Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2007;29(7):358-365
DOI 10.1590/S0100-72032007000700006
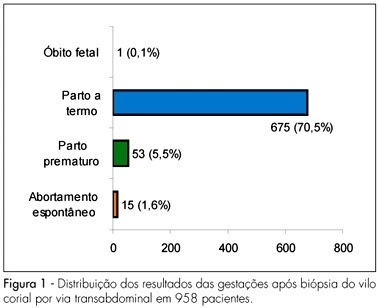
PURPOSE: to evaluate fetal maternal complications after chorionic villus sampling (CVS) for prenatal diagnosis of genetic disorders in pregnant women of Salvador (BA), Brazil. METHODS: case-series study of 958 pregnancies with high risk for chromosomal abnormality submitted to CVS transabdominal between the ninth to the 24th week of gestation, using an ultrasound-guided 18G 3½ spinal needle, from 1990 to 2006. The variables for the analysis of immediate complications were uterine cramps, subchorionic hematoma, accidental amniotic cavity punction, pain in the punction area, amniotic fluid leakage, abdominal discomfort, fetal arrhythmias and vaginal bleeding, and of late complication, abdominal pain, vaginal bleeding, amniotic fluid leakage, infection and spontaneous miscarriage. Premature labor, obstetrical complications (abruption placenta and placenta previa) and newborn malformation were also studied. Qui-square, Student’s "t" or Mann-Whitney tests were used for the statistical analysis; the significance level was 5%. RESULTS: maternal mean age was 36.3±4.9 years old. Immediate complications ware found in 182 (19%) cases (uterine cramp in 14%, subchorionic hematoma in 1.8% and accidental amniotic cavity punction in 1.3%). Late complications were found in 32 (3.3%) cases (vaginal bleeding in 1.6%, abdominal pain in 1.4%, amniotic fluid leakage in 0.3% and spontaneous miscarriage in 1.6% cases). There was no case of abruption placentae, placenta previa or fetal malformation. CONCLUSIONS: CVS is a simple and safe procedure. CVS should be performed in high risk pregnant patients who need prenatal diagnosis of fetal chromosomal abnormalities.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(9):525-531
DOI 10.1590/S0100-72031998000900006
Purpose: to calculate sensitivity, specificity and positive and negative predictive values for multiparameter ultrasound scores for Down's syndrome. Patients and Methods: sensitivity and specificity for Down syndrome were calculated for ultrasound scores in a prospective study of ultrasound signs from 16 to 24 weeks in a high-risk population who denied invasive procedures after genetic counselling. The signs and scores were: femur/foot length < 0,9 (1), nuchal fold > 5 mm (2), pyelocaliceal diameter > 5 mm (1), nasal bones < 6 mm (1), absent or hypoplastic fifth median phalanx (1) and major structural malformations (2). Complete follow-up was obtained in each case. Genetic amniocentesis was proposed in the case of score 2 or more. Results: a total of 963 patients were examined from October 93 to December 97 at a mean gestational age of 19.6 (range 16 -24) weeks. Women's age ranged from 35 to 47 years (mean 38.8) and 18 Down syndrome cases were observed (1.8%). Sensitivity was 94.5% (17/18) for score 1 and 73% (13/18) for score 2 (false positive rate of 9.8% for score 1 and 4.1% for score 2). Individual sign sensitivity and specificity were: femur/foot = 16.7% (3/18) and 96.8% (915/945); nasal bones = 22.2% (4/18) and 92.1% (870/945); nuchal fold = 44.4% (8/18) and 96.5% (912/945); pyelic diameter = 38.9% (7/18) and 94.3% (891/945); absent phalanx = 22.2% (4/18) and 98.5% (912/945); malformation = 22.2% (4/18) and 98.2% (928/945). Conclusions: the overall sensitivity for score 1 was high but false positive rates were also high. For score 2, sensibility was still good (73%) and false positive rate was acceptable (4.1%). Positive and negative predictive values can be calculated for each prevalence (women's age). More cases are needed to reach final conclusions about this screening method (specially in a low-risk population) although this system has been useful for high-risk patients who deny invasive procedures.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(3):151-157
DOI 10.1590/S0100-72032006000300003
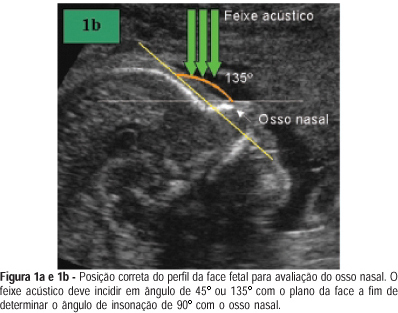
