Summary
Rev Bras Ginecol Obstet. 2004;26(6):429-433
DOI 10.1590/S0100-72032004000600002
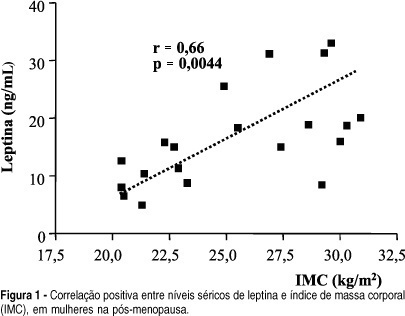
OBJECTIVE: to correlate serum leptin concentration with bone mineral density (BMD) in postmenopausal women. METHODS: twenty-two healthy postmenopausal women were included in the present study. BMD was measured by dual energy X-ray absorptiometry at the lumbar spine and femoral neck. Serum leptin concentrations were determined using an immunoradiometric assay. Statistical analysis was performed by ANOVA and Dunn and Pearson's correlation tests. RESULTS: mean BMD values were 0.898 ± 0.140 g/cm² at the lumbar spine and 0.760 ± 0.152 g/cm² at the femoral neck. Mean serum leptin concentration was 17.2 ± 9.4 ng/ml and no significant differences were observed among women with normal BMD, osteopenia and osteoporosis (18.6 ± 7.8, 18.9 ± 9.9 and 15.6 ± 10.6, respectively; p > 0.05). No significant correlations were observed between serum leptin levels and BMD measurements at the lumbar spine and femoral neck, when the whole sample was considered and when patients were divided into groups with osteoporosis and/or osteopenia and a control group. We observed a positive significant correlation between serum leptin levels and body mass index (BMI) (r = 0.66; p = 0.0044). CONCLUSIONS: there was no direct correlation between leptin and BMD in postmenopausal women, although we observed positive significant correlation between leptin and BMI. This fact indicates a possible indirect effect of leptin on bone metabolism.
Summary
Rev Bras Ginecol Obstet. 2004;26(6):435-439
DOI 10.1590/S0100-72032004000600003
OBJECTIVES: The aim of the present study was to evaluate the nuclear grade, the expressions of p53 and c-erbB-2 proteins, and the estrogen receptors (ER) of 38 women with ductal carcinoma in situ (DCIS) and invasive carcinoma of the same breast. METHODS: the protein profile of 38 women was investigated in a descriptive and retrospective study, through the immune-histochemical technique. The cut-off limit for positive staining was chosen at 10% or more of positive cells for p53 and c-erbB-2 proteins and for ER. The analysis of the concordance between the expressions of proteins and the nuclear grade was done by the kappa coefficient, according to Landis and Koch's criteria. MacNemar's test was used to assess the differences between the two groups. RESULTS: there was a perfect concordance in the expression of p53 proteins (kappa coefficient = 1.00) and almost a perfect concordance for c-erbB-2 proteins, ER and nuclear grade (kappa coefficients = 0.84, 0.89 and 0.89) between in situ and invasive elements of the same tumor. CONCLUSION: there was no difference between the expressions of p53 and c-erbB-2 proteins, ER and nuclear grade in the DCIS and invasive carcinoma of the same breast.
Summary
Rev Bras Ginecol Obstet. 2004;26(6):441-447
DOI 10.1590/S0100-72032004000600004
OBJECTIVE: to compare Baden and Walker's (BW) classification system to the International Continence Society (ICS) standardization of terminology of female pelvic organ prolapse. METHODS: information about urogynecological investigation on 101 women, performed by the Urogynecology and Vaginal Surgery Sector of UNIFESP/EPM, was retrospectively analyzed. Only patients who had undergone the standard ICS exam which quantifies the pelvic prolapse were selected. According to ICS, the prolapse is analyzed through a standard reference system relating the hymen to the anatomic position of six vaginal points: two in the anterior vaginal wall, two in the vaginal apex and other two in the posterior vaginal wall. The maximum amount of pelvic organ prolapse was viewed and recorded during a Valsalva's maneuver. The measurement of the most distal point of the prolapse was performed and it was compared to the BW classification system. The data were analyzed by kappa statistics, to assess the concordance between the two terminologies. RESULTS: There was total correspondence only for the posterior vaginal prolapse stage IV (one patient) and for the uterus prolapse stage 0 (29 patients) with severe rectocele and absence of prolapse, respectively, according to BW. In the three types of prolapses evaluated, the values of kappa statistics were below 0.4, indicating a weak concordance between the two terminologies. There is an extensive variation in the measurement of the most distal point of prolapse when the BW classification is perfomed. CONCLUSIONS: there is a weak concordance between the BW classification system and the ICS standardization of terminology of female pelvic organ prolapse.
