-
Case Report04-01-2016
Prenatal Diagnosis of Lissencephaly Type 2 using Three-dimensional Ultrasound and Fetal MRI: Case Report and Review of the Literature
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(4):201-206
Abstract
Case ReportPrenatal Diagnosis of Lissencephaly Type 2 using Three-dimensional Ultrasound and Fetal MRI: Case Report and Review of the Literature
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(4):201-206
Views209Abstract
Lissencephaly is a genetic heterogeneous autosomal recessive disorder characterized by the classical triad: brain malformations, eye anomalies, and congenital muscular dystrophy. Prenatal diagnosis is feasible by demonstrating abnormal development of sulci and gyri. Magnetic resonance imaging (MRI) may enhance detection of developmental cortical disorders as well as ocular anomalies. We describe a case of early diagnosis of lissencephaly type 2 detected at the time of routine second trimester scan by three-dimensional ultrasound and fetal MRI. Gross pathology confirmed the accuracy of the prenatal diagnosis while histology showed the typical feature of cobblestone cortex. As the disease is associated with poor perinatal prognosis, early and accurate prenatal diagnosis is important for genetic counseling and antenatal care.
Key-words cobblestone cortexGenetic counselinglissencephalyMagnetic resonance ImagingPathologyprenatal diagnosisthree-dimensional ultrasoundSee more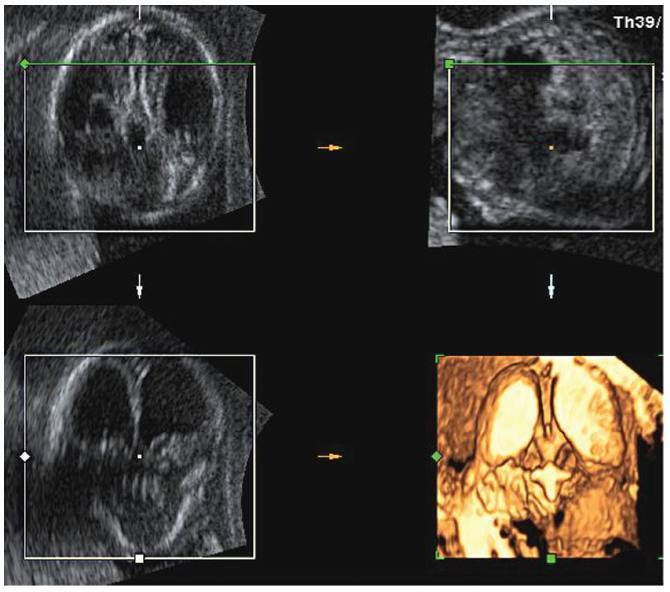
-
Original Article01-20-2010
Uterine fibroid embolization in women with giant fibroids
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(11):530-535
Abstract
Original ArticleUterine fibroid embolization in women with giant fibroids
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(11):530-535
DOI 10.1590/S0100-72032010001100003
Views149PURPOSE: to evaluate the effectiveness of uterine fibroid embolization (UFE) in patients with giant fibroids, with regard to both clinical outcomes and size reduction. METHODS: twenty-six patients with a mean age of 36.5 years, carrying symptomatic fibroids with a volume over 1,000 cm³, were referred for UFE. All patients had indication for percutaneous treatment. The procedures were performed under epidural anesthesia and sedation, using an institutional protocol. By unilateral femoral access, selective catheterization of uterine arteries and infusion of calibrated microspheres through microcatheter were carried out. Clinical evaluation was performed by means of regular outpatient gynecology consultation. All patients underwent magnetic resonance imaging (MRI) before the procedure and 15 patients underwent control MRI after 6 months. RESULTS: technical success was 100%. There was no complication related to the procedures. Mean uterine volume of the 15 patients studied was 1,401 cm³ before embolization (min 1,045 cm³, max 2,137 cm³) and 799 cm³ after 6 months (525 cm³ min, max. 1,604 cm³), resulting in a total reduction of 42.9%. Clinical improvement was observed in 25 of 26 patients. One woman with uterine volume of 1,098 cm³ who developed necrosis and partial fibroid expulsion underwent myomectomy. Another patient was submitted to myomectomy six months after the procedure because she wanted to become pregnant, despite partial fibroid size reduction. One patient with a uterine volume of 2,201 cm³ required a second intervention to achieve an adequate angiographic result. No patient underwent hysterectomy. On average, 9.2 microsphere syringes were used per patient. CONCLUSION: embolization of giant uterine fibroids is a feasible procedure with acceptable clinical and radiological outcomes. It can be considered an option for patients who desire to preserve the uterus, and it may serve as adjuvant therapy for high-risk myomectomy.
