Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(2):75-80
DOI 10.1590/S0100-72032006000200002
PURPOSE: to determine the prevalence of high-grade squamous intraepithelial lesions (HSIL) and cancer in women with cytological diagnosis of persistent ASCUS (atypical squamous cells of undetermined significance) for 6 months in the last 7 years. We also assessed if age could be a predictive factor for presence of HSIL/cancer in this group. METHODS: we included 215 cases of non-pregnant and HIV-seronegative women with cytological diagnosis of persistent ASCUS (unespecific) with at least 6 months of interval between smears. This cytological diagnosis was compared to histological diagnosis obtained by biopsy (large loop excision of the transformation zone) or cone biopsies, and considered negative when colposcopy was satisfactory without lesions or, when unsatisfactory, no lesion was detected after at least one cytological and colposcopic follow-up. RESULTS: among the 215 cases, 49.3% had negative results (CI 95%: 42.6-55.9). The prevalence of histological confirmed low-grade squamous intraepithelial lesion was 38.6% (CI 95%: 32.1- 45.1) and HSIL was 10.7% (CI 95%: 6.5-14.8). Cases of cancer were found in 1.4% of patients (CI 95%: 0-2.9). We could not find a significant difference between the prevalence of HSIL/cancer according to age group using the cutoff point of 35 years. CONCLUSION: HSIL/cancer prevalence observed in this study has shown the risk of finding this kind of lesions in about 12% of women assisted in our public health system with two cytological diagnosis of ASCUS. A higher probability of HSIL/cancer in the different age groups was not found but this result was limited by our small sample size.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(10):619-626
DOI 10.1590/S0100-72032005001000009
PURPOSE: to evaluate the prevalence of cytologic, colposcopic and histopathologic alterations observed in the uterine cervix of adolescents with suspected cervical neoplasia and to compare it with young adult women. METHODS: a cross-sectional, retrospective study that analyzed 366 medical records of females referred to clarify diagnosis of the suspected cervical neoplasia. The patients had been classified into two groups defined by age. The Adolescent group was composed of 129 females between 13 and 19 years and the Adult group was composed of 237 females between 20 and 24 years. Data were analyzed statistically by the prevalence ratio (PR), respective confidence intervals (CI) at 95% for each variable, chi2 test, or Fisher exact test used to compare proportion. RESULTS: the first sexual intercourse coitarche occurred on average at 15.0 years in the Adolescent group and 16.6 years in the Adult group. The possibility of diagnosis of cytological alterations in the first Papanicolaou smears (PR=2.61; CI 95%: 2.0-3,4), the condition of non-clarified cervical intraepithelial neoplasia (CIN) (PR=1.78; CI 95%: 1.26-2,52), and the colposcopic impressions of low grade (PR=1.42; CI 95%: 1.08-1.86) were statistically significant in the Adolescent group. The histopathologic analysis did not show differences at any grade of CIN. However, two cases of microinvasive carcinoma, one in each group, and three cases of clinical invasive carcinoma in the Adult group were identified. CONCLUSION: our study suggests that cervical cancer is rare among adolescents, but we verified that alterations associated with it occurred even in younger women. The evaluation of cervical intraepithelial neoplasia with the careful application of the same tools used for adult women was appropriate also in adolescence.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(3):135-139
DOI 10.1590/S0100-72032000000300003
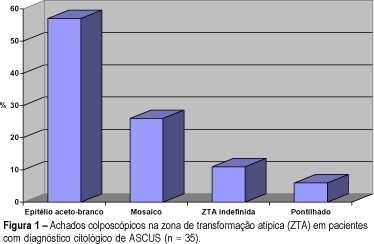
Purpose: to assess clinical, colposcopic profile and follow-up of patients with a cytological report of atypical squamous cells of undetermined significance (ASCUS). Methods: a total of 208 cases of ASCUS diagnosed between 1996 e 1998 were analyzed retrospectively regarding age, symptoms, colposcopy and follow-up. Results: the ASCUS:SIL (squamous intraepithelial lesion) ratio reported was 1:1.2, showing an adequate quality control. Most of the patients were between 15 and 35 years old (72.6 %). The majority referred no symptoms (36.5 %). The colposcopy showed (n = 58) the atypical zone of transformation in 60% of the cases. The subclassification into ASCUS favoring a dysplasia (ASCUS--D), reactive process (ASCUS-R) and unqualified (ASCUS-U) showed that 65% of cases belonged to the first category (ASCUS-D). In the follow-up of 86 patients for 3 to 6 months (average of 4.5 months), 12.5% had a subsequent SIL. Conclusion: the findings of this study indicate that ASCUS occurrence in young women with common symptoms, is frequent and there is the possibility of diagnosing by colposcopy. The follow-up is very important to define the concurrent or subsequent development of a squamous intraepithelial lesion.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(2):65-70
