-
Original Article
Potential Impact of the Z0011 Trial on the Omission of Axillary Dissection: A Retrospective Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):297-303
03-30-2021
Summary
Original ArticlePotential Impact of the Z0011 Trial on the Omission of Axillary Dissection: A Retrospective Cohort Study
Revista Brasileira de Ginecologia e Obstetrícia. 2021;43(4):297-303
03-30-2021Views186See moreAbstract
Objective
To evaluate the number of patients with early-stage breast cancer who could benefit from the omission of axillary surgery following the application of the Alliance for Clinical Trials in Oncology (ACOSOG) Z0011 trial criteria.
Methods
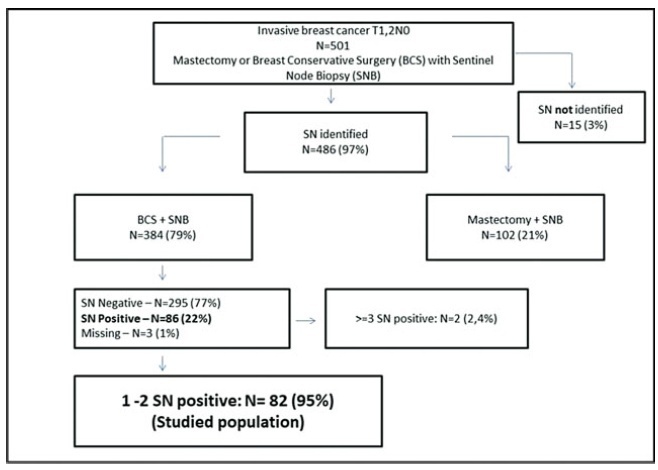
A retrospective cohort study conducted in the Hospital da Mulher da Universidade Estadual de Campinas. The study population included 384 women diagnosed with early-stage invasive breast cancer, clinically negative axilla, treated with breast-conserving surgery and sentinel lymph node biopsy, radiation therapy, chemotherapy and/or endocrine therapy, from January 2005 to December 2010. The ACOSOG Z0011 trial criteria were applied to this population and a statistical analysis was performed to make a comparison between populations.
Results
A total of 384 patients underwent breast-conserving surgery and sentinel lymph node biopsy. Of the total number of patients, 86 women underwent axillary lymph node dissection for metastatic sentinel lymph nodes (SNLs). One patient underwent axillary node dissection due to a suspicious SLN intraoperatively, thus, she was excluded fromthe study. Among these patients, 82/86 (95.3%) had one to two involved sentinel lymph nodes andmet the criteria for the ACOSOG Z0011 trial with the omission of axillary lymph node dissection. Among the 82 eligible women, there were only 13 cases (15.9%) of lymphovascular invasion and 62 cases (75.6%) of tumors measuring up to 2 cm in diameter (T1).
Conclusion
The ACOSOG Z0011 trial criteria can be applied to a select group of SLNpositive patients, reducing the costs and morbidities of breast cancer surgery.
-
Artigos Originais
Efetividade de um manual de exercícios domiciliares na promoção da continência urinária durante a gestação: um ensaio clínico aleatorizado pragmático
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(10):460-466
10-01-2015
Summary
Artigos OriginaisEfetividade de um manual de exercícios domiciliares na promoção da continência urinária durante a gestação: um ensaio clínico aleatorizado pragmático
Revista Brasileira de Ginecologia e Obstetrícia. 2015;37(10):460-466
10-01-2015DOI 10.1590/SO100-720320150005361
Views230See morePURPOSE:
To evaluate the effectiveness of an illustrated home exercise guide targeting the pelvic floor muscles in promoting urinary continence during pregnancy.
METHODS:
A randomized clinical trial was performed with 87 participants, evaluated six times during pregnancy and divided into three groups: Gsup, supervised; Gobs, not supervised, and Gref, women who did not perform the home exercises program. A miction diary and perineometry were used to evaluate urinary incontinence (primary outcome) and pelvic floor muscle strength (secondary outcome), respectively. The Kruskal-Wallis test with post hoc Dunn's and chi-square and Z tests with Bonferroni correction were used for continuous variables and proportions, respectively, with the level of significance set at 5%.
RESULTS:
At the end of the study, 6.9% of pregnant women in the Gsup and Gobs had urinary incontinence, while 96.6% of Gref women were incontinent. Regarding pelvic floor muscle function, Gsup and Gobs had mean contractions of 10 and 8.9 cmH2O, respectively, while Gref had a value of 4.7 cmH2O. Both results were significant.
