You searched for:"Maria Laura Costa"
We found (27) results for your search.Summary
Rev Bras Ginecol Obstet. 2023;45(10):555-556
Summary
Rev Bras Ginecol Obstet. 2022;44(6):557-559
Summary
Rev Bras Ginecol Obstet. 2021;43(7):560-569
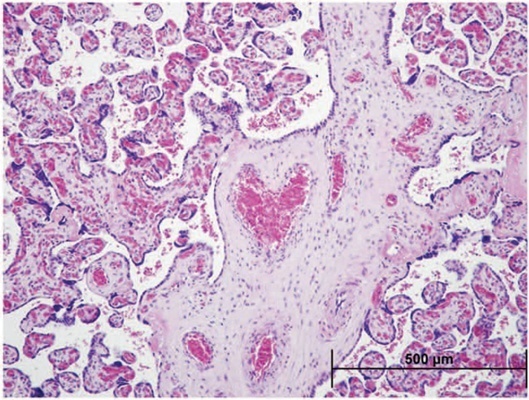
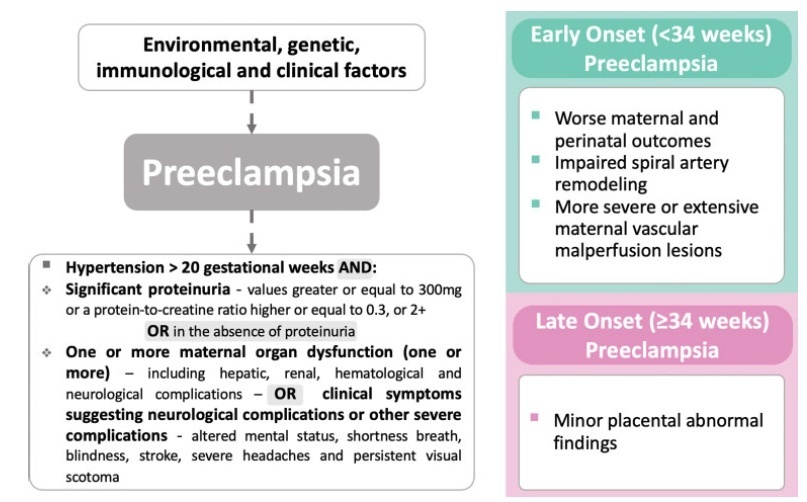
Preeclampsia (PE) is a pregnancy complication associated with increased maternal and perinatal morbidity and mortality. The disease presents with recent onset hypertension (after 20 weeks of gestation) and proteinuria, and can progress to multiple organ dysfunction, with worse outcomes among early onset preeclampsia (EOP) cases (<34 weeks). The placenta is considered the root cause of PE; it represents the interface between the mother and the fetus, and acts as a macromembrane between the two circulations, due to its villous and vascular structures. Therefore, in pathological conditions, macroscopic and microscopic evaluation can provide clinically useful information that can confirm diagnosis and enlighten about outcomes and future therapeutic benefit.
To perform an integrative review of the literature on pathological placental findings associated to preeclampsia (comparing EOP and late onset preeclampsia [LOP]) and its impacts on clinical manifestations.
Cases of EOP presented worse maternal and perinatal outcomes, and pathophysiological and anatomopathological findings were different between EOP and LOP placentas, with less placental perfusion, greater placental pathological changes with less villous volume (villous hypoplasia), greater amount of trophoblastic debris, syncytial nodules, microcalcification, villous infarcts, decidual arteriolopathy in EOP placentas when compared with LOP placentas. Clinically, the use of low doses of aspirin has been shown to be effective in preventing PE, as well asmagnesium sulfate in preventing seizures in cases of severe features.
The anatomopathological characteristics between EOP and LOP are significantly different, with large morphological changes in cases of EOP, such as
Summary
Rev Bras Ginecol Obstet. 2020;42(9):577-585
The aim of the current review is to present a systematic evaluation of reported human placental findings in cases of zika virus (ZIKV) infection.
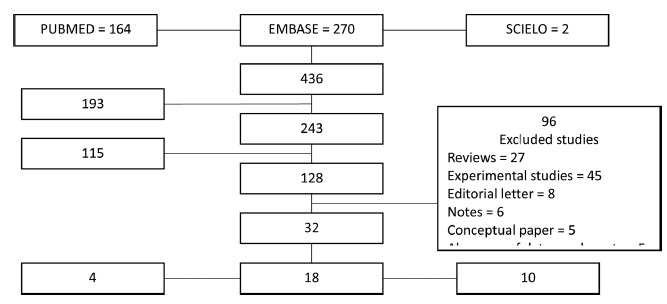
sources We reviewed the EMBASE, PUBMED, and SCIELO databases until June 2019, without language restrictions. Selection of studies The search terms placenta AND zika virus were used. The inclusion criteria of the studies were studies that reported placental findings in humans. Experimental studies, reviews, notes or editorials were excluded. A total of 436 studies were retrieved; after duplicate exclusion, 243 articles had their titles screened, and 128 had their abstract read; of those, 32 were included in the final analysis (18 case reports, 10 case series, and 4 cohorts)
We collected data concerning the author, year of publication, study design, number of participants, number of placental samples, onset of symptoms, perinatal outcomes, and main findings on histological analysis.
