-
Original Article01-24-2021
IgG Avidity in Samples Collected on Filter Paper: Importance of The Early Diagnosis of Congenital Toxoplasmosis
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):887-893
Abstract
Original ArticleIgG Avidity in Samples Collected on Filter Paper: Importance of The Early Diagnosis of Congenital Toxoplasmosis
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):887-893
Views201See moreAbstract
Objective
The purpose of the present study is to standardize and evaluate the use of the immunoglobulin G (IgG) antibody avidity test on blood samples from newborns collected on filter paper to perform the heel test aiming at its implementation in ongoing programs.
Methods
Blood samples from newborns were collected on filter paper simultaneously with the heel prick test. All samples were subjected to immunoglobulin M IgM and IgG enzyme-linked immunosorbent assays (ELISA). Peripheral blood was collected again in the traditional way and on filter paper from newborns with high IgG levels (33). Three types of techniques were performed, the standard for measuring IgG in serum, adapted for filter paper and the technique of IgG avidity in serum and on filter paper. The results of the avidity test were classified according to the Rahbari protocol.
Results
Among the 177 samples, 17 were collected in duplicate from the same child, 1 of peripheral blood and 1 on filter paper. In this analysis, 1 (5.88%) of the 17 samples collected in duplicate also exhibited low IgG avidity, suggesting congenital infection. In addition, the results obtained from serum and filter paper were in agreement, that is, 16 (94.12%) samples presented high avidity, with 100% agreement between the results obtained from serum and from filter paper.
Conclusion
The results of the present study indicate that the avidity test may be another valuable method for the diagnosis of congenital toxoplasmosis in newborns.
-
Original Article01-24-2021
Uterine Artery Pulsatility Index as a Pre-eclampsia Predictor in the 3 Trimesters in Women with Singleton Pregnancies
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):904-910
Abstract
Original ArticleUterine Artery Pulsatility Index as a Pre-eclampsia Predictor in the 3 Trimesters in Women with Singleton Pregnancies
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):904-910
Views230See moreAbstract
Objective
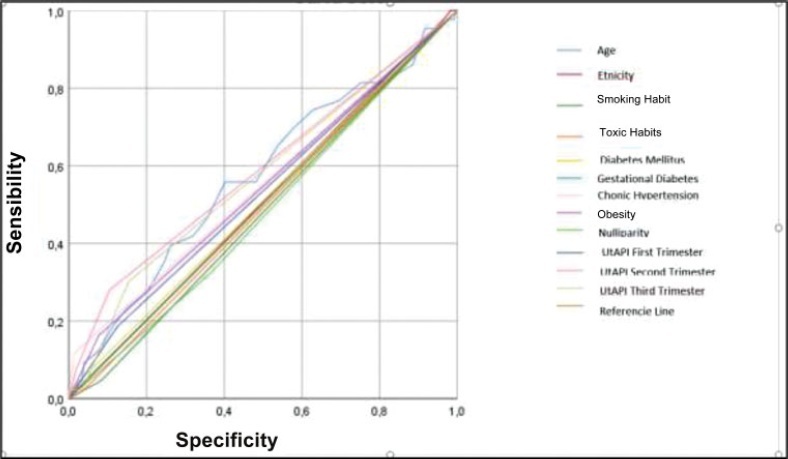
To evaluate the mean uterine artery pulsatility index (UtAPI) in each trimester of pregnancy as a predictor of early or late pre-eclampsia (PE) in Colombian pregnant women.
Methods
The UtAPI was measured in singleton pregnancies in each trimester. Uterine artery pulsatility index as predictor of PE was evaluated by odds ratio (OR), receiver operating characteristic (ROC) curves, and Kaplan-Meier diagram.
Results
Analysis in the 1st and 3rd trimester showed that abnormal UtAPI was associated with early PE (OR: 5.99: 95% confidence interval [CI]: 1.64–21.13; and OR: 10.32; 95%CI: 2.75–42.49, respectively). Sensitivity and specificity were 71.4 and 79.6%, respectively, for developing PE (area under the curve [AUC]: 0.922). The Kaplan-Meier curve showed that a UtAPI of 0.76 (95%CI: 0.58–1.0) in the 1st trimester was associated with early PE, and a UtAPI of 0.73 (95%CI: 0.55–0.97) in the 3rd trimester was associated with late PE.
