Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2016;38(3):154-159
To correlate the expression of high-risk HPV E6 mRNA with pap smear, colposcopy, and biopsy results in women with high grade squamous intraepithelial lesion (HSIL).
A cross-sectional study was performed on women referred for primary care services after cytological diagnosis of HSIL. We evaluated the expression of E6/E7 mRNA of HPV types 16,18,31,33, and 45 and correlated the results with those of Pap smear, colposcopy, and biopsy. For amplification/detection of mRNA E6 / E7 we used NucliSENSEasyQ kit to detect HPV mRNA by polymerase chain reaction with primers/ probes for HPV types 16, 18, 31, 33, and 45.
Out of 128 valid tests, the results of 30 (23.4%) tests were negative and 98 (70%) tests were positive. Only one type of HPV was detected in 87.7% of the E6/E7 mRNA positive cases. HPV16 was detected in 61.2% of the cases, followed by HPV33 (26.5%), HPV31 (17.3%), HPV18 (10%), and HPV45 (4.08%). Pap smear tests revealed that the E6/E7 test was positive in 107 (83.8%) women with atypical squamous cells - high grade (ASC-H), HSIL, or higher. The E6/E7 test was positive in 69 (57.5%) specimens presenting negative cytology results. When analyzing the association with colposcopy results, the frequency of positive E6/E7 results increased with the severity of the injury, ranging from 57.1% in women without colposcopy-detected injury to 86.5% in those with higher levels of colposcopy findings. Of the 111 women who underwent biopsy and E6/E7 testing, the E6/E7 test was positive in 84.7% of the women who presented with lesions of cervical intraepithelial neoplasia (CIN) grade 2 or higher. Finally, 41.2% of women with a negative biopsy presented a positive E6/E7 test.
E6/E7mRNA expression was higher in women with HSIL and CIN grade 2 or higher.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(8):381-387
DOI 10.1590/SO100-720320150005393
To evaluate the waiting times before obtaining the first colposcopic examination for women with abnormal Papanicolaou smears.
Retrospective cohort study conducted on patients who required a colposcopic examination to clarify an abnormal pap test, between 2002 January and 2008 August, in a metropolitan region of Brazil. The waiting times were defined as: Total Waiting Time (interval between the date of the pap test result and the date of the first colposcopic examination); Partial A Waiting Time (interval between the date of the pap test result and the date of referral); Partial B Waiting Time (interval between the date of referral and the date of the first colposcopic examination). Means, medians, relative and absolute frequencies were calculated. The Kruskal-Wallis test and Pearson's chi-square test were used to determine statistical significance.
A total of 1,544 women with mean of age of 34 years (SD=12.6 years) were analyzed. Most of them had access to colposcopic examination within 30 days (65.8%) or 60 days (92.8%) from referral. Mean Total Waiting Time, Partial A Waiting Time, and Partial B Waiting Time were 94.5 days (SD=96.8 days), 67.8 days (SD=95.3 days) and 29.2 days (SD=35.1 days), respectively.
A large part of the women studied had access to colposcopic examination within 60 days after referral, but Total waiting time was long. Measures to reduce the waiting time for obtaining the first colposcopic examination can help to improve the quality of care in the context of cervical cancer control in the region, and ought to be addressed at the phase between the date of the pap test results and the date of referral to the teaching hospital.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2012;34(6):248-253
DOI 10.1590/S0100-72032012000600002
PURPOSE: To verify whether women with atypias of undetermined significance and precursor lesions or invasive cervical outcomes were referred to Medium Complexity Units (MCU) following the guidelines recommended by the Brazilian Ministry of Health. METHODS: Retrospective study based on the cytopathological outcomes of users of the Unified Health System, seen at Basic Health Assistance Units (BHAU) and referred to MCUs in the municipality of Goiânia, state of Goiás, from 2005 to 2006. We assessed 832 records according to the recommendations of the Brazilian Ministry of Health, as established by the Brazilian Nomenclature for Cervical Cytopathologic Outcomes and