Key-words Angiography, digital subtractionEmbolization, therapeuticHysterectomyMagnetic resonance ImagingUterine artery embolizationUterine fibroidsSee more -
Original Article11-19-2009
Sternalis muscle simulating a breast nodule
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(10):492-495
Abstract
Original ArticleSternalis muscle simulating a breast nodule
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(10):492-495
DOI 10.1590/S0100-72032009001000004
Views147PURPOSE: to report a series of three cases of a normal variation known as sternal muscle, simulating a breast lesion. METHODS: the diagnostic suspicion was based on the clinical picture, findings in the physical examination and imaging, being confirmed by sectional imaging methods such as computerized tomography (CT) and magnetic resonance imaging (MRI). A review of the literature has been made in the data Medline and in breast radiology textbooks about the anatomic, clinical and imaging aspects of the sternal muscle. RESULTS: three female patients, without complaints, who presented nodular breast lesions in the medial quadrants projection (two in a routine mammographic exam and one in a computerized tomography). The diagnosis of sternal muscle was confirmed through breast MRI or through thoracic CT, showing an elongated image in the left parasternal region, adjacent to the breast muscle. CONCLUSIONS: the sternal muscle is an unusual variation of the muscles of the thoracic wall, present in about 2 to 8% of the population. The knowledge of this entity is crucial, as it can simulate a breast node.
Key-words Breast deseasesBreast neoplasmsDiagnosis, differentialMagnetic resonance ImagingMammographyMusclesThoracic wallTomography, X-ray computedSee more -
Case Report02-04-2008
Lymphoma of the uterine cervix: report of two cases and review of the literature
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(12):626-630
Abstract
Case ReportLymphoma of the uterine cervix: report of two cases and review of the literature
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(12):626-630
DOI 10.1590/S0100-72032008001200007
Views97See moreThe occurrence of primary lymphomas of the female genital tract is rare. The diagnosis is usually not possible by the cytological examination; a tissue biopsy is necessary. The present paper reports two patients referred to our service with a diagnosis of cervical lymphoma. In one of them, the diagnostic difficulties are demonstrated. Both patients were submitted to chemotherapy with satisfactory post-operatory period. There is no standard treatment for uterine lymphomas. Exclusive local treatment is supported by some reports in the literature in clinical stage IE, while others prefer systemic treatment irrespective of clinical stage.
-
Original Article03-19-2006
Value of magnetic resonance imaging in prenatal diagnosis of placental accretism
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(12):700-707
Abstract
Original ArticleValue of magnetic resonance imaging in prenatal diagnosis of placental accretism
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(12):700-707
DOI 10.1590/S0100-72032006001200003
Views73See morePURPOSE: to establish the main signs of placental accretism in magnetic resonance imaging (MRI) in patients with clinical suspicion and to estimate the benefit of this method. METHODS: prospective transversal study with 15 patients suspected of placental accretism, referred between March 2003 and February 2006. Gestational age varied from 20 to 31 weeks. All patients underwent MRI to study the placenta and had previously done an ultrasonography. Material was sent to histological study. MRI was done on Magnetom Impact and Sonata Maestro Class Siemens®, with acquired sequences HASTE, TURBO SPIN in axial, sagittal, coronal planes and echo gradient (GE®), pre- and post-dynamic contrast in the best plan for acquisition. Images were analyzed by a team of two radiologists. RESULTS: mean gestational age was 24.3 weeks. We studied seven placenta previa (47%), six anterior placentas (40%) and two posterior placentas (13%). Ultrasonography was positive in 80% of the palcentas and MRI in 53%. However, echography had a low concordance with anatomic pathological studies by Kappa test (11%), revealing 75% of sensitivity, 14% of specificity, 50% as positive predictive value (PPV) and 33% as negative predictive value (NPV). MRI had an excellent concordance with anatomic pathological studies (0.86), showing 100% of sensitivity, 86% of specificity, 89% as PPV and 100% as NPV. CONCLUSIONS: MRI is useful for placental accretism diagnosis. The principal findings are transmural hyper-signal, the loss of continuity in myometrial wall in fast sequences and the identification of vessels invading myometrial layer in dynamic sequences.