DOI 10.1590/S0100-72032000000200002
Purpose: to evaluate conization by the loop electrosurgical excision procedure (LEEP) for the diagnosis and treatment of cervical intraepithelial neoplasms (CIN), the importance of the margins and follow-up of these women. Methods: 95 women who underwent conization by LEEP for CIN and microinvasive carcinoma from January 1996 to December 1997 were evaluated. For statistical analysis, we used the kappa agreement coefficient and the tendency test of Cochran Armitage. Results: among 63 cases who underwent colposcopically directed biopsy before the conization, the cone presented the same grade of lesion in 20 and no residual disease in 8. The cone lesion presented a higher grade in 24 cases and one of them was a microinvasive carcinoma. Among the 25 women who underwent the cone biopsy with a previous biopsy suggestive of cervicitis or CIN 1, 56% had CIN 2 or 3 in the cone. Among the 32 women without previous biopsy, 15 had CIN 2 or 3, and four had microinvasive carcinoma in the cone. Regarding the margins of the cone, 25 cases presented some grade of CIN in the endocervical margins and 2/10 who underwent a second procedure presented residual disease on histological analysis. Among the 70 women with free cone margins, 2/4 who underwent a second procedure had residual disease on histological analysis. Conclusion: conization by LEEP without previous directed biopsy depends on the experience of the colposcopist. The second resection after LEEP for the diagnosis and treatment of CIN depends not only on the presence of disease in the cone margins but also on the follow-up. A second histological analysis is recommended in cases with microinvasive carcinoma and glandular lesion and affected margins.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2005;27(2):51-57
DOI 10.1590/S0100-72032005000200002
PURPOSE: to estimate the validity of visual inspection of cervical intraepithelial neoplasia (CIN) and HPV-induced lesion screening, after acetic acid application (VIA), and to compare its performance with that of colpocytology and colposcopy. METHODS: a diagnostic test validation study involving 893 women aged 18 to 65 years, simultaneously screened with colpocytology, VIA and colposcopy was carried out at a public health unit in Recife, PE. VIA was performed by applying 5% acetic acid onto the cervix and observing it with the help of a clinical spotlight. The finding of any aceto-white lesion on the cervix was considered positive. The gold standard was the histopathology of cervical biopsy, carried out whenever any of the three test results was abnormal. Validity indicators were estimated for each test, within 95% confidence intervals. The analysis of agreement between test results was done by the kappa coefficient. RESULTS: of 303 women submitted to biopsy, the histopathological study was abnormal in 24. Among this total, VIA was positive in 22, yielding an estimated 91.7% sensibility, 68.9% specificity, and 7.5% positive predictive value and 99.7% negative predictive value. Comparing 95% confidence intervals, VIA was more sensitive than colpocytology, despite a lower specificity and positive predictive value. There was poor agreement between VIA and colpocytology (k=0.02) and excellent agreement with colposcopy (k=0.93). CONCLUSION: VIA was much more sensitive than colpocytology in the screening of CIN and HPV-induced lesions and presented a performance similar to colposcopy. Its low specificity determined a high number of false-positive results.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2004;26(3):213-219
DOI 10.1590/S0100-72032004000300007
