-
Review Article
Combined Oral Contraceptive Use and the Risk of Cervical Cancer: Literature Review
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):818-823
01-11-2023
Summary
Review ArticleCombined Oral Contraceptive Use and the Risk of Cervical Cancer: Literature Review
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(12):818-823
01-11-2023Views225See moreAbstract
Cervical cancer (CC) is caused by persistent infection of human papillomavirus of high oncogenic risk (hr-HPV); however, several cofactors are important in its carcinogenesis, such as smoking, multiparity, and prolonged use of oral hormonal contraceptives (COCs). Worldwide, 16% of women use COCs, whereas in Brazil this rate is of ~ 30%. The safety and adverse effects of COCs are widely discussed in the literature, including the increase in carcinogenic risk. Due to the existence of several drugs, combinations, and dosages of COCs, it is hard to have uniform information in epidemiological studies. Our objective was to perform a narrative review on the role of COCs use in the carcinogenesis of cervical cancer. Several populational studies have suggested an increase in the incidence of cervical cancer for those who have used COCs for > 5 years, but other available studies reach controversial and contradictory results regarding the action of COCs in the development of CC.
-
Original Article
Association of Swede Score and 2011 IFCPC Nomenclature in Women with Abnormal Cytology
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(10):938-944
01-23-2022
Summary
Original ArticleAssociation of Swede Score and 2011 IFCPC Nomenclature in Women with Abnormal Cytology
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(10):938-944
01-23-2022Views85See moreAbstract
Objective
To assess the association between two colposcopic indices, the Swede score and the 2011 International Federation of Cervical Pathology and Colposcopy (IFCPC) Nomenclature as well as to determine the efficacy of the Swede score with cutoffs of 7 and 8.
Methods
In the present cross-sectional pilot study, 34 women who had at least 1 colposcopy-directed biopsy due to abnormal cytology were enrolled. The colposcopic findings were scored by both the Swede score and the 2011 IFCPC Nomenclature and were compared with each other. The Kappa coefficient and the McNemar test were used. Accuracy, sensitivity, specificity, and positive and negative predictive values (NPV and PPV, respectively) were calculated, as well as the effectiveness with cutoffs of 7 and 8 in identifying cervical intraepithelial neoplasm (CIN) 2+ when using the Swede score.
Results
The correlation between the 2 colposcopic indices was 79.41%. The Kappa coefficient and the McNemar p-value were 0.55 and 0.37, respectively. The IFCPC Nomenclature had sensitivity, specificity, accuracy, PPV, and NPV of 85.71, 55.00, 67.64, 57.14, and 84.61%, respectively. The Swede score had sensitivity, specificity, accuracy, PPV, and NPV of 100, 63.15, 79.41, 68.18, and 100%, respectively. A Swede score cutoff of 7 for CIN 2+ detection had a specificity of 94.73%, while with a cutoff of 8 it increased to 100%. The sensitivity for both values was 60%. The PPV and NPV for cutoffs of 7 and 8 were 90 and 75 and 100 and 76%, respectively.
Conclusion
Although both colposcopic indices have good reproducibility, the Swede score showed greater accuracy, sensitivity, and specificity in identifying CIN 2 + , especially when using a cutoff of 8.
-
Original Article
Estimation of the Costs of Invasive Cervical Cancer Treatment in Brazil: A Micro-Costing Study
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(6):387-393
07-22-2019
Summary
Original ArticleEstimation of the Costs of Invasive Cervical Cancer Treatment in Brazil: A Micro-Costing Study
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(6):387-393
07-22-2019Views114See moreAbstract
Objective
Themain objective of the present study was to estimate the annual treatment costs of invasive cervical cancer (ICC) per patient at an oncology center in Brazil from a societal perspective by considering direct medical, direct nonmedical, and indirect costs.
Methods
A cost analysis descriptive study, in which direct medical, direct nonmedical, and indirect costs were collected using a microcosting approach, was conducted between May 2014 and July 2016 from a societal perspective. The study population consisted of women diagnosed with ICC admitted to a tertiary hospital in Recife, state of Pernambuco, Brazil. The annual cost per patient was estimated in terms of the value of American Dollars (US$) in 2016.
Results
From a societal perspective, the annual ICC treatment cost per patient was US $ 2,219.73. Direct medical costs were responsible for 81.2% of the total value, of which radiotherapy and outpatient chemotherapy had the largest share. Under the base-case assumption, the estimated cost to the national budget of a year of ICC treatment in the Brazilian population was US$ 25,954,195.04.
Conclusion
We found a high economic impact of health care systems treating ICC in a poor region of Brazil. These estimates could be applicable to further evaluations of the cost-effectiveness of preventing and treating ICC.
-
Original Article
Association between Hormonal Contraception and Injuries Induced by Human Papillomavirus in the Uterine Cervix
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):196-202
04-01-2018
Summary
Original ArticleAssociation between Hormonal Contraception and Injuries Induced by Human Papillomavirus in the Uterine Cervix
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(4):196-202
04-01-2018Views104See moreAbstract
Objective
To evaluate the association between hormonal contraception and the appearance of human papillomavirus HPV-induced lesions in the uterine cervix of patients assisted at a school outpatient clinic - ObGyn outpatient service of the Universidade do Sul de Santa Catarina.
