You searched for:"Roseli Mieko Yamamoto"
We found (41) results for your search.Summary
Rev Bras Ginecol Obstet. 2006;28(8):453-459
DOI 10.1590/S0100-72032006000800003
PURPOSE: to analyze the fetal heart rate (FHR) and umbilical artery Dopplervelocimetry between 18th and 20th weeks of gestation in pregnant women complicated by pregestational diabetes mellitus. METHODS: twenty-eight pregnancies with pregestational diabetes and 27 normal pregnant women were analyzed prospectively, in a cross-sectional and case-control study. The inclusion criteria were the following: singleton pregnancy between 18 and 29 weeks, no other associated maternal diseases and no fetal abnormality. Ultrasonography was performed and FHR was calculated by the interval between the beginnings of two consecutive cardiac cycles, in the three umbilical artery Doppler sonograms, obtained in the umbilical cord near to the placental insertion, using color Doppler. Five consecutive FHR cycles from each sonogram were measured, to analyze mean FHR and its variation. The following Doppler indices were studied: systolic/diastolic ratio, pulsatility index (PI) and resistance index (RI). Student's t test and Mann-Whitney Utest were applied to comparative study. p values were considered significant when p<0.05. Results: no significant difference was observed in mean FHR between the studied groups (diabetic group: 149.2 bpm, control group: 147.2 bpm; p = 0.12). FHR variation revealed similar results between the groups (diabetic group: 5.3 bpm; control group: 5.3 bpm; p=0.50). No significant difference was found in the Doppler indices S/D (p=0.79), PI (p=0.25) and RI (p=0.71) between the groups. CONCLUSIONS: the absence of differences in FHR characteristics between the 18th and 20th gestational weeks indicates similar neurological maturation of FHR regulatory systems in this period, between fetuses of diabetic mothers and controls. Abnormalities in the uteroplacental resistance were not identified in the studied period, in pregnancies complicated by pregestational diabetes.
Summary
Rev Bras Ginecol Obstet. 2000;22(8):503-510
DOI 10.1590/S0100-72032000000800006
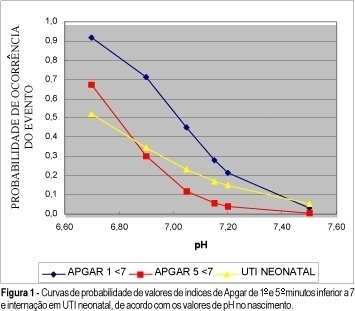
Purpose: to analyze the relationship between the values of pH at birth, fetal surveillance examinatios and neonatal results. Methods: one thousand, three hundred and forty-six high-risk pregnancies were evaluated at the Fetal Surveillance Unit. The assessment of fetal well-being included cardiotocography, fetal biophysical profile and amniotic fluid index. After birth, the perinatal results (gestational age at birth, birth weight, Apgar scores at 1st and 5th minutes, umbilical cord pH at birth) were collected. To study the results, the patients were divided into four groups: G1 (pH <7.05), G2 (pH between 7.05 and 7.14), G3 (pH between 7.15 and 7.19) and G4 (pH > or = 7.20). Results: the abnormal patterns of cardiotocography were associated with pH at birth inferior to 7.20 (p = 0.001). Abnormal results of the fetal biophysical profile (<=4) were related to decrease in pH values at birth (p<0.001). The adverse neonatal outcomes were associated with acidosis at birth, and they were selected to be analyzed by the logistic regression model, showing that the odds ratio of each adverse neonatal outcome increases significantly when the values of pH at birth decrease. Conclusions: significant correlation was found between the values of pH at birth and adverse neonatal results, providing the possibility to estimate the risk of neonatal complications according to the pH values at birth.
Summary
Rev Bras Ginecol Obstet. 2010;32(10):510-515
DOI 10.1590/S0100-72032010001000007
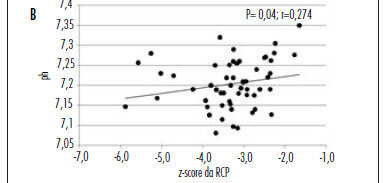
PURPOSE: to evaluate the hypothesis that the fetal cerebroplacental ratio (CPR) is related to acidemia at birth in pregnancies complicated by placental insufficiency detected before 34 weeks of gestation. METHODS: this is a prospective cohort study of 55 patients between 26 and 34 weeks of gestation with a diagnosis of placental insufficiency characterized by abnormal umbilical artery Doppler (pulsatility index>95p). Fetal assessment was performed for each patient by dopplervelocimetry of the umbilical artery, middle cerebral artery and ductus venosus, and by the fetal biophysical profile. CPR was calculated using the ratio between middle cerebral artery pulsatility index and umbilical artery pulsatility index, and the z-score was obtained (number of standard deviations of the mean value at each gestational age). Acidemia at birth was characterized when pH<7.2. RESULTS: of 55 patients, 29 (52.7%) presented acidemia at birth. In the group of fetal acidemia, when compared with the group with pH>7.2, a significant association was observed with CPR values (median 0.47 versus 0.58; p=0.009), pulsatility index of the umbilical artery (median 2.45 versus 1.93; p=0.003), ductus venosus pulsatility index for veins (PIV) (median 1.08 versus 0.85; p=0.034) and suspected or abnormal fetal biophysical profile (37 versus 8%; p=0.031). CPR analysis by z-score showed a negative tendency, but was not statistically significant (p=0.080). Significant correlations were found between pH at birth and CPR (r=0.45; p<0.01), z-score of CPR (r=0.27; p<0.05) and ductus venosus PIV (r=-0.35 p<0.01). CONCLUSION: CPR is associated with the presence of acidemia at birth in pregnancies with placental insufficiency detected before 34 weeks of gestation and this parameter could potentially represent a factor for assessing the severity of fetal involvement.
