Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2025;47:e-rbgo97
01-23-2025
Our aims to compare level of serum ischemia modified albümin(IMA) between healthy and preeclamptic pregnancies and to evaluate the relationship of IMA with preeclampsia, preeclampsia severity and perinatal outcomes.
Our study is a prospective case-control study. A total of 134 pregnant women (66 preeclamptic and 68 healthy pregnant) between 18-45 years of age and between 24- 41 gestational weeks participated. Serum IMA levels were measured by the Albumin Cobalt Binding (ACB) test.
The mean IMA values were found to be significantly higher in the preeclampsia group compared to the control group (p<0,001). Patients were divided into 3 groups; severe preeclampsia(n=29), non-severe preeclampsia(n=37) and healthy pregnant(n=68). Statistically significant difference was not found between severe preeclampsia and non-severe preeclampsia (p=0.505). The performance of IMA values in predicting the development of preeclampsia among all participants was evaluated with Receiver Operating Characteristic (ROC) analysis. According to the ROC analysis, the best cut-off value at which the maximum area under the curve (AUC) was obtained was found when IMA>0.98(AUC: 0.690 95% Confidence Interval (CI): 0.600-0.781 p<0.001). When IMA threshold value of >0.98 was taken to predict preeclampsia; the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated as 65.15%, 64.71%, 64.18%, and 65.67%, respectively.
IMA level may be a useful new marker in recognizing and predicting preeclampsia. However, despite the power of recognizing the disease, serum IMA levels do not give an idea about the severity of the disease. More comprehensive studies are needed in order to use IMA levels in the diagnosis of preeclampsia.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo66
07-26-2024
This study aimed to investigate the effects of the presence of subchorionic hematoma (SH) in early pregnancies with threatened miscarriage (TM) on levels of first-trimester maternal serum markers, pregnancy-associated plasma protein-A (PAPP-A), and free β-human chorionic gonadotropin (β-hCG) levels.
The data of TM cases with SH in the first trimester between 2015 and 2021 were evaluated retrospectively. The data of age and gestational age-matched TM cases without SH were also assessed to constitute a control group. Demographic characteristics, obstetric histories, ultrasonographic findings, and free β-hCG and PAPP-A levels of the groups were compared.
There were 119 cases in the study group and 153 cases in the control group. The median vertical and longitudinal lengths of the SH were 31 mm and 16 mm. The median age of both groups was similar (p=0.422). The MoM value of PAPP-A was 0.088 (.93) in the study group and 0.9 (0.63) in the control group (p=0.519). Similarly, the MoM value of free β-hCG was 1.04 (0.78) in the study group and 0.99 (0.86) in the control group (p=0.66). No significant relationship was found in the multivariate analysis between free β-hCG MoM, PAPP-A MoM, age, gravida, and vertical and longitudinal lengths of the hematoma (p>0.05).
The level of PAPP-A and free β-hCG were not affected by the SH. Therefore, these markers can be used reliably in TM cases with SH for the first-trimester fetal aneuploidy screening test.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2023;45(9):535-541
10-30-2023
Breast cancer (BC) biomarkers, such as hormone receptors expression, are crucial to guide therapy in BC patients. Antiandrogens have been studied in BC; however, limited data are available on androgen receptor (AR) expression test methodology. We aim to report the core needle biopsy (CNB) accuracy for AR expression in BC.
Patients diagnosed with stage I-III invasive BC from a single institution were included. Androgen receptor expression was evaluated by immunohistochemistry (IHC) using 1 and 10% cutoff and the AR expression in surgical specimens (SS) was the gold standard. Kappa coefficients were used to evaluate the intraprocedural agreement.
A total of 72 patients were included, with a mean age of 61 years old and 84% were Luminal A or B tumors. The prevalence of AR expression in all BC samples was 87.5% using a cutoff ≥ 10% in SS. With a cutoff value ≥ 1%, CNB had an accuracy of 95.8% (Kappa value = 0.645; 95% confidence interval [CI]: 0.272–1.000; p < 0.001) and 86.1% (Kappa value = 0.365; 95% CI: 0.052–0.679; p < 0.001) when ≥ 10% cutoff was used for AR positivity. Androgen receptor expression in CNB (cutoff ≥ 1%) had a sensitivity of 98.5%, specificity of 60%, positive predictive value of 97.0%, and a negative predictive value of 76.9% in the detection of AR expression in SS.
Core needle biopsy has good accuracy in evaluating AR expression in BC. The accuracy of CNB decreases with higher cutoff values for AR positivity.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2020;42(9):555-561
10-23-2020
To evaluate the role of clinical features and preoperativemeasurement of cancer antigen 125 (CA125), human epididymis protein(HE4), and carcinoembryonic antigen (CEA) serum levels in women with benign and malignant non-epithelial ovarian tumors.
