Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2011;33(11):334-340
DOI 10.1590/S0100-72032011001100003
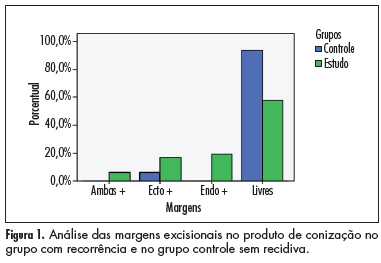
PURPOSE: To evaluate the ability of various factors related to the conization process in cytological/histological cervical intraepithelial neoplasias (CIN), after therapeutic conization. METHODS: A retrospective review was conducted of patients who had undergone conization due to CIN 2 and 3, from January 1999 to January 2006. They were divided into two groups: case group (residual disease or recurrence) and control group (without residual disease or recurrence), during 18 months of follow up. Univariate and multivariate analysis were used to define the predictive factors of disease recurrence. The c2 test or Fisher exact test was used for statistical analysis, with the level of significance set at p£0.05. RESULTS: Forty-eight patients showed recurrence/progression of CIN (case group) and 65 showed no recurrence/progression of disease (control group). Age and parity were similar in the two groups, as determined by calculation of the mean and standard deviation. There was no difference in smoking habits or in the use of contraceptive methods. The recurrence rate was 14.6%. Only conization positive margins were predictors of recurrence/progression (p<0.001). The conization techinique, the surgeon, CIN grade, gland involvement, and size of the uterine volume removed were not related to the evolution of disease after surgery. CONCLUSION: The recurrence of CIN 2 and 3 was related to positive margins in the product of conization.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(8):368-373
DOI 10.1590/S0100-72032010000800002
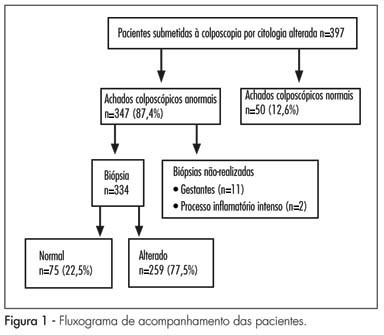
PURPOSE: to evaluate the agreement between conventional cytology using the Papanicolaou test, repeated at the time of colposcopy, with colposcopic and histopathological findings. METHODS: the study was carried out at the central public health laboratory of the state of Pernambuco between January and July, 2008, involving 397 women referred for colposcopic evaluation following an abnormal cervical smear test. Cytology was repeated at the time of colposcopy using conventional method, with particular attention being paid to the presence of abnormal colposcopic findings. The nomenclature used for cytology was the 2001 Bethesda system terminology, while that used for histology was the World Health Organization 1994 classification. Cytology performed at the time of colposcopy was compared with colposcopy and with histopathology obtained by colposcopy-directed biopsy. The Kappa coefficient was used to evaluate the agreement between methods, as well as the χ2 test, with the level of significance set at 5%. RESULTS: poor agreement was found between cytology performed at the time of colposcopy and colposcopic findings (K=0.33; 95%CI=0.21-0.45) and between colposcopy and histopathology (K=0.35; 95%CI=0.39-0.51). Cytology performed at the time of colposcopy compared with histopathology revealed a Kappa of 0.41 (95%CI=0.29-0.530), which was considered to reflect moderate agreement. CONCLUSIONS: agreement was better between cytology and histopathology than between colposcopy and cytology or between colposcopy and histopathology.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2010;32(7):315-320
DOI 10.1590/S0100-72032010000700002
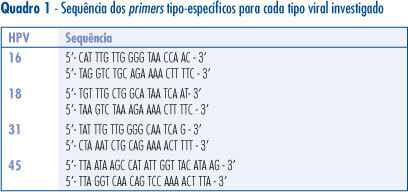
PURPOSE: to determine the prevalence of HPV 16, 18, 31 and 45 in cervical screening samples of women with cellular changes and/or colposcopy suggestive of persistent high grade or low grade lesion who were submitted to conization. METHODS: a total of 120 women were included in the study. Histological analysis of the cervical cones revealed 7 cases of cervicitis, 22 of CIN1, 31 of CIN2, 54 of CIN3, and 6 invasive carcinomas. The cervical screening samples were analyzed before conization for the presence of HPV-DNA by PCR using the consensus primers PGMY09/11. HPV-DNA-positive samples were tested for the presence of HPV16, 18, 31 and 45 using type-specific primers for these HPV. RESULTS: HPV-DNA was detected in 67.5% of the studied women. HPV 16 (40%) was the most prevalent type in most ilesions, followed by HPV 31 (13.3%), 45 (13.3%), and 18 (4.1%). Multiple infections occurred in 15% of the cases and infections with other HPV types were detected in 14% of the sample. CONCLUSIONS: HPV 16 and 18 infections do not always occur as a single infection, and may be associated with other HPV types on different occasions.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(12):604-608