Conclusion
Uterine arteries proved to be a useful predictor tool in the 1st and 3rd trimesters for early PE and in the 3rd trimester for late PE in a pregnant population with high prevalence of PE.
-
Original Article01-24-2021
Increased Risk for Maternal Anxiety during the COVID-19 Outbreak in Brazil among Pregnant Women without Comorbidities
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):932-939
Abstract
Original ArticleIncreased Risk for Maternal Anxiety during the COVID-19 Outbreak in Brazil among Pregnant Women without Comorbidities
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):932-939
Views164Abstract
Objective
To study maternal anxiety in pregnant women without comorbidities in the context of the COVID-19 outbreak in Brazil and to study maternal knowledge and concerns about the pandemic.
Methods
This is a secondary analysis from a national multicenter cross-sectional study performed in 10 cities, from June to August, 2020, in Brazil. Interviewed postpartum women, without medical or obstetrical comorbidities, were included in the present subanalysis. A structured questionnaire and the Beck Anxiety Inventory (BAI) were applied.
Results
Out of the 1,662 women, 763 (45.9%) met the criteria for the current analysis and 16.1% presented with moderate and 11.5% with severe maternal anxiety. Moderate or severe maternal anxiety was associated with high school education (odds ratio [OR]:1.58; 95% confidence interval [CI]:1.04–2.40). The protective factor was cohabiting with a partner (OR: 0.46; 95%CI: 0.29–0.73). There was a positive correlation between the total BAI score and receiving information about care in the pandemic (rpartial 0.15; p < 0.001); concern about vertical transmission of COVID-19 (rpartial 0.10; p = 0.01); receiving information about breastfeeding (rpartial 0.08; p = 0.03); concerns about prenatal care (rpartial 0.10; p = 0.01), and concerns about the baby contracting COVID-19 (rpartial 0.11; p = 0.004). The correlation was negative in the following aspects: self-confidence in protecting from COVID-19 (rpartial 0.08; p = 0.04), having learned (rpartial 0.09; p = 0.01) and self-confidence in breastfeeding (rpartial 0.22; p < 0.001) in the context of the pandemic.
Conclusion
The anxiety of pregnant women without medical or obstetrical comorbidities was associated to high school educational level and not living with a partner during the COVID-19 pandemic. Self-confidence in protecting against COVID-19 and knowledge about breastfeeding care during the pandemic reduced maternal anxiety.
Key-words Breastfeedingchildbirthcoronavirus disease 2019Maternal anxietypandemicPostpartumPregnancyQuestionnairesSee more -
Review Article01-24-2021
Clinical and Obstetric Aspects of Pregnant Women with COVID-19: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):949-960
Abstract
Review ArticleClinical and Obstetric Aspects of Pregnant Women with COVID-19: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(12):949-960
Views210See moreAbstract
Objective
To analyze the clinical and obstetric aspects of pregnant women with COVID-19.