Recommended Clinical Practice. To check the distribution of variables such as reasons for referral, results of colposcopy and histopathology and clinical procedures we calculated absolute and relative frequencies, mean, minimum and maximum values. RESULTS: We understood 72.7% of the referrals were not in accordance with the recommendations of the Ministry of Health. There were 605 women with test results classified as atypical squamous cells of undetermined significance, possibly non-neoplasms, and squamous intraepithelial lesion of low level which were sent to MCU, and of these 71.8% were submitted to colposcopy, and 64.7% had histopathological examination which results were classified as 31.0% with non-neoplasms and 44.6% as NIC I. Out of 211 women with results classified as more severe squamous lesions, 86.3% were submitted to colposcopy and 68.7% of these had histopathological examinations. CONCLUSIONS: The results of this study revealed high rates of inappropriate referrals to MCU, which required a high percentage of unnecessary procedures. The recommendations of the Ministry of Health were followed by BHAU and the majority of women received counseling/treatment as recommended.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(8):368-373
DOI 10.1590/S0100-72032010000800002
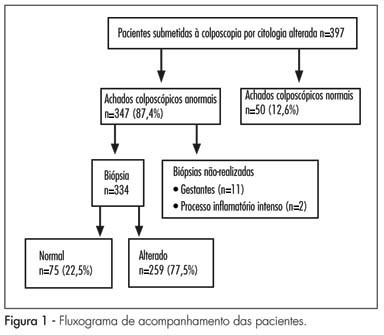
PURPOSE: to evaluate the agreement between conventional cytology using the Papanicolaou test, repeated at the time of colposcopy, with colposcopic and histopathological findings. METHODS: the study was carried out at the central public health laboratory of the state of Pernambuco between January and July, 2008, involving 397 women referred for colposcopic evaluation following an abnormal cervical smear test. Cytology was repeated at the time of colposcopy using conventional method, with particular attention being paid to the presence of abnormal colposcopic findings. The nomenclature used for cytology was the 2001 Bethesda system terminology, while that used for histology was the World Health Organization 1994 classification. Cytology performed at the time of colposcopy was compared with colposcopy and with histopathology obtained by colposcopy-directed biopsy. The Kappa coefficient was used to evaluate the agreement between methods, as well as the χ2 test, with the level of significance set at 5%. RESULTS: poor agreement was found between cytology performed at the time of colposcopy and colposcopic findings (K=0.33; 95%CI=0.21-0.45) and between colposcopy and histopathology (K=0.35; 95%CI=0.39-0.51). Cytology performed at the time of colposcopy compared with histopathology revealed a Kappa of 0.41 (95%CI=0.29-0.530), which was considered to reflect moderate agreement. CONCLUSIONS: agreement was better between cytology and histopathology than between colposcopy and cytology or between colposcopy and histopathology.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(12):604-608
DOI 10.1590/S0100-72032009001200005
PURPOSE: to evaluate the results of treatment to which patients with high grade intraepithelial cervical neoplasia (HSIL) are submitted, as well as their follow-up during pregnancy. METHODS: retrospective study based on the review of the medical report of 30 patients with diagnosis of high-grade squamous intraepithelial lesions (HSIL) during pregnancy and attended to at a tertiary hospital in southern Brazil from 1990 to 2002. Diagnosis was performed by colposcopy and biopsy, with repetition of the colposcopy during the pregnancy and after delivery. The diagnoses of regression and progression of lesions were evaluated. RESULTS: from 30 patients, 3 were excluded of the sample because the diagnosis of high-grade squamous intraepithelial lesions (HSIL) was not confirmed by the colposcopy with biopsia. Four patients were submitted to treatment during pregnancy, and one of them presented preterm delivery at the 32nd week. Twenty-three patients were submitted to expectant treatment, underwent a new colposcopy and biopsy, and then were submitted to conisation surgery at about the 11th week after the end of pregnancy. In 7.4% of the cases, there was lesion regression in the surgical specimen. CONCLUSIONS: all patients with diagnosis should be submitted to colposcopy and biopsy to exclude the possibility of invasive lesion. The expectant procedure for intraepithelial lesions is the most widely chosen and safe due to the possibility of regression in the postpartum period.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(11):573-582