CONCLUSION:
An illustrated home exercise guide targeting the pelvic floor muscles is effective in promoting urinary continence during pregnancy, even without permanent supervision.
-
Artigos Originais
Effect of a short-term functional training program on body composition in postmenopausal women
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(9):404-409
09-01-2014
Summary
Artigos OriginaisEffect of a short-term functional training program on body composition in postmenopausal women
Revista Brasileira de Ginecologia e Obstetrícia. 2014;36(9):404-409
09-01-2014DOI 10.1590/SO100-720320140005073
Views88See morePURPOSE:
To evaluate the effect of 8 weeks of functional training on body composition in postmenopausal women.
METHODS:
The study was conducted on 38 postmenopausal women, divided into two groups: Training Group (TG) and Control Group (CG). TG women (n=21) performed a program of physical exercise for a period of 8 weeks, 3 times a week on nonconsecutive days, with 90 minutes per session. For the same period, CG women (n=17) did not perform any systematic physical activity. All participants were assessed at baseline and after 8 weeks. The evaluations were performed by the same trained raters. Analysis of body composition was performed using dual-energy X-ray absorptiometry (DEXA), which allows estimation of body composition in the whole body and by segment. TG participants performed a functional exercise program 3 days a week (non-consecutive), with 11 stations consisting of exercises developed in circuit format sessions. The objectives of the exercises were the development of strength, agility, coordination and proprioception, followed by aerobic exercise (walking). After normality of the data was determined by the Shapiro-Wilk test (p<0.05), we applied the Student t-test for independent samples to check for possible differences in anthropometric variables and body composition between groups at both times of intervention (pre and post-test). All analyses were performed using the SPSS software v. 17.0 (SPSS Inc., Chicago, IL, USA) with the level of significance set at 5%.
RESULTS:
At baseline, no significant difference was observed between groups regarding anthropometric body variables or age composition, indicating homogeneity of the groups. After 8 weeks of training, significant differences were observed between TG and CG regarding fat - CG=0.2±0.7 and TG=-0.4±0.5, total body fat (kg) - CG=0.2±1.3 and TG=-0.7±0.8, and total weight - CG=0.4±1.4 and TG=-0.6±1.1. Percent body fat was reduced in terms of absolute values, although without significance: CG=0.1±1.5 and TG=-0.8±1.5.
CONCLUSION:
Functional training in circuit format can be used as a strategy to alter body composition in postmenopausal women, particularly in terms of reduction of adipose tissue. This is a model that promotes high adhesion on the part of the participants, suggesting that it is an attractive proposal for the investigated age group.
-
Artigos Originais
Titrated oral solution of misoprostol for labour induction: a pilot study
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(5):208-213
08-26-2010
Summary
Artigos OriginaisTitrated oral solution of misoprostol for labour induction: a pilot study
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(5):208-213
08-26-2010DOI 10.1590/S0100-72032010000500002
Views106PURPOSE: to test effectiveness and safety of the oral administration of a new misoprostol formulation in titrated doses for the induction of delivery of a live fetus at term. METHODS: an open pilot multicenter, non-randomized clinical trial was conducted from July to December 2008. A total of 30 patients with indications for induction of labor were included. The patients had a live fetus, Bishop score <6, vertex presentation, fetal weight <4,000g estimated by ultrasonography and amniotic fluid index >5. Exclusion criteria were previous uterine scar, non-reassuring fetal heart rate tracing, multiple pregnancy, fetal growth restriction, genital hemorrhage and presence of genital tumors, ulcerations or malformations. An initial dose of 20µg/hour of the oral misoprostol solution was used in the first 6 hours, and was increased progressively to 20µg/hour every 6 hours if labor did not start, up to a maximum dose of 80µg/h in the first 24 hours, maintained for additional 24 hours if necessary. RESULTS: labor was satisfactorily induced in 96.7% of patients. The interval between the first dose and the beginning of uterine contractions was 3.8±1.8 hours. The interval between the initial dose and delivery varied from 6 to 24 hours. The frequency of vaginal delivery was 80% (24 cases). Most of the patients (60%; n=18) initiated labor with a dose of 20mg/hour. Tachysystole occurred in 13.3% of women and meconium-stained fluid was detected in 20% of cases. There were two cases of Apgar scores <7 in the first minute and no Apgar score <7 in the fifth minute. CONCLUSIONS: the oral solution of misoprostol was effective and safe for the induction of labor. However, further randomized controlled trials are needed to compare this new formulation with misoprostol administered by the vaginal route.