Summary
Rev Bras Ginecol Obstet. 2004;26(6):449-454
DOI 10.1590/S0100-72032004000600005
OBJECTIVE: to study the effect of a single contraceptive implant of nomegestrol acetate (Uniplant) on the ovarian function, cervical mucus production and sperm penetration, when inserted in women in the preovulatory phase. METHODS: twenty women with regular menstrual cycles were included in an open comparative study. All participants were investigated during one menstrual cycle before (control) and one menstrual cycle after implant insertion. Measurements of estradiol, LH, and progesterone, as well as transvaginal sonography, cervical mucus examination and sperm penetration test, were carried out. Statistical analysis was performed with the paired t-test and the non-parametric test of Wilcoxon. RESULTS: all control cycles were ovulatory and presented normal parameters. Preovulatory estradiol and LH peak decreased significantly from 603.2 ± 78.0 pmo/l and 22.5 ± 6.5 IU/l at pre-insertion to 380.7 ± 51.9 pmol/l and 4.9 ± 1.3 IU/l 48 hours after implant insertion (p < 0.05 and p < 0.01, respectively). Progesterone levels did not vary significantly (control cycle = 49.8 ± 3.3 nmol/l and treated cycle = 43.2 ± 5.2 nmol/l). Cervical mucus and sperm penetration tests were profoundly affected in 10.5% of the users 20 h after implant insertion, in 68.5% after 24 h and in 100% after 48 h. Follicular rupture occurred in the majority of the cycles 48 h after implant insertion. CONCLUSIONS: the use of a single implant of nomegestrol acetate affected estradiol and LH preovulatory peaks and disrupted the process of cervical mucus production and sperm penetration, but it was unable to prevent ovulation when inserted at the preovulatory phase, which reinforces the need to insert the implant during the first five days of the menstrual cycle.
Summary
Rev Bras Ginecol Obstet. 2004;26(6):457-462
DOI 10.1590/S0100-72032004000600006
OBJECTIVE: to assess the ability of Pap smear and hybrid capture II (HCII) to detect clinically significant cervical lesions (CIN2/3) in women referred to hospital due to atypical squamous cells of unknown significance (ASCUS) or low-grade squamous intraepithelial lesions (LSIL). METHODS: a cross-sectional study comprising 161 women referred to the Taubaté University Hospital due to ASCUS/LSIL, between August 2000 and September 2002. All women responded to a questionnaire regarding sociodemographic and reproductive characteristics and were subjected to gynecological examination with specimen collection for Pap test and HCII, along with colposcopy and eventual cervical biopsy. The relationship between HCII results and age, use of condom, oral hormonal contraception, and smoking were evaluated by the chi-square test. The sensitivity, specificity, positive and negative predictive values of both Pap test and HCII were calculated. All calculations were performed within 95% confidence intervals. RESULTS: sixty-seven percent of the women that tested positive for HPV were less than 30 years old. Pap smear and HCII showed the same 82% sensitivity in detecting CIN2/3 when the threshold for a positive Pap result was ASCUS, LSIL or HSIL. Pap smear specificity and positive predictive values were substantially increased when only HSIL results were considered as positive (from 29 to 95% and 12 to 50%, respectively). These figures were superior to those of HCII, but at the expense of an expressive loss of sensitivity (from 82% to 41%). CONCLUSIONS: our results substantiate the potential of HCII in detecting CIN2/3 among women referred due to ASCUS/LSIL.