Methods
A case-control study, with women in fertile age, performed between 2012 and 2015. A total of 101 patients with cervical lesions secondary to HPV were included in the case group, and 101 patients with normal oncotic colpocytology, in the control group. The data were analyzed through the Statistical Package for the Social Sciences (SPSS, IBM Corp. Armonk, NY, US) software, version 24.0, using the 95% confidence interval. To test the homogeneity of the proportions, the chi-square (χ2) test was used for the qualitative variables, and the Student t-test, for the quantitative variables.
Results
When comparing the occurrence of HPV lesions in users and non-users of combined oral contraceptives (COCs), the association with doses of 0.03 mg or higher of ethinylestradiol (EE) was observed. Thus, a higher probability of developing cervical lesions induced by HPV was identified (odds ratio [OR]: 1.9 p = 0.039); and when these cases were separated by the degree of the lesion, the probability of these patients presentingwith lowgrade squamous intraepithelial lesion was 2.1 times higher (p = 0.036), but with no impact on high-grade squamous intraepithelial lesions and the occurrence of invasive cancer. No significant differences were found in the other variables analyzed.
Conclusion
Although the results found in the present study suggest a higher probability of the users of combined hormonal contraceptives with a concentration higher than 0.03 mg of EE to develop low-grade intraepithelial lesions, more studies are needed to conclude causality.
-
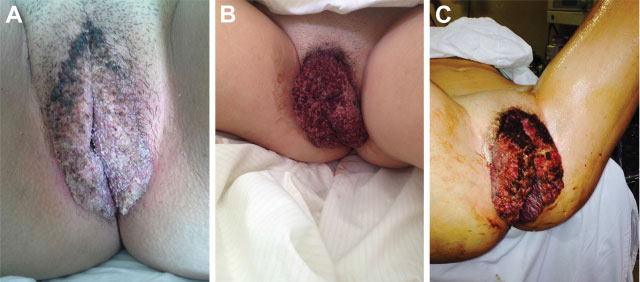
Case Report
Giant Condyloma (Buschke-Loewenstein Tumor) in a 16-year-old Patient: Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):471-476
09-01-2016
Summary
Case ReportGiant Condyloma (Buschke-Loewenstein Tumor) in a 16-year-old Patient: Case Report
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(9):471-476
09-01-2016Views153See moreAbstract
The Buschke-Loewenstein tumor is characterized by excessive growth of verrucous lesions on the genitals and/or perianal region. It is considered benign despite the high rate of recurrence and the possibility of malignant transformation. It is commonly associated with subtypes 6 and 11 of the human papillomavirus (HPV), and host 's immunity plays an important role in the development of the disease. Surgical excision is the recommended treatment in most cases. We present the case of a 16 years old female patient with extensive vulvar lesions successfully treated surgically.
-
Original Articles
High Risk HPV E6/E7 Oncoprotein Expression in Women with High Grade Squamous Intraepithelial Lesion
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(3):154-159
03-01-2016
Summary
Original ArticlesHigh Risk HPV E6/E7 Oncoprotein Expression in Women with High Grade Squamous Intraepithelial Lesion
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(3):154-159
03-01-2016Views175See morePurpose
To correlate the expression of high-risk HPV E6 mRNA with pap smear, colposcopy, and biopsy results in women with high grade squamous intraepithelial lesion (HSIL).
Methods
A cross-sectional study was performed on women referred for primary care services after cytological diagnosis of HSIL. We evaluated the expression of E6/E7 mRNA of HPV types 16,18,31,33, and 45 and correlated the results with those of Pap smear, colposcopy, and biopsy. For amplification/detection of mRNA E6 / E7 we used NucliSENSEasyQ kit to detect HPV mRNA by polymerase chain reaction with primers/ probes for HPV types 16, 18, 31, 33, and 45.
Results
Out of 128 valid tests, the results of 30 (23.4%) tests were negative and 98 (70%) tests were positive. Only one type of HPV was detected in 87.7% of the E6/E7 mRNA positive cases. HPV16 was detected in 61.2% of the cases, followed by HPV33 (26.5%), HPV31 (17.3%), HPV18 (10%), and HPV45 (4.08%). Pap smear tests revealed that the E6/E7 test was positive in 107 (83.8%) women with atypical squamous cells - high grade (ASC-H), HSIL, or higher. The E6/E7 test was positive in 69 (57.5%) specimens presenting negative cytology results. When analyzing the association with colposcopy results, the frequency of positive E6/E7 results increased with the severity of the injury, ranging from 57.1% in women without colposcopy-detected injury to 86.5% in those with higher levels of colposcopy findings. Of the 111 women who underwent biopsy and E6/E7 testing, the E6/E7 test was positive in 84.7% of the women who presented with lesions of cervical intraepithelial neoplasia (CIN) grade 2 or higher. Finally, 41.2% of women with a negative biopsy presented a positive E6/E7 test.