Summary
Rev Bras Ginecol Obstet. 2009;31(10):513-526
DOI 10.1590/S0100-72032009001000008
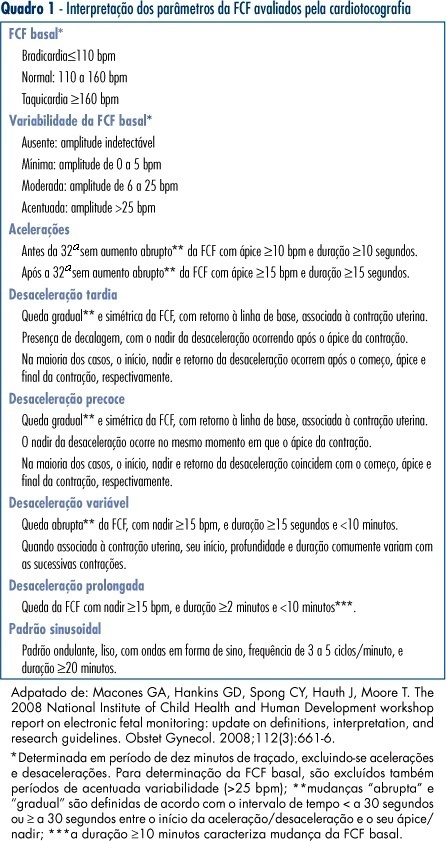
The present context of medical practice demands from the obstetrician and gynecologist broad understanding of the scientific and technological advances of the area. The main purpose of prenatal evaluation is to identify fetuses at risk for adverse events or death, for preventive action to avoid mishappenings. The determination of fetal biophysical profile reaches its maximum efficiency when applied within the clinical context of each case. In high risk gestations, the Doppler velocimetry of the umbilical artery has shown to be useful to improve perinatal outcome. In the fetal growth deficit, due to severe placentary insufficiency, Doppler velocimetry of the venous duct has been showing to be an important tool in handling of the cases before the 34th week of gestation. Although no test itself is considered the best to evaluate the fetus's prenatal vitality, the joint analysis of all methods may lead to a better understanding of the fetal response to hypoxia.
Summary
Rev Bras Ginecol Obstet. 1998;20(9):517-524
DOI 10.1590/S0100-72031998000900005
Purpose: to determine the behavior of doppler velocimetry during the course of risk pregnancies and to compare the perinatal results obtained for concepti with retarded intrauterine growth (RIUG) with those for concepti considered adequate for gestational age (AGA). Methods: a prospective study of the evolution of doppler ultrasound was made in 38 pregnant women with of idiopathic intrauterine growth retardation (IUGR) in previous pregnancy. A relationship was established between this antecedent and the new pregnancy. The pregnant women studied were divided into two groups in agreement with their neonates birthweight. Group 1 was associated with IUGR and group 2 with adequate birth weight. IUGR was confirmed in 23.7% of the cases. Umbilical and uterine artery doppler velocimetry was performed from 20 to 40 weeks of gestation. Middle cerebral artery doppler velocimetry was analyzed after 28 weeks of gestation, twice a month, being the last valued examination before birth. Results: the uterine and umbilical artery ratio at 24 and 28 weeks of gestation, respectively, correlated with the presence of IUGR. There was no difference between the two groups regarding the presence or absence of a small notch in the uterine artery wave form and middle cerebral artery doppler velocimetry ratio, at the last examination before birth. There was a relationship between neonatal stay in hospital for more than three days and the presence of IUGR. Conclusions: doppler ultrasound should be used in the follow-up of cases with a high risk of IUGR. It allows the detection of the fetuses at high risk of hypoxia and, by interrupting the pregnancy, fetal distress-related complications may be avoided.
Summary
Rev Bras Ginecol Obstet. 2014;36(11):519-524
DOI 10.1590/S0100-720320140005100
To validate a questionnaire to be applied in order to learn and describe the perceptions of specialists in obstetrics and gynecology about their experience and self-confidence in the emergency care for vaginal delivery.
