Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2017;39(2):80-85
To evaluate the association of age at first sexual intercourse with the results of the cervicovaginal cytology.
Observational analytical study about the prevalence of altered cervicovaginal cytology results in women aged between 18 and 34 years from a densely populated area in Brazil, during 10 years. The patients were stratified into 2 categories according to their age at first sexual intercourse (13-16 years and 17-24 years).
From the total of 2,505,154 exams, 898,921 tests were in accordance with the inclusion criteria. Considering women with 4 years or less from the first sexual intercourse as a reference, those with 5 to 9 years and 10 years or more showed a higher prevalence of high-grade squamous intraepithelial lesions (HSILs). Women with an earlier onset of sexual intercourse (13-16 years) showed higher prevalence ratios for atypical squamous cells (ASC), low-grade squamous intraepithelial lesion (LSIL) and HSIL. The prevalence ratio for HSIL adjusted by age at diagnosis and by age at first sexual intercourse was higher only for women with an earlier onset of sexual intercourse.
The age of first sexual intercourse could be a variable that might qualify the selection among young women who are really at a higher risk for HSIL.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2009;31(2):54-60
DOI 10.1590/S0100-72032009000200002
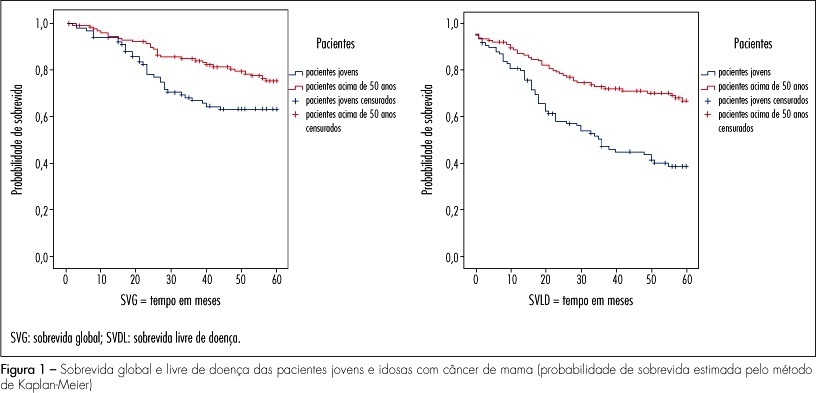
PURPOSE: the objective of this study was to evaluate the clinical, pathological and molecular characteristics in very young women and postmenopausal women with breast cancer. METHODS: we selected 106 cases of breast cancer of very young women (<35 years) and 130 cases of postmenopausal women. We evaluated clinical characteristics of patients (age at diagnosis, ethnic group, family history of breast cancer, staging, presence of distant metastases, overall and disease-free survival), pathological characteristics of tumors (tumor size, histological type and grade, axillary lymph nodes status) and expression of molecular markers (hormone receptors, HER2, p53, p63, cytokeratins 5 and 14, and EGFR), using immunohistochemistry and tissue microarray. RESULTS: when comparing clinicopathologic variables between the age groups, younger women demonstrated greater frequency of nulliparity (p=0.03), larger tumors (p<0.000), higher stage disease (p=0.01), lymph node positivity (p=0.001), and higher grade tumors (p=0.004). Most of the young patients received chemotherapy (90.8%) and radiotherapy (85.2%) and less tamoxifen therapy (31.5%) comparing with postmenopausal women. Lower estrogen receptor positivity 49.1% (p=0.01) and higher HER2 overexpression 28.7% (p=0.03) were observed in young women. In 32 young patients (29.6%) and in 20% of the posmenopausal women, the breast carcinomas were of the triple-negative phenotype (p=0.034). In 16 young women (50%) and in 10 postmenopausal women (7.7%), the tumors expressed positivity for cytokeratin 5 and/or 14, basal phenotype (p=0.064). Systemic metastases were detected in 55.3% of the young women and in 39.2% of the postmenopausal women. Breast cancer overall survival and disease-free survival in five years were, respectively, 63 and 39% for young women and 75 and 67% for postmenopausal women. CONCLUSIONS: breast cancer arising in very young women showed negative clinicobiological characteristics and more aggressive tumors.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2008;30(11):561-565
DOI 10.1590/S0100-72032008001100006
PURPOSE: to evaluate the influence of age on the quality of semen in men submitted to spermatic analysis in a human reproduction service, in cases of conjugal infertility. METHODS: a retrospective study in which the spermiograms of all men in process of investigation for conjugal infertility in a service of assisted reproduction in the Northeast of Brazil were evaluated from September 2002 to December 2004. A number of 531 individuals submitted to 531 spermatic evaluations were included in the study. The following parameters have been analyzed: spermatic volume, concentration, motility and morphology. The men under investigation have been divided in groups, according to the results obtained in each of the variables studied. Seminal volume groups were divided in: hypospermia, normospermia and hyperspermia. Spermatic concentration groups were divided in: azoospermia, oligospermia, normospermia and polyspermia. Motility groups were divided in: normal motility and asthenospermia. Morphology groups were divided in: normal morphology and teratospermia. The t test has been used to compare the average age of patients in groups with normal and in groups with altered parameters. The program XLSTAT (p<0.05) has been used for the statistical analysis. RESULTS: the individuals studied presented an average of 37±7.9 years old, with an average of seminal volume of 3±1.4 mL, a spermatic concentration of 61.4±66.4 spermatozoids by mL of semen, a progressive motility of 44.7±19.4% of the total of spermatozoids and normal morphology of 11.2±6.6% of the spermatozoids. Average age among groups were similar, except for that of individuals with hypospermia, which was significantly higher than the one from men with normospermia (39.6±10.3 versus 36.5±7.3, p=0.001). CONCLUSIONS: age interferes in an inversely proportional way on the ejaculated volume, but does not influence spermatic concentration, motility and morphology.