The placental pathologic findings were described as mild and nonspecific, similar to those of other placental infections, including chronic placentitis, chronic villitis, increased Hofbauer cells, irregular fibrin deposits, increased mononuclear cells in the villus stroma, villous immaturity, edema, hypervascularization, stromal fibrosis, calcification, and focal necrosis of syncytiotrophoblasts.
Zika infection presents unspecific placental findings, similar to other infections in the toxoplasmosis, other agents, rubella, cytomegalovirus, and herpes (TORCH)group. Characterizing and standardizing placental findings after zika virus infection is key to understanding the mechanisms of congenital diseases.
Summary
Rev Bras Ginecol Obstet. 2022;44(6):593-601
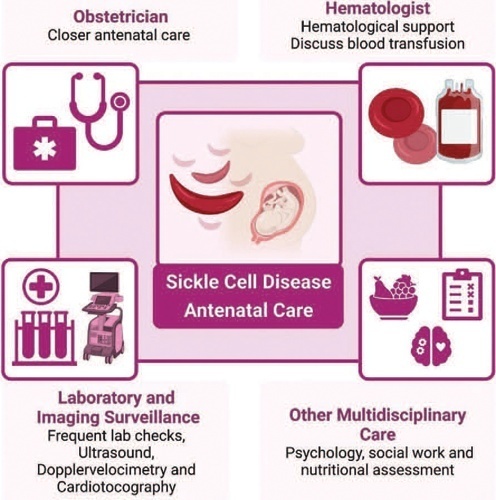
Sickle cell disease (SCD) is the most common monogenic disease worldwide, with a variable prevalence in each continent. A single nucleotide substitution leads to an amino-acid change in the β-globin chain, altering the normal structure of hemoglobin, which is then called hemoglobin S inherited in homozygosity (HbSS) or double heterozygosity (HbSC, HbSβ), and leads to chronic hemolysis, vaso-occlusion, inflammation, and endothelium activation. Pregnant women with SCD are at a higher risk of developing maternal and perinatal complications. We performed a narrative review of the literature considering SCD and pregnancy, the main clinical and obstetrical complications, the specific antenatal care, and the follow-up for maternal and fetal surveillance. Pregnant women with SCD are at a higher risk of developing clinical and obstetric complications such as pain episodes, pulmonary complications, infections, thromboembolic events, preeclampsia, and maternal death. Their newborns are also at an increased risk of developing neonatal complications: fetal growth restriction, preterm birth, stillbirth. Severe complications can occur in patients of any genotype. We concluded that SCD is a high-risk condition that increases maternal and perinatal morbidity and mortality. A multidisciplinary approach during pregnancy and the postpartum period is key to adequately diagnose and treat complications.
Summary
Rev Bras Ginecol Obstet. 2021;43(1):61-65
Pre-eclampsia (PE) is a severe disorder that affects up to 8% of all pregnancies and represents an important cause of maternal and perinatal morbidity and mortality. The screening of the disease is a subject of studies, but the complexity and uncertainties regarding its etiology make this objective a difficult task. In addition, the costs related to screening protocols, the heterogeneity of the most affected populations and the lack of highly effective prevention methods reduce the potential of current available algorithms for screening. Thus, the National Specialized Commission of Hypertension in Pregnancy of the Brazilian Association of Gynecology and Obstetrics Federation (Febrasgo, in the Portuguese acronym) (NSC Hypertension in Pregnancy of the Febrasgo) considers that there are no screening algorithms to be implemented in the country to date and advocates that Aspirin and calcium should be widely used.
Summary
Rev Bras Ginecol Obstet. 2017;39(11):622-631
Preeclampsia, a multifactorial disease with pathophysiology not yet fully understood, is a major cause of maternal and perinatal morbidity and mortality, especially when preterm. The diagnosis is performed when there is an association between arterial hypertension and proteinuria or evidence of severity. There are unanswered questions in the literature considering the timing of delivery once preterm preeclampsia has been diagnosed, given the risk of developingmaternal complications versus the risk of adverse perinatal outcomes associated with prematurity. The objective of this systematic review is to determine the best timing of delivery for women diagnosed with preeclampsia before 37 weeks of gestation.