Summary
Rev Bras Ginecol Obstet. 2004;26(6):463-469
DOI 10.1590/S0100-72032004000600007
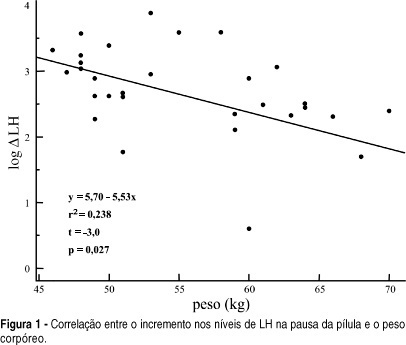
OBJECTIVE: to evaluate serum levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) in the pill-free interval of a combined oral contraceptive containing 20 mg of ethynylestradiol and 75 mg of gestodene. METHODS: thirty-one women from 17 to 36 years old, mean age of 24.5 years old, 19% adolescents, were included. FSH, LH, prolactin (PRL) and estradiol (E2) levels were measured by immunochemoluminescence. Both FSH and LH levels were measured within the last four days of pill intake and on the 7th day of the pill-free interval between two cycles. Hormonal levels were compared by the Student t-test. Comparisons between hormonal and anthropometric data were made by linear regression; values of p < 0.05 were taken as significant. RESULTS: seventy-one percent of women were using the pill for the first time. FSH levels increased from 1.3 to 5.7 mIU/ml between the end of the blister pack and the 7th day of the pill-free interval. LH increased from 0.8 to 4.3 mIU/ml. E2 levels changed from 20.2 to 28.0 pg/ml. The levels of PRL decreased from 12.4 to 10.2 ng/ml. There was no correlation between the changes in gonadotrophin levels and most of the anthropometric parameters in these women, with body mass index < 25 kg/m². CONCLUSION: the gonadotrophin levels detected on the last four days of pill intake were greatly suppressed, recovery of three to four times in amount occurring on the 7th day of the pill-free interval.
Summary
Rev Bras Ginecol Obstet. 2004;26(6):471-475
DOI 10.1590/S0100-72032004000600008
OBJECTIVE: to evaluate the correlation between the beta-human chorionic gonadotropin (beta-hCG) serum levels and the measurement of the endometrial thickness, in patients under treatment of ectopic pregnancy with methotrexate. METHODS: a prospective study in which the levels of beta-hCG as well as the largest measurement of the endometrial thickness on the uterine longitudinal axis through transvaginal ultrasound were evaluated at 24-48 h intervals in thirty-eight patients with hemodynamic stability, ectopic pregnancy, diameter <3.5 cm, and increased beta-hCG levels. All the patients got methotrexate in a single-dose therapy (50 mg/m² im). We compared the mean values of beta-hCG and endometrial thickness of cases that evolved successfully versus the poor responders using the Student t-test. Afterwards we analyzed the difference of the beta-hCG mean serum values related to the endometrial thickness(<10.0 mm and >10.0 mm) independently of the response to treatment employing the Student t-test. RESULTS: the mean values of beta-hCG and endometrial thickness in patients with successful treatment (28 cases) were 1936.2 mIU/ml and 6.4 mm, respectively, significanlty lower than the mean values for insuccessful cases: 6831.3 mIU/ml and 11.7 mm, respectively (p<0.05). The mean values of beta-hCG in women with endometrial thickness <10.0 mm were 2008.7 mIU/ml, significantly lower than the ones with endometrium >10.0 mm, whose mean values were 6925.9 mIU/ml (<0.05). CONCLUSIONS: the measurement of the endometrial thickness through ultrasound is under the beta-hCG serum values influence, and it showed to be a valuable additional factor to suggest medical treatment with methotrexate in the non-disrupted ectopic pregnancy.
Summary
Rev Bras Ginecol Obstet. 2004;26(6):477-482
DOI 10.1590/S0100-72032004000600009
OBJECTIVE: to evaluate the neonatal morbidity and mortality related to mothers at the age of 35 or older than that. METHODS: in 2377 births in a year, 316 newborns (13.26%) from mothers at the age of 35 or more were selected for the study. These women were compared to pregnant controls aged 20 to 29, randomly selected among the 1170 women in the same age group (49,2%). For the inclusion criteria, pregnancies should have been over 22 weeks and the newborns should have weighted 500g or more at birth. Fourteen twin cases were excluded. To evaluate mortality and morbidity the following variables were considered: Apgar Index, birth weight, newborn health conditions, fetal malformations and neonatal mortality until hospital discharge. RESULTS: when analyzed as a whole, nulliparous and multiparous women showed significantly less favorable perinatal results for the selected group of women at 35 or more years old as compared with pregnant controls, what was not sustained when the nulliparous were excluded. Multiparous at the age of 35 or over presented a higher rate of low Apgar index in the 1st minute: 21.3 and 13.1%: (p<0,0033); small NB for the gestational age: 15.2% and 6.7% (p<0,02); big NB for the gestational age: 5.7 and 0.0% (p<0,02); low weight at birth: 23.8 and 14,5% (p<0,01), and prematurity, 16,7 and 6,7%, (p<0,005). Significant differences were not found for the Apgar index in the 5th minute, fetal malformations, newborn health conditions at hospital discharge and neonatal mortality. CONCLUSIONS: Neonatal morbidity increased among pregnant women at the age of 35 and older, but not the neonatal mortality.