This was a prospective study for the validation of an instrument that contains statements about emergency obstetrical care: breech delivery (n=23), shoulder dystocia (n=20), postpartum haemorrhage (n=24), forceps delivery (n=32), and vacuum extractor (n=5). Participants gave their opinions on each item by applying the Likert scale (0=strongly disagree, 1=partially disagree, 2=indifferent, 3=partially agree and 4=strongly agree). The questionnaire was applied to 12 specialists in obstetrics and gynecology and it was expected to be found a level of comprehension exceeding 80%. A five-point scale was used to assess the understanding of each question (from 0=did not understand anything to 5=understood perfectly and I have no doubt). A score above 4 was considered to indicate sufficient understanding. The instrument used was specially designed to suit the specific demands. The analysis of internal reliability was done using the Cronbach alpha coefficient. For external validation, we calculated the proportion of items with full understanding for each subscale. For research purposes, the alpha should be greater than 0.7.
Participants had a mean age of 33.3 years, with 5.0 standard deviation (SD), and an average interval time since graduation from medical school of 5.8 years (SD=1.3 years). All were specialists with residency in obstetrics and gynecology. The mean proportion of participants who fully understood the items in each emergency was 97.3% for breech delivery, 96.7% for shoulder dystocia, 99.7% for postpartum hemorrhage, 97.4% for forceps delivery, and 98.3% for the use of a vacuum extractor. The results of Cronbach's alpha for the items in each emergency studied were: 0.85 for breech delivery, with 0.72 lower limit of 95% confidence interval ((%%CI), 0.74 for shoulder dystocia (lower limit of 95%CI=0.51), 0.79 for postpartum hemorrhage (lower limit of 95%CI=0.61), 0.96 for forceps delivery (lower limit of 95%CI=0.92), and 0.90 for the vacuum extractor (lower limit of 95%CI=0.79).
The validated questionnaire is useful for learning and describing the perception of physicians about their experience and self-confidence in emergency care for vaginal births.
Summary
Rev Bras Ginecol Obstet. 2009;31(11):547-551
DOI 10.1590/S0100-72032009001100004
PURPOSE: to study the effect of acoustic stimulation in the fetal cardiac response, according to parameters from computerized cardiotocography in low risk pregnancies. METHODS: twenty low risk pregnant women were included in the study, according to the following criteria: age over 18; single gestation, living fetus; gestational age between 36 and 40 weeks; amniotic liquid index over 8.0 cm and absence of fetal malformation. Cases with post-natal diagnosis of fetal anomaly were excluded. Computerized cardiotocography was performed for 20 minutes, before and after fetal acoustic stimulation. Results were analyzed by the t test for dependent samples, with significance level at p<0.05. RESULTS: acoustic stimulation was successfully performed in all cases analyzed. By the analysis of the cardiotocographic parameters, there was no significant difference when the pre and post-stimulation parameters were compared: average number of fetal movements per hour (55.6 versus 71.9, p=0.1); mean basal fetal heart rate (FHR) (135.2 versus 137.5 bpm, p=0.3); mean FHR increases>10 bpm (6.5 versus 6.8, p=0.7); mean FHR increases>15 bpm (3.8 versus 4.3, p=0.5); mean duration of high FHR variation episodes (11.4 versus 10.9 min, p=0.7); mean duration of low FHR variation episodes (2.5 versus 1.1 min, p=0.2), and mean short-term variation (10.6 versus 10.9 ms, p=0.6). CONCLUSIONS: in low risk gestations at term, computerized cardiotocography has not evidenced differences in the FHR parameters after the fetal sonic stimulation.
Summary
Rev Bras Ginecol Obstet. 2013;35(2):55-59
DOI 10.1590/S0100-72032013000200003
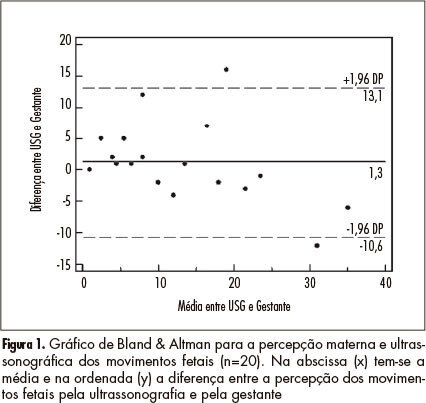
PURPOSE: To determine the agreement between maternal perception of fetal movements and the movements recorded simultaneously by ultrasound in low-risk pregnancies. METHODS: Twenty pregnant women were evaluated with the following inclusion criteria: single pregnancy, alive fetus, maternal age between 18 and 35 years; between 36 and 40 weeks gestation; normal fetal morphology at ultrasound, and absence of maternal comorbidities. The pregnant women were evaluated for 10 minutes, during which cardiotocography was used to record fetal movements triggered with the event marker, with the paper speed set at 3 cm/min. At the same time, fetal movements were observed by ultrasonography. RESULTS: The kappa index for interobserver agreement analysis was 0.62, showing good agreement (95%CI 0.45 - 0.79). The intraclass correlation coefficient was 0.82 (95%CI 0.61 - 0.92). Analysis by the Bland & Altman graph indicated good agreement. A linear regression analysis showed a significant correlation between maternal perception (x) and ultrasound (y) observation (r²=0.71, p<0.001; equation: y=5.31+0.66x). CONCLUSIONS: The agreement between ultrasound and maternal perception of fetal movement is good, allowing the use of fetal movement counting in the assessment of fetal wellbeing.