-
Original Article12-06-2006
Prenatal diagnosis of conjoined twins by magnetic resonance imaging: report of two cases
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(7):416-423
Abstract
Original ArticlePrenatal diagnosis of conjoined twins by magnetic resonance imaging: report of two cases
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(7):416-423
DOI 10.1590/S0100-72032006000700007
Views110Conjoined twins have a rare prevalence and special curiosity among physicians and the general population. The reported frequency varies from 1:50,000 to 1:200,000 pregnancies. Its early diagnosis becomes very important when we think about pregnancy management, method of delivery and neonatal care. We describe two cases of conjoined twins diagnosed by ultrasound and magnetic resonance during prenatal care with the aim to better studying the fetus anatomy. The first conjoined twins were cephalopagus sharing head, thorax and abdominal wall and with two pelvis and four arms and four legs. The second were thoracopagus, united by thorax and part of abdomen. Magnetic resonance imaging contribution was not important to diagnose conjoined twins. However, it was useful to describe the shared organs, contributing to define fetal outcome.
Key-words Case reportsMagnetic resonance Imagingprenatalprenatal diagnosisTwinsTwins, conjoinedUltrasonographySee more -
Original Article08-16-2006
Uterine arteriovenous malformation after gestational trophoblastic disease
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(2):112-121
Abstract
Original ArticleUterine arteriovenous malformation after gestational trophoblastic disease
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(2):112-121
DOI 10.1590/S0100-72032006000200007
Views82PURPOSE: to investigate the presence and outcome of uterinevascular malformations (UVAM) after gestational trophoblastic disease (GTD). METHODS: retrospective study of 2764 patients with GTD diagnosed from 1987 to 2004. All patients were followed up annually at the "Santa Casa da Misericórdia" Trophoblastic Disease Center (Rio de Janeiro, RJ, Brazil) with transvaginal ultrasonography (US) and color Doppler imaging. Seven patients had a final diagnosis of UVAM based on ultrasonographic analysis - pulsatility index (PI), resistance index (RI), peak systolic velocity (PSV) - and pelvic magnetic nuclear resonance (MNR) findings. Negative beta-hCG values were of utmost importance to establish differential diagnosis with persistent GTD. RESULTS: the incidence of UVAM after GTD was 0.2% (7/2764). US features of UVAM: PI mean 0.44±0,058 (extremes: 0.38-0.52); RI mean 0.36±0.072 (extremes: 0.29-0.50); PSV mean 64.6±23.99 cm/s (extremes: 37-96). MNR image showed a bulky uterus, myometrial inhomogeneity, serpiginous flow-related signal voids, and prominent parametrial vessels. The most common UVAM clinical presentation was vaginal hemorrhage, present in 52.7% (4/7). Pharmacological management with 150 mg medroxyprogesterone acetate was employed to control bleeding, after hemodynamic stabilization. These patients are still being followed and remain asymptomatic nowadays. Two patients with persistent UVAM became pregnant and had successful outcomes. CONCLUSION: patients with antecedent of GTD presenting transvaginal bleeding and negative beta-hCG may be considered to have UVAM and should be investigated through US with Doppler velocimetry. Conservative management is a valuable option in many of the acquired UVAM after GTD.
Key-words Arteriovenous malformationsMagnetic resonance ImagingPregnancy complicationsTrophoblastic neoplasmsUltrasonography, dopplerSee more -
Case Report04-13-2005
Congenital cytomegalovirus infection: a case report
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(12):750-758
Abstract
Case ReportCongenital cytomegalovirus infection: a case report
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(12):750-758
DOI 10.1590/S0100-72032005001200008
Views111Congenital cytomegalovirus infection is an important clinical entity, due to its sonographic symptomatology. In Brazil, in utero diagnosis is not accomplished despite the improvements in diagnostic methods. We report a congenital infection including: splenomegaly and hepatomegaly, hypoplasia of the cerebellar vermis, intracranial calcifications, hyperechoic kidneys, hyperechoic bowel, cardiomegaly, lung hypoplasia, ascites, and pericardial effusion. Fetal magnetic resonance imaging confirmed the sonographic findings. Amniocentesis was performed for cytomegalovirus PCR in amniotic fluid, which confirmed fetal infection. Fetal loss occurred in the 31st week of pregnancy. Necropsy studies confirmed the sonographic findings. The diagnostic methods have been useful to confirm congenital cytomegalovirus infection and to establish fetal outcome.
Key-words CytomegalovirusCytomegalovirus infectionsMagnetic resonance Imagingprenatal diagnosisUltrasonographySee more


