Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo9
00-00-2024
To analyze the amount of muscle and the presence of sarcopenia in postmenopausal women using different methods, verifying the agreement between them as to skeletal muscle mass (SMM).
This cross-sectional observational study was conducted with postmenopausal women aged ≥ 50 years. SMM was obtained from a predictive equation, Bioelectrical Impedance (BIA), and Dual Energy X-Ray Absorptiometry (DXA). The skeletal muscle mass index (SMI) and the appendicular skeletal muscle mass index (ASMI) were calculated. The cut-off point of SMI was determined for the population itself. The agreement between the SMI obtained using the different methods was verified. Sarcopenia was diagnosed according to the criteria proposed by the European Working Group on Sarcopenia in Older People 2 (EWGSOP2). The significance level adopted for all tests was 5.0%.
A total of 112 women were evaluated, with an average age of 66.1 ± 5.65 years. Among them, 51.8% were sufficiently active and 43.8% were overweight and obese. The SMI cut-offs were 6.46 kg/m2 for the predictive equation and 7.66 kg/m2 for BIA, with high sensitivity and specificity. There was an excellent agreement in the identification of SMM by the predictive equation (0.89 [0.824-0.917], p < 0.001) and BIA (0.92 [0.883-0.945], p < 0.001), in reference to DXA. The prevalence of sarcopenia was 0.9%, 1.8%, and 2.7% according to BIA, DXA, and the predictive equation, respectively.
The predictive equation showed the expected agreement in estimating skeletal muscle mass in postmenopausal women, offering a viable and accurate alternative.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(10):594-602
12-11-2023
Adhesive capsulitis is a condition characterized by shoulder pain and stiffness. Breast cancer treatment has been linked to the development of this condition, but its mechanisms are still little known. This study's objective was to identify predictors factors associated with the development of adhesive capsulitis in breast cancer patients.
A case control study was performed with women undergoing treatment for breast cancer in a single center. The sampling was nonprobabilistic and consecutive. Adhesive capsulitis was defined as constant pain associated with decreased active and passive shoulder movement in anterior elevation, external rotation at 0°/90° abduction, and internal rotation at 90° abduction. The study group consisted of patients with shoulder pain and range of motion limitations, while the control group consisted of women without any shoulder abnormalities. Sociodemographic and clinical variables were collected. A univariate logistic regression was used to assess the influence of variables on the studied outcome. For p< 0.20, a multivariate logistic regression was used. The probability of null hypothesis rejection was 5%.
A total of 145 women were assessed, with 39 (26.9%) on the study group and 106 (73.1%) on the control group. The majority was under 60 years old. In the multivariate analysis, variables correlated to the outcome under study were shoulder immobilization (OR = 3.09; 95% CI: 1.33–7.18; p = 0.009), lymphedema (OR = 5.09; 95% CI: 1.81–14.35; p = 0.002), and obesity (OR = 3.91; 95% CI: 1.27–12.01; p = 0.017).
Lymphedema, postsurgery immobilization, and obesity are predictive factors for the development of adhesive capsulitis in breast cancer patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(2):082-088
07-10-2023
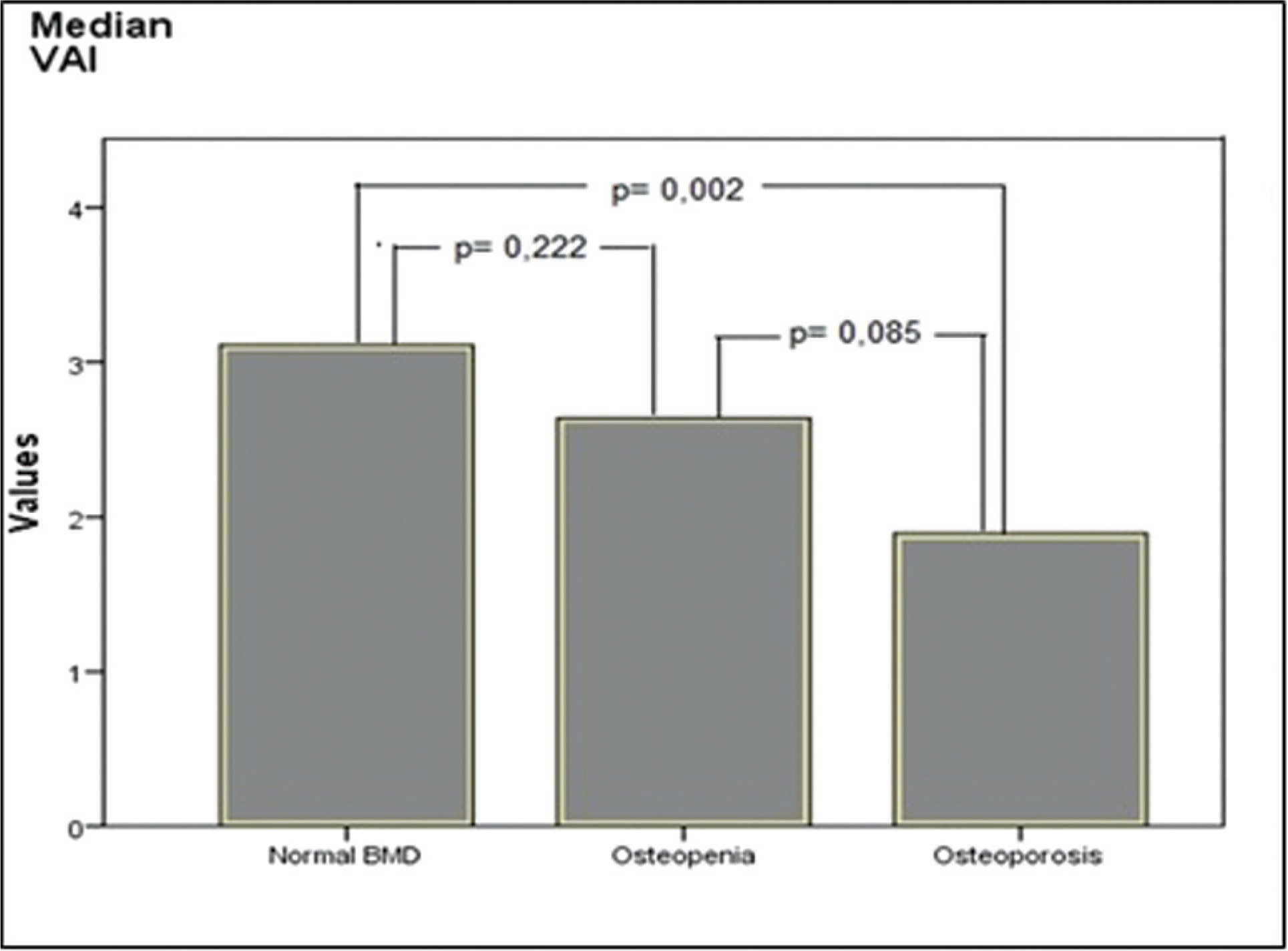
It was aimed to compare visceral adiposity index (VAI) levels in patients with normal bone mineral density (BMD), osteopenia, and osteoporosis.