Methods
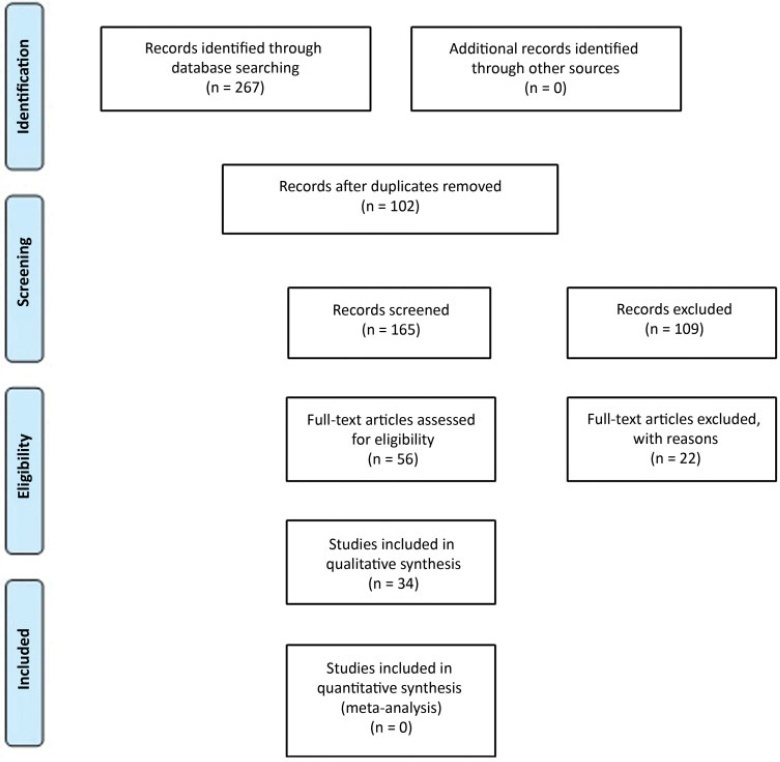
A systematic literature review in the MEDLINE/PubMed, LILACS, SCIELO, and CNKI databases was performed from March to May 2020, with the descriptors: Pregnancy; 2019-nCov; Coronavirus; SARS-Cov-2, Covid-19. Of those chosen were original titles, without language and period restriction and that addressed pregnant women with a clinical and/or laboratory diagnosis of COVID-19. Revisions, editorials, and duplicate titles were excluded. The Newcastle-Ottawa (NOS) and Murad et al. scales were used to assess the quality of the studies.
Results
We included 34 articles with 412 pregnant women infected with severe acute respiratory syndrome (SARS-Cov-2), with an average age of 27.5 years of age and 36.0 gestational weeks. The most common symptom was fever (205 [49.7%]), and 89 (21.6%) pregnant women progressed to severe viral pneumonia. Laboratory tests showed an increase in C-reactive protein (154 [37.8%]), and radiological tests showed pneumonia with peripheral ground-glass pattern (172 [51.4%]). Emergency cesarean delivery was indicated for most pregnant women, and the most common gestational complication was premature rupture of ovarian membranes (14 [3.4%;]). We detected 2 (0.5%) neonatal deaths, 2 (0.5%) stillbirths, and 1 (0.2%) maternal death.
Conclusion
Pregnant women with COVID-19 presented a clinical picture similar to that of non-infected pregnant women, with few obstetric or neonatal repercussions. There was a greater indication of cesarean deliveries before the disease aggravated, and there was no evidence of vertical transmission of the infection.
-
Review Article12-17-2021
Association of the Maternal Folic Acid Supplementation with the Autism Spectrum Disorder: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(10):775-781
Abstract
Review ArticleAssociation of the Maternal Folic Acid Supplementation with the Autism Spectrum Disorder: A Systematic Review
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(10):775-781
Views296See moreAbstract
Objective
To analyze the scientific production regarding maternal folic acid (FA) supplementation and its relationship with autistic spectrum disorder (ASD).
Data Sources
We performed unrestricted electronic searches in the BIREME virtual bank, Virtual Health Library (VHL) and Medical Literature Analysis and Retrieval System Online (MEDLINE/PubMed) databases.
Selection of Studies
For sample selection, articles that met the proposed objectives were included, published in English, Spanish and Portuguese, the use of Health Sciences Descriptors (DeCS): autistic OR autism AND autism spectrum disorder AND folic acid, AND, with the use of the Medical Subject Headings (MeSH): autistic OR autism AND autistic spectrum disorder AND folic acid.
Data Collection
Data extraction was performed by the reviewers with a preestablished data collection formulary.
Data Synthesis
The Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) was used based on a checklist with 27 items and a 4-step flowchart.
Results
A total of 384 articles was found by the search strategies, of which 17 were eligible following the pre-established criteria. The main findings of the present review point to maternal FA supplementation in the pre-conception period and beginning of pregnancy as a protective effect in relation to ASD, which should be indicated in this period as prevention to the problem.
Conclusion
According to the research analyzed, more studies are necessary to know its effects on pregnancy, since the consumption of excessive FA may not be innocuous.
