery Doppler in healthy singleton pregnancies from Northeast Brazil was established. The 95th percentile of UtA-PI and UtA-RI values may serve as a cut-off for future prediction of pregnancy complications studies (i.e., pre-eclampsia) in Northeast Brazil.
Key-words Fetal growth retardationPlacental circulationPre-eclampsiaPregnancy trimester, firstUltrasonography, dopplerSee more -
Original Article08-02-2013
Perinatal and pediatric follow up of children with increased nuchal translucency and normal karyotype
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(6):274-280
Abstract
Original ArticlePerinatal and pediatric follow up of children with increased nuchal translucency and normal karyotype
Revista Brasileira de Ginecologia e Obstetrícia. 2013;35(6):274-280
DOI 10.1590/S0100-72032013000600007
Views78PURPOSE: To analyze the perinatal and pediatric outcome of fetuses that showed nuchal translucency (NT) above the 95th percentile (P95) and a normal karyotype in order to obtain data allowing better maternal prenatal counseling. METHODS: fetuses from a tertiary obstetric service with an NT above P95 and a normal karyotype were analyzed between 2005 and 2011. We analyzed gestational ultrasound follow-up, fetal and postnatal echocardiography (ECHO), weight, length and Apgar score at birth, and neuropsychomotor development by the Ages and Stages Questionnaire (ASQ) up to July 2012. RESULTS: During this period, there were 116 cases of nuchal translucency above the 95th percentile, and the fetal karyotype was determined in 79 of them (68%). Forty-three analyses were normal (54.4%) and 36 were altered (45.6%). Among the fetuses with a normal karyotype, one was miscarried at 15 weeks of gestation with Cantrel pentalogy and one died at 24 weeks with several structural abnormalities. There was one neonatal death of unknown cause and two cases of intraventricular communication (IVC) detected by fetal ECHO. Postnatal echocardiography revealed the persistence of IVC in one case and one case of atrial septal defect (ASD) and patent ductus arteriosus (PDA). Of the 40 surviving children, only 1 showed delayed speech development and another presented autism. The remaining cases resulted in normal neurodevelopment. CONCLUSION: During the monitoring of fetuses with increased NT and a normal karyotype, parents can be best advised that when a 2nd trimester morphological-echocardiography ultrasound study is normal, the probability of the child being born alive and well is high (93.5%).
Key-words Child developmentCongenital abnormalitiesHeart defects, congenitalKaryotypeNuchal translucency measurementPregnancy trimester, firstUltrasonography, prenatalSee more -
Original Article01-20-2010
Echographic characteristics of the corpus luteum in early pregnancy: morphology and vascularization
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(11):549-555
Abstract
Original ArticleEchographic characteristics of the corpus luteum in early pregnancy: morphology and vascularization
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(11):549-555
DOI 10.1590/S0100-72032010001100006
Views106See morePURPOSE: the purpose of this research was to evaluate the morphological aspects and vasculature of the corpus luteum (CL) based on ultrasound parameters during early pregnancy and to assess their relationship with early pregnancy loss. METHODS: this was a prospective cohort study of 90 pregnant patients between 6 and 8 weeks plus 6 days weeks of gestation. We included women at low risk, without acute or chronic systemic disease and with spontaneous conception. Exclusion criteria: use of drugs or smoking, drugs inducing ovulation, history of more than one abortion, no heartbeat visible in the embryo and impossibility of visualization of the corpus luteum. The size, volume, morphological aspects, resistive index, and peak systolic velocity of the corpus luteum were measured by transvaginal sonography. RESULTS: ninety patients were included in the study. Maternal age ranged from 15 to 41 years (mean 28.6±5.8 years). The corpus luteum could be visualized in 87 patients (96.7%), 79 patients had normal pregnancies (90.1%), whereas spontaneous losses occurred in 8 cases (9.9%). In a comparison of the survivors and losses, there was no difference in mean CL diameter (21.8 versus 20.0 mm; p=0.108, Mann-Whitney test), mean CL volume (4.2 versus 3.0 cm³; p=0.076, Mann-Whitney test), mean resistive index (0.55 versus 0,58; p=0.220, Mann-Whitney test), peak systolic velocity (15 versus 15 cm/s; p=0.757, Mann-Whitney test). There was a positive relation between maternal age and resistive index. CONCLUSIONS: no apparent correlation was found between the morphological and vascular aspects of the corpus luteum in early normal pregnancies and first-trimester pregnancy losses.
-
Original Article11-27-2008
Embryo volume estimated by three-dimensional ultrasonography at seven to ten weeks of pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(10):499-503
Abstract
Original ArticleEmbryo volume estimated by three-dimensional ultrasonography at seven to ten weeks of pregnancy
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(10):499-503
DOI 10.1590/S0100-72032008001000004
Views144PURPOSE: to evaluate the embryo's volume (EV) between the seventh and the tenth gestational week, through tridimensional ultrasonography. METHODS: a transversal study with 63 normal pregnant women between the seventh and the tenth gestational week. The ultrasonographical exams have been performed with a volumetric abdominal transducer. Virtual Organ Computer-aided Analysis (VOCAL) has been used to calculate EV, with a rotation angle of 12º and a delimitation of 15 sequential slides. The average, median, standard deviation and maximum and minimum values have been calculated for the EV in all the gestational ages. A dispersion graphic has been drawn to assess the correlation between EV and the craniogluteal length (CGL), the adjustment being done by the determination coefficient (R²). To determine EV's reference intervals as a function of the CGL, the following formula was used: percentile=EV+K versus SD, with K=1.96. RESULTS: CGL has varied from 9.0 to 39.7 mm, with an average of 23.9 mm (±7.9 mm), while EV has varied from 0.1 to 7.6 cm³, with an average of 2.7 cm³ (±3.2 cm³). EV was highly correlated to CGL, the best adjustment being obtained with quadratic regression (EV=0.2-0.055 versus CGL+0.005 versus CGL²; R²=0.8). The average EV has varied from 0.1 (-0.3 to 0.5 cm³) to 6.7 cm³ (3.8 to 9.7 cm³) within the interval of 9 to 40 mm of CGL. EV has increased 67 times in this interval, while CGL, only 4.4 times. CONCLUSIONS: EV is a more sensitive parameter than CGL to evaluate embryo growth between the seventh and the tenth week of gestation.
Key-words Crown-rump lengthEmbryonic structuresImagingPregnancy trimester, firstReference valuesthree-dimensionalSee more