One hundred twenty postmenopausal women (40 with normal BMD, 40 with osteopenia, and 40 with osteoporosis) between the ages of 50 to 70 years were included in the study. For females, the VAI was calculated using the formula (waist circumference [WC]/[36.58 + (1.89 x body mass index (BMI))]) x (1.52/High-density lipoprotein [HDL]-cholesterol [mmol/L]) x (triglyceride [TG]/0.81 [mmol/L]).
The time of menopause from the beginning was similar in all groups. Waist circumference was found to be higher in those with normal BMD than in the osteopenic and osteoporotic groups (p = 0.018 and p < 0.001, respectively), and it was also higher in the osteopenic group than in the osteoporotic group (p = 0.003). Height and body weight, BMI, blood pressure, insulin, glucose, HDL-cholesterol, and homeostasis model assessment-insulin resistance (HOMA-IR) levels were similar in all groups. Triglyceride levels were found to be higher in the normal BMD group, compared with the osteoporotic group (p = 0.005). The level of VAI was detected as higher in those with normal BMD, compared with the women with osteoporosis (p = 0.002). Additionally, the correlation analysis showed a positive correlation between dual-energy X-ray absorptiometry (DXA) spine T-scores, WC, VAI, and a negative correlation between DXA spine T-scores and age.
In our study, we found higher VAI levels in those with normal BMD, compared with women with osteoporosis. We consider that further studies with a larger sample size will be beneficial in elucidating the entity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(12):1117-1121
03-24-2022
Although obesity can result in high morbidity and mortality in surgical outcomes because of multiple comorbidities, determinants of outcome in obese patients who underwent endometrial cancer surgery remain unclear. The aim of this study is to assess the relationship between body mass index (BMI) and surgical outcomes in obese patients with endometrial cancer.
An institutional retrospective review of the demographic details, clinical characteristics, and follow-up data of 142 patients with endometrial cancer who underwent surgery during a 72-month period was performed. The patients were divided into three groups based on their BMI; patients with BMI < 25 were identified as normal weight, patients with BMI between 25 and 30 were accepted as overweight, and those with BMI ≥ 30 kg/m2 were identified as obese. The groups' demographic and clinical variables were compared.
Of the 142 patients, 42 were in the normal weight group, 55 in the overweight group, and 45 in the obese group. Age, surgical procedures, blood loss, preoperative health status, and metastatic lymph nodes did not show a significant difference between groups. However, surgery time and total lymph nodes were higher in the obese group. (p = 0.02, p = 0.00, and p = 0.00, respectively). Common complications were anemia, fever, intestinal injury, deep vein thrombosis, fascial dehiscence and urinary infection. There was no significant difference according to the complications.
Our results indicated that higher BMI was significantly associated with a longer duration of endometrial cancer surgery. Minimally invasive surgeries and conventional laparotomy could be performed safely in obese patients.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(6):586-592
08-15-2022
To determine if there is a correlation between body mass index (BMI) and climacteric symptoms in postmenopausal women.
The study sample was composed of 109 postmenopausal women with a mean age of 57 ± 8 years, mean body mass index (BMI) of 30 ± 6 kg/m2, and 8 ± 8 years after menopause. For the assessment of the climacteric symptoms, the Blatt-Kupperman Index (BKI), the Menopause Rating Scale (MRS), and the Cervantes Scale (CS) were used. Data analysis was performed through the Chi-squared test, analysis of variance (ANOVA) with the Bonferroni post hoc test, and multiple linear regression. The level of significance adopted was of p < 0.05. The statistical analyses were performed using the Statistical Package for the Social Sciences (IBM SPSS Statistics for Windows, IBM Corp., Armonk, NY, United States) software, version 26.0.
The multiple linear regression showed a positive association (p<0.01) between BMI values and menopause symptoms when adjusted for age and time after menopause in the 3 questionnaires used (BKI: B = 0.432; CS: B = 304; and MRS: B = 302). Regarding symptom scores, the obese women had higher mean scores (p<0.05) when compared to eutrophic women (BKI = 28 ± 10 and 20 ± 10; and MRS = 20 ± 10 and 13±7, respectively). In the Chi-squared analysis, 28% of obese women had severe symptoms and 46% had moderate symptoms, while only 1% and 46% of eutrophic women had these same symptoms.
There is an association between BMI and climacteric symptoms, and overweight or obese women have more intense and moderate symptoms than eutrophic women.