-
Review Article12-17-2021
Oral Iron Supplementation in Pregnancy: Current Recommendations and Evidence-Based Medicine Suplementação oral de ferro na gravidez: recomendações atuais e medicina baseada na evidência
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(10):782-788
Abstract
Review ArticleOral Iron Supplementation in Pregnancy: Current Recommendations and Evidence-Based Medicine Suplementação oral de ferro na gravidez: recomendações atuais e medicina baseada na evidência
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(10):782-788
Views414See moreAbstract
Objective
To review the evidence about universal iron supplementation in pregnancy to prevent maternal anemia.
Methods
Bibliographic research of randomized and controlled clinical trials, meta-analyses, systematic reviews, and clinical guidelines, published between August 2009 and August 2019, using the MeSH terms: iron; therapeutic use; pregnancy; anemia, prevention and control.
Results
We included six clinical guidelines, three meta-analyses and one randomized controlled clinical trial.
Discussion
Most articles point to the improvement of hematological parameters and reduction of maternal anemia risk, with supplementary iron. However, they do not correlate this improvement in pregnant women without previous anemia with the eventual improvement of clinical parameters.
Conclusion
Universal iron supplementation in pregnancy is controversial, so we attribute a SORT C recommendation strength.
-
Original Article12-17-2021
The Assessment of Vitamin D Levels in Pregnant Women is not Associated to Fetal Growth Restriction: A Cross Sectional Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(10):743-748
Abstract
Original ArticleThe Assessment of Vitamin D Levels in Pregnant Women is not Associated to Fetal Growth Restriction: A Cross Sectional Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(10):743-748
Views254See moreAbstract
Objective
To assess maternal serum levels of vitamin D in fetuses appropriate for gestational age (AGA), small for gestational age (SGA), and with fetal growth restriction (FGR) according to estimated fetal weight (EFW).
Methods
This cross-sectional study included 87 pregnant women between 26 and 36 weeks of gestation: 38 in the AGA group, 24 in the SGA group, and 25 in the FGR group. Maternal serum vitamin D levels were assessed using the chemiluminescence method. The Fisher exact test was used to compare the results between the groups.
Results
The mean ± standard deviation (SD) of maternal age (years) and body mass index (kg/m2) in the AGA, SGA, and FGR groups were 25.26 8.40 / 26.57 ± 4.37; 25.04 ± 8.44 / 26.09 ± 3.94; and 25.48 ± 7.52 / 26.24 ± 4.66, respectively (p > 0.05). The maternal serum vitamin D levels (mean ± SD) of the AGA, SGA, and FGR groups were 22.47 ± 8.35 ng/mL, 24.80 ± 10.76 ng/mL, and 23.61 ± 9.98 ng/mL, respectively, but without significant differences between the groups (p = 0.672).
Conclusion
Maternal serum vitamin D levels did not present significant differences among pregnant women with AGA, SGA, or FGR fetuses between 26 and 36 weeks of gestation according to EFW.
-
Original Article11-15-2021
COVID-19 in Pregnancy: Implication on Platelets and Blood Indices
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):595-599
Abstract
Original ArticleCOVID-19 in Pregnancy: Implication on Platelets and Blood Indices
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(8):595-599
Views169See moreAbstract
Objective
To describe the hematological changes, the platelet indices in particular, in pregnant women with coronavirus disease 2019 (COVID-19) compared to healthy pregnant women.
Methods
A retrospective case-control study conducted at the Al Yarmouk Teaching Hospital, in Baghdad, Iraq, involving 100 pregnant women, 50 with positive viral DNA for COVID-19 (case group), and 50 with negative results (control group); both groups were subjected to a thorough hematological evaluation.
Results
Among the main hematological variables analyzed, the platelet indices, namely the mean platelet volume (MPV) and the platelet distribution width (PDW), showed statistically significant differences (MPV: 10.87±66.92 fL for the case group versus 9.84±1.2 fL for the control group; PDW: 14.82±3.18 fL for the case group versus 13.3±2.16 fL for the controls). The criterionvalue of the receiver operating characteristic (ROC) curve forPDWat a cutoffpoint of>11.8 fL showed a weak diagnostic marker, while the MPV at a cutoff value of>10.17 fL showed a good diagnostic marker.
Conclusion
The MPV and PDW are significantly affected by the this viral infection, even in asymptomatic confirmed cases, and we recommend that both parameters be included in the diagnostic panel of this infection.