One hundred and nineteen consecutive women with germ cell, sex cordstromal, and ovarian leiomyomas were included in this study. The preoperative levels of biomarkers were measured, and then surgery and histopathological analysis were performed. Information about the treatment and disease recurrence were obtained from the medical files of patients.
Our sample included 71 women with germ cell tumors (64 benign and 7 malignant), 46 with sex cord-stromal tumors (32 benign and 14 malignant), and 2 with ovarian leiomyomas. Among benign germ cell tumors, 63 were mature teratomas, and, amongmalignant, fourwere immatureteratomas. Themost common tumors in the sex cordstromal group were fibromas (benign) and granulosa cell tumor (malignant). The biomarker serum levels were not different among benign andmalignant non-epithelial ovarian tumors. Fertility-sparing surgeries were performed in 5 (71.4%) women with malignant germ cell tumor. Eleven (78.6%) patients with malignant sex cord-stromal tumors were treated with fertility-sparing surgeries. Five women (71.4%) with germ cell tumors and only 1 (7.1%) with sex cord-stromal tumor were treated with chemotherapy. One woman with germ cell tumor recurred and died of the disease and one woman with sex cord-stromal tumor recurred.
Non-epithelial ovarian tumors were benign in the majority of cases, and the malignant caseswere diagnosed at initial stages with good prognosis. Themeasurements of CA125, HE4, and CEA serum levels were not useful in the preoperative diagnosis of these tumors.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2019;41(4):256-263
06-19-2019
The hypothesis of fetal origins to adult diseases proposes that metabolic chronic disorders, including cardiovascular diseases, diabetes, and hypertension originate in the developmental plasticity due to intrauterine insults. These processes involve an adaptative response by the fetus to changes in the environmental signals, which can promote the reset of hormones and of the metabolism to establish a “thrifty phenotype”. Metabolic alterations during intrauterine growth restriction can modify the fetal programming. The present nonsystematic review intended to summarize historical and current references that indicated that developmental origins of health and disease (DOHaD) occur as a consequence of altered maternal and fetal metabolic pathways. The purpose is to highlight the potential implications of growth factors and adipokines in “developmental programming”, which could interfere in the development by controlling fetal growth patterns. These changes affect the structure and the functional capacity of various organs, including the brain, the kidneys, and the pancreas. These investigations may improve the approach to optimizing antenatal as well as perinatal care aimed to protect newborns against long-termchronic diseases.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(10):593-598
10-01-2018
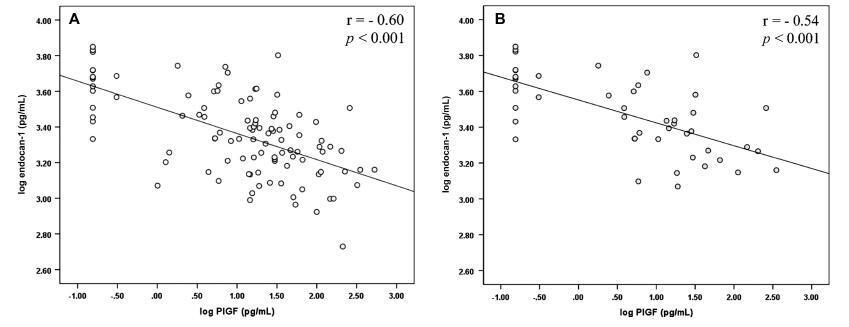
To analyze endocan-1, a biomarker of vascular endothelial related pathologies, and the placental growth factor (PlGF), an angiogenic factor and a placental dysfunction marker in patients with preeclampsia (PE).
Case-control study conducted at Hospital São Lucas, in the city of Porto Alegre, Brazil. Endocan-1 and PlGF levels were quantified in the maternal plasma using the MagPlexTH-C microsphere system (MAGPIX System, Luminex, Austin, Texas, US) and evaluated through analysis of covariance (ANCOVA) and adjusted by body mass index (BMI), gestational age and maternal age. To estimate the difference between the groups, the mean ratio (MR) and the 95% confidence interval (95%CI) were calculated. The Pearson correlation test was used to establish any association between endocan-1 and PlGF levels. The null hypothesis was rejected when p < 0.05.
The group of patients was composed by normotensive (n = 67) patients and patients with PE (n = 50). A negative correlation between endocan-1 and the PlGF was noted in the entire normotensive group (linear correlation coefficient [r] = -0.605; p < 0.001), as well as in the PE group (r = -0.545; p < 0.001).