PURPOSE: the absence of fetal nasal bone is correlated with trisomy 21. Although a hypoplastic nasal bone is also correlated with trisomy 21, there is no clear definition of this term in the literature. Our objective was to establish the reference values for fetal nasal bone size throughout gestation in a local population in Brazil. METHODS: it is a cross-sectional study on 902 fetuses at 10 to 39 weeks of gestation. After having excluded fetal malformations and maternal diseases which are known to interfere with fetal growth, 625 fetuses were selected. We obtained a mid-sagittal view of the fetal profile by holding the ultrasound bean at an angle of 45º or 135º. The nasal bone size mean was calculated by using polynomial regression. The Anderson-Darling test proved the normal distribution of the measurements (p>0.05). RESULTS: of the 625 fetuses, 88.3% were from single gestations and 11.7% from multiple ones. There was a direct correlation between fetal nasal bone size and gestational age. The variability of nasal bone size became larger as gestational age increased. Minimal length of 1.0 and 4.7 mm in the first and second trimesters, respectively, were found. CONCLUSIONS: there is a direct correlation between fetal nasal bone size and gestational age. This correlation is valid either for a single gestation or a multiple one. These measurements of the fetal nasal bone will allow us to use them as a screening test for cromosomal abnormalities. This is a useful study if we consider the large miscegenation of the Brazilian population. However, further systematic and standardized approach to study the fetal nasal bone is needed to establish its real value in fetuses once classified as at high or low risk for aneuploidies.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(9):601-608
DOI 10.1590/S0100-72032002000900006
Purpose: to appraise the value of ultrasonographic parameters for the diagnosis of fetal Down syndrome (T21), in order to permit its use in routine clinical practice. Methods: this is a prospective cohort study using various ultrasonographic parameters for the prediction of T21. A total of 1662 scans were evaluated in the cohort study and 289 examinations were analyzed as a differential sample to test the normality curve from October 1993 to November 2000. The statistical analysis was based on the calculation of intra- and interobserver variations, the construction of normality curves for the studied parameters, as well as their validity tests, and the calculation of sensitivity, specificity, relative risk, likelyhood ratio and posttest predictive values. Results: among 1662 cases, 22 fetuses (1.32%) with T21 were identified. The normality curves were built for nucal fold thickness, femur/foot ratio and nasal bone length. Renal pelvis had a semiquantitative distribution and the proposed cutoff level was 4.0 mm. Sensitivity, specificity, false positive rate, relative risk and likelyhood ratio for nucal fold measurements above the 95th percentile were 54.5%, 95.2%, 4.9%, 20.2 and 11, respectively. For nasal bone measurements below the 5th percentile, 59.0%, 90.1%, 9.0%, 13.4 and 6.5. For femur/foot ratio below the 5th percentile, 45.5%, 84.4%, 15.6%, 3.7 and 2,6. For renal pelvis greater than 4.0 mm, 36.4%, 89.2%, 10.9%, 4.5 and 3.4. For absent fifth finger middle phalanx, 22.7%, 98.1%, 1.9%, 13.2 and 11.9. For the presence of major malformations, 31.8%, 98.7%, 1.3%, 27.2 and 24,8. After calculating the probability rates and the incidence of T21 in different maternal ages, a table for posttest risk using ultrasonographic parameters was set up. Conclusions: normality curves and indices for the assessment of risk for fetal Down syndrome on a population basis were established by the utilization of different maternal ages and by multiplying factors proposed by the authors. It was not possible to establish a normality curve for renal pelvis measurements, because of their semiquantitative distribution.