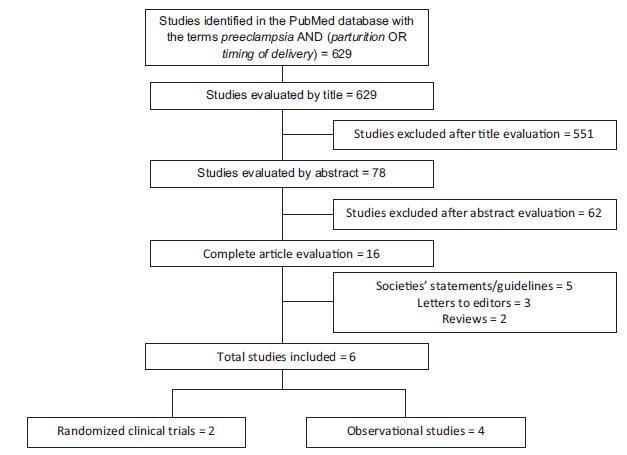
Systematic literature review, performed in the PubMed database, using the terms preeclampsia, parturition and timing of delivery to look for studies conducted between 2014 and 2017. Studies that compared the maternal and perinatal outcomes of women who underwent immediate delivery or delayed delivery, in the absence of evidence of severe preeclampsia, were selected.
A total of 629 studies were initially retrieved. After reading the titles, 78 were selected, and their abstracts, evaluated; 16 were then evaluated in full and, in the end, 6 studies (2 randomized clinical trials and 4 observational studies) met the inclusion criteria. The results were presented according to gestational age range (< 34 weeks and between 34 and 37 weeks) and by maternal and perinatal outcomes, according to the timing of delivery, considering immediate delivery or expectant management. Before 34 weeks, thematernal outcomeswere similar, but the perinatal outcomes were significantly worse when immediate delivery occurred. Between 34 and 37 weeks, the progression to severe maternal disease was slightly higher among women undergoing expectant management, however, with better perinatal outcomes.
When there is no evidence of severe preeclampsia or impaired fetal wellbeing, especially before 34 weeks, the pregnancy should be carefully surveilled, and the delivery, postponed, aiming at improving the perinatal outcomes. Between 34 and 37 weeks, the decision on the timing of delivery should be shared with the pregnant woman and her family, after providing information regarding the risks of adverse outcomes associated with preeclampsia and prematurity.
Summary
Rev Bras Ginecol Obstet. 2022;44(7):686-691
To review literature and estimate the occurrence of preeclampsia and its complications in Brazil.
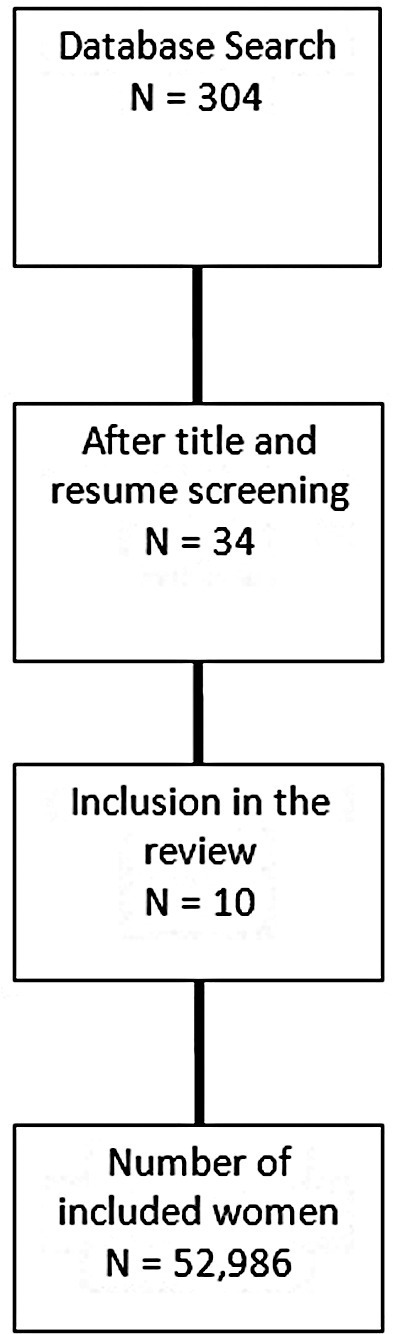
We performed an integrative review of the literature, and included observational studies published until August 2021 on the SciELO and PubMed databases that evaluated preeclampsia among pregnant women in Brazil. Other variables of interests were maternal death, neonatal death, hemolysis, elevated liver enzymes, and low platelet count (HELLP) syndrome, and eclampsia. Three independent reviewers evaluated all retrieved studies and selected those that met inclusion criteria. A metanalysis of the prevalence of preeclampsia and eclampsia was also performed, to estimate a pooled frequency of those conditions among the studies included.
We retrieved 304 studies after the initial search; of those, 10 were included in the final analysis, with a total of 52,986 women considered. The pooled prevalence of preeclampsia was of 6.7%, with a total of 2,988 cases reported. The frequency of eclampsia ranged from 1.7% to 6.2%, while the occurrence of HELLP syndrome was underreported. Prematurity associated to hypertensive disorders ranged from 0.5% to 1.72%.
The frequency of preeclampsia was similar to that reported in other international studies, and it is increasing in Brazil, probably due to the adoption of new diagnostic criteria. The development of a national surveillance network would be essential to understand the problem of hypertensive disorders of pregnancy in Brazil.