DOI 10.1590/S0100-72032009001200005
PURPOSE: to evaluate the results of treatment to which patients with high grade intraepithelial cervical neoplasia (HSIL) are submitted, as well as their follow-up during pregnancy. METHODS: retrospective study based on the review of the medical report of 30 patients with diagnosis of high-grade squamous intraepithelial lesions (HSIL) during pregnancy and attended to at a tertiary hospital in southern Brazil from 1990 to 2002. Diagnosis was performed by colposcopy and biopsy, with repetition of the colposcopy during the pregnancy and after delivery. The diagnoses of regression and progression of lesions were evaluated. RESULTS: from 30 patients, 3 were excluded of the sample because the diagnosis of high-grade squamous intraepithelial lesions (HSIL) was not confirmed by the colposcopy with biopsia. Four patients were submitted to treatment during pregnancy, and one of them presented preterm delivery at the 32nd week. Twenty-three patients were submitted to expectant treatment, underwent a new colposcopy and biopsy, and then were submitted to conisation surgery at about the 11th week after the end of pregnancy. In 7.4% of the cases, there was lesion regression in the surgical specimen. CONCLUSIONS: all patients with diagnosis should be submitted to colposcopy and biopsy to exclude the possibility of invasive lesion. The expectant procedure for intraepithelial lesions is the most widely chosen and safe due to the possibility of regression in the postpartum period.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(2):61-66
DOI 10.1590/S0100-72032008000200003
PURPOSE: to demonstrate the expression of biomarkers, detected by immunohistochemical techniques in healthy tissues, as well as in preneoplastic and neoplastic lesions of the uterine cervix. METHODS: in order to evaluate the immunohistochemical reactivity of tissues from the uterine cervix to p16 and to type 2 herpes simplex virus (HSV-2), 187 samples of low-grade intraepithelial lesions (LG-IEL) and high-grade intraepithelial lesions (HG-IEL), and of uterine cervix carcinoma were compared with a group of patients without uterine cervix lesions. Statistical analysis was done by the chi2 test for trends. The significance level was alpha=0.05. RESULTS: the reactivity to p16 was assessed showing the following distribution: group without uterine cervix lesions: 56% (24/43), LG-IEL: 92% (43/47), HG-IEL: 94% (43/46), and cancer: 98% (46/47) (p<0.001, linear trend). Concerning the HSV-2: group without uterine cervix lesions: 27% (12/45), LG-IEL: 58% (22/38), HG-IEL: 78% (35/45), and cancer: 59 % (29/49) (p<0.001, linear trend). There was an increase in the reactivity ratio for the two markers in the pathological groups (LG-IEL, HG-IEL and uterine cervix cancer, at p<0.001) compared to controls. There was no significant difference between the LG-IEL and the HG-IEL groups. CONCLUSIONS: a progressive increase of reactivity ratios of the studied immunohistochemical markers as a function of lesion severity was observed.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(9):536-544
DOI 10.1590/S0100-72032006000900006
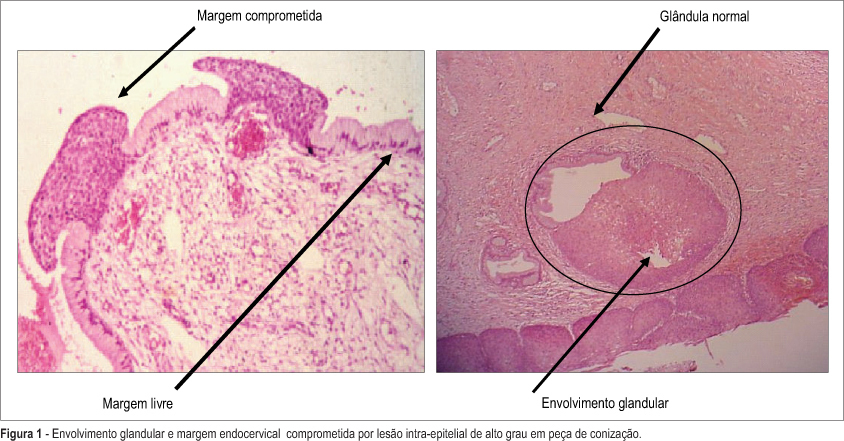
PURPOSE: to evaluate risk factors associated with cervical intraepithelial lesion recurrence after LEEP conization. METHODS: nested case-control study in a cohort of 201 patients with cervical intraepithelial lesion, that were submitted to LEEP conization. Average follow-up of these patients was 2 years. Ninety-four HIV-infected women and 107 non-infected were enrolled. Cervical conization was achieved by the Loop Electrosurgical Excision Procedure (LEEP). Evaluated surgical biopsy histopathological characteristics were lesion grade, lesion borders and glandular involvement. After surgery all patients were submitted to a colposcopy and cytological evaluation every six