DOI 10.1590/S0100-72032008001100008
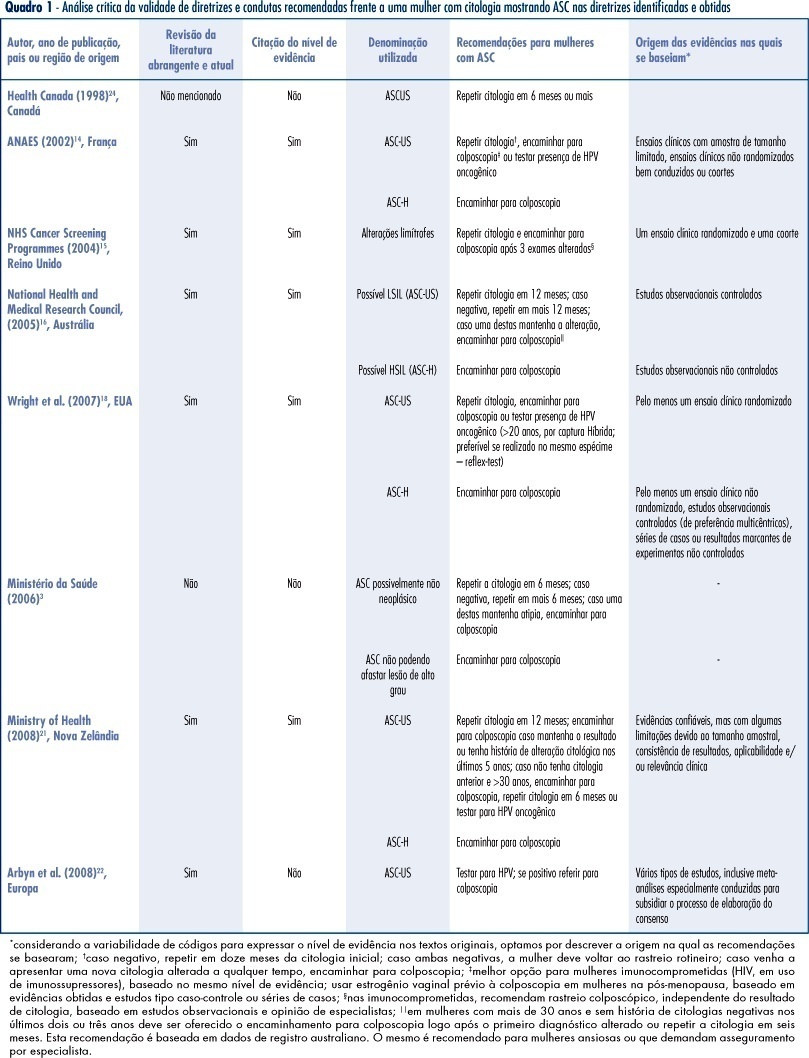
PURPOSE: to identify valid guidelines for the approach of women with cytopathological diagnosis of undetermined significance atypias in squamous cells (ASC), discussing its applicability to the Brazilian scenario. METHODS: an electronic search of publications at PubMed, National Guidelines Clearinghouse and Scholar Google was carried out, as well as a manual search of references from the texts found. The guidelines identified, and specifically related to the theme, were evaluated according to its validity and the recommendations were criticized and summarized. RESULTS: guidelines for the United Kingdom, France, Australia, the USA and New Zealand have been considered as valid. These documents recommend repeating the cytology in six or twelve months, in ASCs of undetermined significance (ASC-US) before referring to colposcopy, and immediate referral to colposcopy in ASCs, when it is not possible to disregard high degree lesions (ASC-H). We have also found valid colposcopy recommendations for women with ASC-US in special situations (immune deficient women requiring specialist assistance) and the use of oncogenic HPV test, which, when present in women over 20, should motivate referral to colposcopy. CONCLUSIONS: the clinical guidelines recommended for the Programa Nacional de Controle do Cancer do Colo do Útero in Brazil can be improved with the referral to colposcopy in special situations (immune deficient women requiring specialist assistance), the use of test for the detection of oncogenic HPV in women over 20 (when present, refer to colposcopy), the investigation of vaginal lesions, the use of estrogens before the colposcopy in post-menopausal women, and disregard biopsia in case of slighter alterations.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1998;20(1):50-52
DOI 10.1590/S0100-72031998000100009
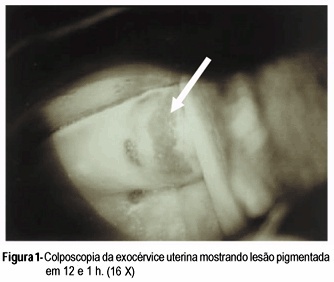
Compound nevus of the uterine cervix is very rare. Benign and malignant melanotic lesions of endo and exocervix have been rarely documented. The present case of compound nevus in the uterine exocervix was found in a 47-year-old woman without gynecologic complaints. Diagnosis was suspected by colposcopic evaluation and confirmed trough histopathological examination. The treatment was concluded with total abdominal hysterectomy based on the possible malignant transformation of these lesions and the difficult patient follow-up.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 1999;21(4):193-200
DOI 10.1590/S0100-72031999000400003
Purpose: to evaluate the efficacy of cytology and colposcopy-directed biopsy to distinguish preclinical invasive cervical carcinoma from intraepithelial lesions. Patients and Methods: 441 patients submitted to conization, hysterectomy and Wertheim-Meigs operation from 1978 to 1995 in the University Hospital "Clementino Fraga Filho", Federal University of Rio de Janeiro, Cervical Pathology Outpatient Clinic. We estimated sensitivity, specificity, predictive values, likelihood ratio and confidence intervals of each study, which were divided into four classes: 1) normal and inflammatory; 2) mild and moderate dysplasias; 3) severe dysplasia and carcinoma in situ; 4) microcarcinoma and invasive carcinoma. Biopsies were analyzed as a whole and separated in accordance with the type of the colposcopic result (satisfactory and unsatisfactory). Results: cytology has shown sensitivity of 50%, specificity of 89%, positive predictive value of 63% and negative predictive value of 82%. The likelihood ratios were 4.4 for stromal invasion diagnosis, 0.7 for severe dysplasia and carcinoma in situ, 0.1 for mild and moderate dysplasia, 2.2 for normal and inflammatory report and 0.6 for the negative results for invasion as a whole. Satisfactory colposcopic guided biopsy white a visible lesion showed sensitivity of 59%, specificity of 100% positive predictive value of 100% and negative predictive value of 83%. Likelyohood ratios were: tending to infinity for invasion, 0.5 for severe dysplasia and carcinoma in situ, zero for mild and moderate dysplasia, zero for negative and inflammatory and 0.4 for all negative results for invasion.