OBJECTIVE: to evaluate the effectiveness of the hygroscopic dilator in the colposcopic examination of the endocervical canal in patients with high-grade lesion in the cytopathology and unsatisfactory colposcopy. METHODS: prospective study, including 62 patients with unsatisfactory colposcopic examination and cytology compatible with high-grade intraepithelial lesion. The patients were submitted to dilation of the endocervical canal by means of a hygroscopic dilator. After dilation, the new colposcopic findings were recorded, and then conization was made through loop electrosurgical excision procedure. The incidence of neoplasic involvement of surgical margins was compared between patients with examinations modified toward satisfactory results and those that remained with unsatisfactory colposcopy. In order to compare the incidence of involved margins and the incidence of residual disease, two retrospective control-groups were used: the GinSat group (n = 35): patients with unsatisfactory colposcopy; GSat group (n = 38): patients with satisfactory colposcopy and endocervical atypy. RESULTS: 80.6% of the cases presented satisfactory colposcopic vision after dilation. 80.4% of those presented disease-free resection margins. The incidence of disease-free resection margins in patients with persistent unsatisfactory colposcopy after dilation was 36.3%. Affected surgical margins occurred in 28% of the group that had undergone dilation, 28.5% of the cases in GinSat group, and 31.5% in the Gsat group. Follow-up showed the incidence of residual disease in 7.5% of the patients under dilation, 28.5% in the GinSat group and 28.9% in the GSat group. CONCLUSION: the use of hygroscopic dilation improved visualization of lesions of difficult access to the colposcopic examination, thus permitting reduction in the percentage of residual neoplasic disease in patients with unsatisfactory colposcopy treated with loop electrosurgical excision procedure.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2000;22(9):573-577
DOI 10.1590/S0100-72032000000900006
Purpose: to verify the frequency of cervical intraepithelial neoplasia in human immunodeficiency virus (HIV) ¾ infected women. Methods: ninety-nine HIV-seropositive women were studied. The diagnosis of the HIV infection was established through two ELISA tests complemented by Western blot test or indirect immunofluorescence test. As control group, 104 women whose ELISA test was not positive were analyzed. The investigation of cervical intraepithelial neoplasia was achieved by association of Pap smear and colposcopy in both groups. In the cases where colposcopy revealed existence of abnormal transformation zones, NIC diagnosis was obtained through colposcopy-guided biopsy complemented or not by conization. Results: cervical intraepithelial neoplasia was found in 15 of the 99 patients (15.2%), and among them there were ten NIC I, one NIC II and four NIC III. Among the 104 women of the control group, four presented cervical intraepithelial neoplasia (3.8%), one being NIC I and three NIC III. Conclusion: the comparative analysis of the results showed that the frequency of cervical intraepithelial neoplasia was significantly higher among those patients infected with HIV.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2001;23(6):349-354
DOI 10.1590/S0100-72032001000600002
Purpose: to evaluate the histopathologic results of cone specimens of patients undergoing loop electrosurgical excision procedure (LEEP) and their relationship with the localization of the lesion. Methods: in a retrospective study, 134 clinical reports of patients with abnormal findings of cervical cytology and/or biopsy undergoing LEEP were reviewed. The colposcopic findings were divided into three groups according to the localization of the lesion. Group I (n = 36): patients with ectocervical lesions and fully visible squamocolumnar junction; Group II (n = 50): patients with lesions at the ectocervix and endocervix, and Group III (n = 48): patients with unsatisfactory colposcopy. Results: the mean age in Group I was 33 years and there were 8.3% positive margins. In Group II the mean age was 39 years, with 36% positive margins. Group III had a mean age of 48 years and presented 29.2% positive margins. The percentage of residual disease was 4.2% in Group I, 31.6% in Group II and 35.5% in Group III. Conclusion: patients with lesions at the endocervical canal showed a higher rate of positive margins. Patients with high-grade cervical intraepithelial neoplasia at the endocervical canal and older than 40 years have a greater chance of showing positive margins and residual disease, therefore requiring stricter cytologic and colposcopic follow-up.