Conclusions
E6/E7mRNA expression was higher in women with HSIL and CIN grade 2 or higher.
-
Original Articles
Predictive Capability of HPV and Pap Tests in Screening for Cervical Cancer over a Three-Year Follow-up
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(3):147-153
03-01-2016
Summary
Original ArticlesPredictive Capability of HPV and Pap Tests in Screening for Cervical Cancer over a Three-Year Follow-up
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(3):147-153
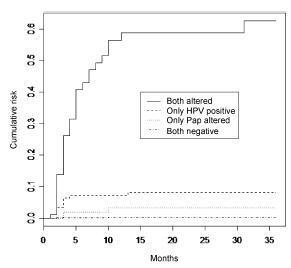
03-01-2016Views93See morePurpose
To compare the predictive capability of HPV and Pap smear tests for screening pre-cancerous lesions of the cervix over a three-year follow-up, in a population of users of the Brazilian National Health System (SUS).
Methods
This is a retrospective cohort study of 2,032 women with satisfactory results for Pap smear and HPV tests using second-generation hybrid capture,made in a previous study. We followed them for 36 months with data obtained from medical records, the Cervix Cancer Information System (SISCOLO), and the Mortality Information System (SIM). The outcome was a histological diagnosis of cervical intraepithelial neoplasia grade 2 or more advanced lesions (CIN2ş). We constructed progression curves of the baseline test results for the period, using the Kaplan-Meier method, and estimated sensitivity, specificity, positive and negative predictive value, and positive and negative likelihood ratios for each test.
Results
A total of 1,440 women had at least one test during follow-up. Progression curves of the baseline test results indicated differences in capability to detect CIN2ş (p < 0.001) with significantly greater capability when both tests were abnormal, followed by only a positive HPV test. The HPV test was more sensitive than the Pap smear (88.7% and 73.6%, respectively; p < 0.05) and had a better negative likelihood ratio (0.13 and 0.30, respectively). Specificity and positive likelihood ratio of the tests were similar.
Conclusions
These findings corroborate the importance of HPV test as a primary cervical cancer screening.
-
Original Articles
Expression of the Immunohistochemical Markers p16 and Ki-67 and Their Usefulness in the Diagnosis of Cervical Intraepithelial Neoplasms
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(2):82-87
02-01-2016
Summary
Original ArticlesExpression of the Immunohistochemical Markers p16 and Ki-67 and Their Usefulness in the Diagnosis of Cervical Intraepithelial Neoplasms
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(2):82-87
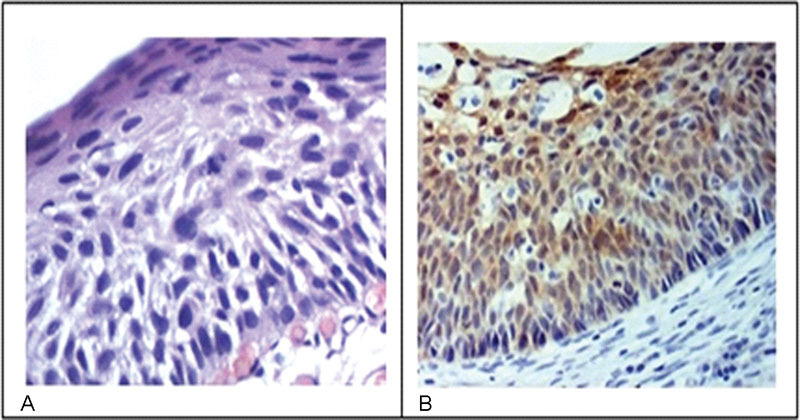
02-01-2016Views110See moreObjective
The aim of this study was to determine the expression of the immunohistochemical markers p16 and Ki-67 in cervical intraepithelial neoplasms and their influence on the level of agreement among different observers and for the same observer.
Methods
The study included 184 patients with cervical intraepithelial neoplasms previously confirmed through biopsies performed between 2005 and 2006. Three pathologists reviewed the biopsies by using hematoxylin-eosin staining to reach a consensus on the diagnosis. Subsequently, an immunohistochemical study analyzed the expression of p16 and Ki-67 in such cases.
Results
The comparison among the reviewing pathologists revealed only moderate agreement (kappa = 0.44). The agreement improved when the differentiation of highgrade lesions (cervical intraepithelial neoplasm - CIN - 3) was analyzed (kappa = 0.59). p16 staining exhibited a high negative predictive value and sensitivity; however, the specificity was low. Overall, both qualitative and quantitative analyses of p16 and a quantitative analysis Ki-67 exhibited low accuracy. The agreement among diagnoses before immunohistochemistry was 0.47. The use of immunohistochemistry increased the agreement to 0.68.
Conclusion
Our study showed that the agreement among observers using traditional diagnostic criteria of cervical intraepithelial lesions can improve with the use of immunohistochemistry.