Key-words Administration, oralClinical trialLabor, inducedLabor, obstetricMisoprostolMulticenter studySee more -
Trabalhos Originais
Vaginal hysterectomy versus abdominal hysterectomy in patients without uterine prolapse: a randomized clinical trial
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(3):169-176
09-08-2003
Summary
Trabalhos OriginaisVaginal hysterectomy versus abdominal hysterectomy in patients without uterine prolapse: a randomized clinical trial
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(3):169-176
09-08-2003DOI 10.1590/S0100-72032003000300005
Views90PURPOSE: to compare intra- and postoperative results of vaginal hysterectomy with those of abdominal hysterectomy in women without genital prolapse or adnexal pathology. METHODS: a randomized, open clinical trial was conducted, involving 35 patients without genital prolapse scheduled for total hysterectomy due to benign disease, at IMIP, Recife, Brazil. These patients were randomly assigned to vaginal hysterectomy (19 patients) or abdominal hysterectomy (16 patients). Main outcome measures included estimated blood loss, rate of blood transfusion, duration of surgery, postoperative pain (intensity and analgesic requirement), time in hospital, postoperative complications, recovery time and patient satisfaction. Statistical analysis was performed using chi2, exact Fisher and Mann-Whitney tests at a 5% level of significance. RESULTS: estimated blood losses were significantly lower in vaginal hysterectomy (median of 520 mL) than in abdominal hysterectomy (median 902 mL). There was no blood transfusion among patients of the vaginal hysterectomy group, in contrast to 19% of the abdominal hysterectomy group. Duration of surgery was similar (median of 120 min in both groups). Postoperative pain, as measured by visual analog scale and analgesic requirement, was lower for vaginal hysterectomy than for abdominal hysterectomy. There was no statistically significant difference regarding frequency of postoperative complications. There was one case of infection in each group and one case of thrombosis in the vaginal hysterectomy group. Postoperative hospital stay was shorter in the vaginal group. Recovery time was significantly shorter in the vaginal group (median of 35 days) versus the abdominal group (median 40 days). Overall patient satisfaction with the operation was similar in the two groups. CONCLUSIONS: patients without genital prolapse submitted to vaginal hysterectomy for treatment of benign diseases had some advantages in relation to those submitted to abdominal hysterectomy: lower intraoperative blood loss, lower postoperative pain and faster recovery time. Vaginal hysterectomy may replace abdominal hysterectomy in most patients who require hysterectomy.
Key-words Abdominal hysterectomyClinical trialGynecologic surgeryPostoperative complicationsVaginal hysterectomySee more -
Trabalhos Originais
Treatment of bacterial vaginosis with Schinus terebinthifolius Raddi vaginal gel: a randomized controlled trial
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(2):95-102
07-04-2003
Summary
Trabalhos OriginaisTreatment of bacterial vaginosis with Schinus terebinthifolius Raddi vaginal gel: a randomized controlled trial
Revista Brasileira de Ginecologia e Obstetrícia. 2003;25(2):95-102
07-04-2003DOI 10.1590/S0100-72032003000200004
Views83See morePURPOSE: to test the efficacy of and tolerance to Schinus terebinthifolius Raddi gel in the treatment of bacterial vaginosis. METHODS: forty-eight women with symptomatic bacterial vaginosis (according to Amsel's criteria) were enrolled in a randomized, double-blind, controlled trial comparing Schinus terebinthifolius Raddi gel (25 cases) with placebo (23 cases). The main outcome parameters were: rate of cure, presence of lactobacilli in Pap smear after treatment and side effects. Statistical analysis was performed using the chi2 and the Fisher exact test at 5% level of significance. RESULTS: using Amsel's clinical parameters of bacterial vaginosis, the cure rate was 84% in the Schinus group and 47.8% in the placebo group (p=0.008). A significant increase in the frequency of lactobacilli was observed in the Pap smear of the group treated with Schinus (43.5%) compared to the patient group (4.3%) (p=0.002). Treatment-related adverse events were not frequent in either group. CONCLUSIOS: the present study indicates that Schinus vaginal gel is effective and safe in the treatment of bacterial vaginosis. In addition, potential beneficial effects on the vaginal flora are suggested.