Endocan-1 levels are increased in patients with PE, and are inversely correlated with PlGF levels. We suggest that it is important to analyze angiogenic and proinflammatory molecules concomitantly in women with PE to better understand the pathophysiology of the disease. Both molecules are strong candidates for PE biomarkers, and future studies will examine any mechanisms connecting these factors in PE.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2018;40(7):384-389
07-01-2018
The main objective of this study was to examine the diagnostic performance of the first-trimester combined test for aneuploidies in unselected pregnancies from Rio de Janeiro and compare it with the examples available in the literature.
We investigated 3,639 patients submitted to aneuploidy screening from February 2009 to September 2015. The examination is composed of the Fetal Medicine Foundation risk evaluation based on nuchal translucency evaluation, mother’s age, presence of risk factors, presence of the nasal bone and Doppler of the ductus venous in addition to biochemical analysis of pregnancy-associated plasma protein A (PAPP-A) and beta-human chorionic gonadotropin (β-hCG) markers. The cut-off point for high risk for aneuploidies was defined as greater than 1:100, with intermediate risk defined between 1:100 and 1:1,000, and low risk defined as less than 1:1,000. The variable aneuploidy was considered as a result not only of trisomy of chromosome 21 but also trisomy of chromosomes 13 and 18.
Excluding the losses, the results of 2,748 patients were analyzed. The firsttrimester combined test achieved 71.4% sensitivity with a 7.4% false-positive (FP) rate, specificity of 92.6%, positive predictive value (PPV) of 6.91% and negative predictive value (NPV) of 99.76%, when the cut-off point considered was greater than 1:1,000. Through a receiving operating characteristics (ROC) curve, the cut-off point that maximized the sensitivity and specificity for the diagnosis of aneuploidies was defined as 1:1,860. When we adjusted the false-positive (FP) rate to 5%, the detection rate for this analysis is 72.7%, with a cut-off point of 1:610.
The combined test of aneuploidy screening showed a detection rate inferior to those described in the literature for a higher FP rate.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(6):273-281
06-01-2017
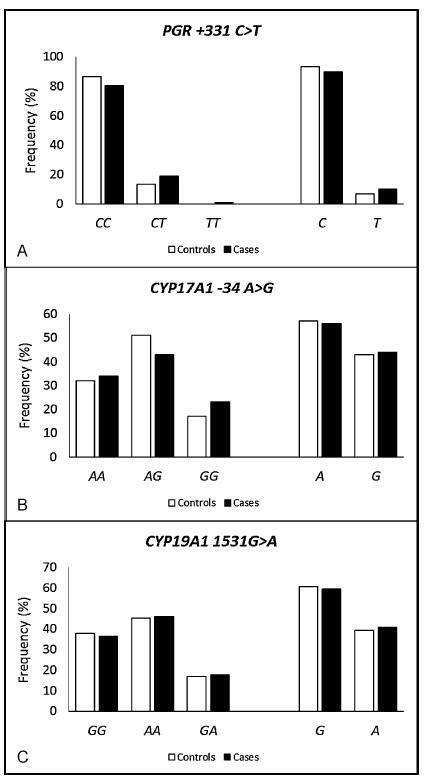
To evaluate the magnitude of the association of the polymorphisms of the genes PGR, CYP17A1 and CYP19A1 in the development of endometriosis.
This is a retrospective case-control study involving 161 women with endometriosis (cases) and 179 controls. The polymorphisms were genotyped by real-time polymerase chain reaction using the TaqMan system. The association of the polymorphisms with endometriosis was evaluated using the multivariate logistic regression.
The endometriosis patients were significantly younger than the controls (36.0±7.3 versus 38.0±8.5 respectively, p = 0.023), and they had a lower body mass index (26.3±4.8 versus 27.9±5.7 respectively, p = 0.006), higher average duration of the menstrual flow (7.4±4.9 versus 6.1±4.4 days respectively, p = 0.03), and lower average time intervals between menstrual periods (25.2±9.6 versus 27.5±11.1 days respectively, p = 0.05). A higher prevalence of symptoms of dysmenorrhea, dyspareunia, chronic pelvic pain, infertility and intestinal or urinary changes was observed in the case group when compared with the control group. The interval between the onset of symptoms and the definitive diagnosis of endometriosis was 5.2±6.9 years. When comparing both groups, significant differences were not observed in the allelic and genotypic frequencies of the polymorphisms PGR + 331C > T, CYP17A1 -34A > G and CYP19A1 1531G > A, even when considering the symptoms, classification and stage of the endometriosis. The combined genotype PGR + 331TT/CYP17A1 -34AA/CYP19A11531AA is positively associated with endometriosis (odds ratio [OR] = 1.72; 95% confidence interval [95%CI] = 1.09-2.72).
The combined analysis of the polymorphisms PGR-CYP17A1-CYP19A1 suggests a gene-gene interaction in the susceptibility to endometriosis. These results may contribute to the identification of biomarkers for the diagnosis and/or prognosis of the disease and of possible molecular targets for individualized treatments.