months. Recurrent lesions were defined it confirmed by biopsy after surgery. Cases were patients with and controls patients without recurrence. chi2 test and multivariable analysis by logistic regression were used for group comparisons. Kaplan Meier's method was performed for the survival analyses (log-rank test). RESULTS: 40 patients had lesion recurrence. Initially, significant variables were: partner number, HIV-infection, lesion borders and glandular involvement. The most frequent recurrence occurred when there were simultaneous association between positive margins and glandular involvement as indicator for recurrence risk. After logistic regression analysis the main factors associated with lesion recurrence were: glandular involvement (OR-9.1; 95% CI:13.0- 27.5); HIV-infection (OR-4.6; 95% IC:1.1-6.3); compromised margins (OR-2.6; 95% IC:1.9-11.2). CONCLUSIONS: risk factors associated with cervical intraepitelial lesion recurrence were HIV-infection, glandular involvement and compromised margins.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(6):345-351
DOI 10.1590/S0100-72032006000600005
PURPOSE: to evaluate association between CD4+ cell count and cervical intraepithelial lesion severity in HIV-infected women. METHODS: cross-sectional study of 87 HIV-infected patients which were confirmed by previous serologic examinations. All had cervical HPV diagnosed by polymerase chain reaction (PCR). All patients underwent anamnesis, physical examinations and colposcopy. Cervix biopsy was performed when indicated by colposcopical examination. Histopathological results followed Richart's classification, adapted by Wright, and CD4+ cell count and cervical intraepithelial lesion severity association was analysed by comparison of means using analysis using analysis of variance (ANOVA). RESULTS: among 60 biopsied women 24 were found (40.0%) with CIN I, eight (13.3%) with CIN II, three (5%) with CIN III, 14 (23.3%) with chronic cervicitis and 11 with cytopathic effect of HPV, without cell polarity loss. This corresponds to 35 (58.3%) women with intraepithelial lesion of low grade (CIN I + HPV) and 11 (18.3%) with intraepithelial lesion of high grade (CIN II + CIN III). There was no significant association between CD4+ cell count mean and cervical intraepithelial lesion severity (p=0.901). CONCLUSIONS: there was no association between CD4+ cell count and cervical intraepithelial lesion severity diagnosed by histopathological examination.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2006;28(2):75-80
DOI 10.1590/S0100-72032006000200002
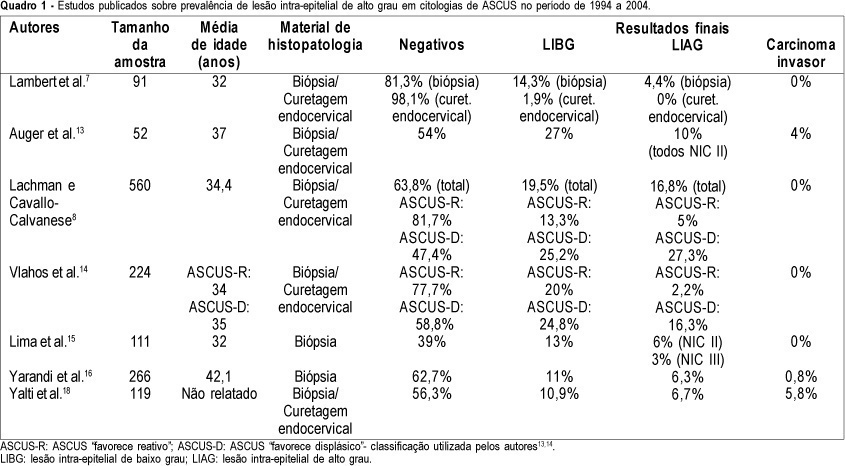
PURPOSE: to determine the prevalence of high-grade squamous intraepithelial lesions (HSIL) and cancer in women with cytological diagnosis of persistent ASCUS (atypical squamous cells of undetermined significance) for 6 months in the last 7 years. We also assessed if age could be a predictive factor for presence of HSIL/cancer in this group. METHODS: we included 215 cases of non-pregnant and HIV-seronegative women with cytological diagnosis of persistent ASCUS (unespecific) with at least 6 months of interval between smears. This cytological diagnosis was compared to histological diagnosis obtained by biopsy (large loop excision of the transformation zone) or cone biopsies, and considered negative when colposcopy was satisfactory without lesions or, when unsatisfactory, no lesion was detected after at least one cytological and colposcopic follow-up. RESULTS: among the 215 cases, 49.3% had negative results (CI 95%: 42.6-55.9). The prevalence of histological confirmed low-grade squamous intraepithelial lesion was 38.6% (CI 95%: 32.1- 45.1) and HSIL was 10.7% (CI 95%: 6.5-14.8). Cases of cancer were found in 1.4% of patients (CI 95%: 0-2.9). We could not find a significant difference between the prevalence of HSIL/cancer according to age group using the cutoff point of 35 years. CONCLUSION: HSIL/cancer prevalence observed in this study has shown the risk of finding this kind of lesions in about 12% of women assisted in our public health system with two cytological diagnosis of ASCUS. A higher probability of HSIL/cancer in the different age groups was not found but this result was limited by our small sample size.