You searched for:"Rodrigo de Aquino Castro"
We found (11) results for your search.-
Review Article
Systematic Review of Oral Therapy for the Treatment of Symptoms of Bladder PainSyndrome: The Brazilian Guidelines
Rev Bras Ginecol Obstet. 2018;40(2):96-102
Summary
Review ArticleSystematic Review of Oral Therapy for the Treatment of Symptoms of Bladder PainSyndrome: The Brazilian Guidelines
Rev Bras Ginecol Obstet. 2018;40(2):96-102
Views2See moreAbstract
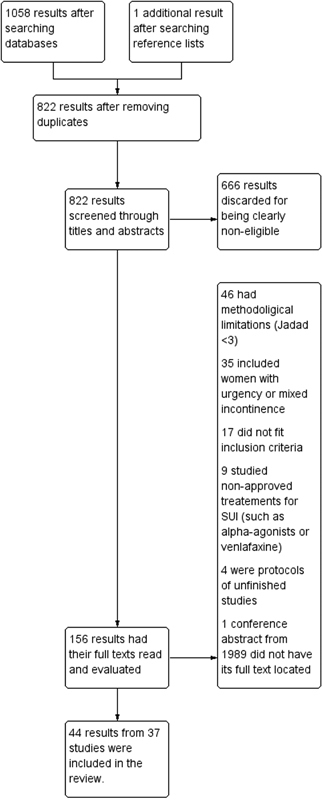
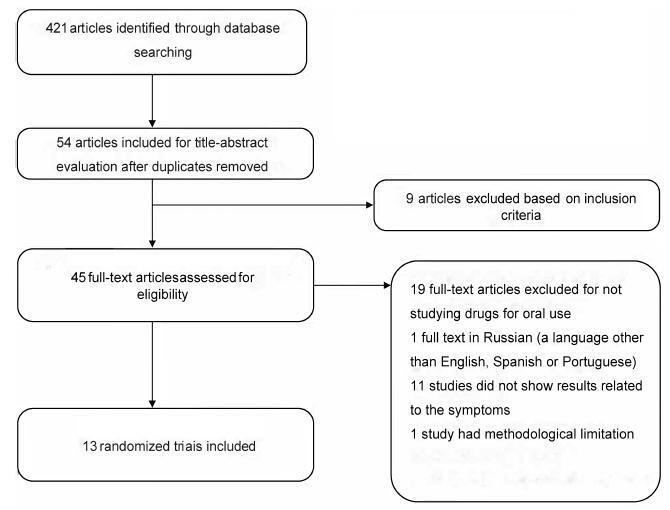
Interstitial cystitis (IC), including bladder pain syndrome (BPS), is a chronic and debilitating disease thatmainly affectswomen. It is characterized by pelvic pain associated with urinary urgency, frequency, nocturia and negative urine culture,with normal cytology. In 2009, the Society for Urodynamics and Female Urology (SUFU) defined the term IC/BPS as an unpleasant sensation (pain, pressure, and discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptoms for more than 6 weeks duration, in the absence of infection or other identifiable causes. This is the definition used by the American Urological Association (AUA) in the most recent guidelines on IC/BPS. Interstitial cystitis may be sufficiently severe to have a devastating effect on the quality of life, but it may also be associated with moderate symptoms whose effects are less debilitating. Although there are several clinical trials to assess oral and intravesical therapies, the treatment for IC remains far from ideal. This systematic assessment evaluates published randomized clinical trials on oralmedications used totreat symptoms of BPS. This studywas performed according to the preferred reporting items for systematic reviews and metaanalyses (PRISMA)method. Two independent reviewers screened the studies to determine their inclusion or exclusion and to perform the methodological analysis. The inclusion criteria included randomized studiespublishedbetween April of 1988and April of2016 that used oral medications to treat symptoms of BPS or IC. According to the systematic review performed,we should consider pentosan polysulfate as one of the bestoptions of oral drugs for the treatment of BPS symptoms. However, this drug is not an available option in Brazil. Orally administered amitriptyline is an efficacious medical treatment for BPS, and it should be the first treatment offered.
-
Original Article
Uterine Fibroid Symptom – Quality of Life questionnaire translation and validation into Brazilian Portuguese
Rev Bras Ginecol Obstet. 2016;38(10):518-523
Summary
Original ArticleUterine Fibroid Symptom – Quality of Life questionnaire translation and validation into Brazilian Portuguese
Rev Bras Ginecol Obstet. 2016;38(10):518-523
Views1See moreAbstract
Purpose
To translate into Portuguese, culturally adapt and validate the Uterine Fibroid Symptom – Quality of Life (UFS-QoL) questionnaire for Brazilian women with uterine leiomyoma.
Methods
Initially, the UFS-QoL questionnaire was translated into Brazilian Portuguese in accordance with international standards, with subsequent cultural, structural, conceptual and semantic adaptations, so that patients were able to properly answer the questionnaire. Fifty patients with uterine leiomyoma and 19 patients without the disease, confirmed by abdominal pelvic examination and/or transvaginal ultrasound, were selected at the outpatient clinics of the Department of Gynecology of the Universidade Federal de São Paulo (Unifesp). The UFS-QoL questionnaire was administered to all women twice on the same day, with two different interviewers, with an interval of 15 minutes between interviews. After 15 days, the questionnaire was readministered by the first interviewer. Reliability (internal consistency and test-retest), construct and discriminative validity were tested to ratify the questionnaire.
Results
The reliability of the instrument was assessed by Cronbach’s α coefficient with an overall result of 0.97, indicating high reliability. The survey results showed a high correlation (p= 0.94; p 0.001).
Conclusion
The UFS-QoL questionnaire was successfully adapted to the Brazilian Portuguese language and Brazilian culture, showing reliability and validity.
-
Original Article
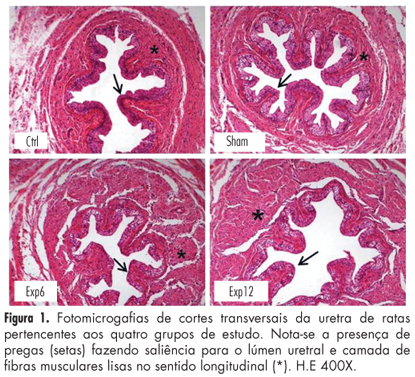
Morphological aspects of the urethra in female rats after electrical stimulation of the pelvic floor
Rev Bras Ginecol Obstet. 2013;35(4):159-163
Summary
Original ArticleMorphological aspects of the urethra in female rats after electrical stimulation of the pelvic floor
Rev Bras Ginecol Obstet. 2013;35(4):159-163
DOI 10.1590/S0100-72032013000400005
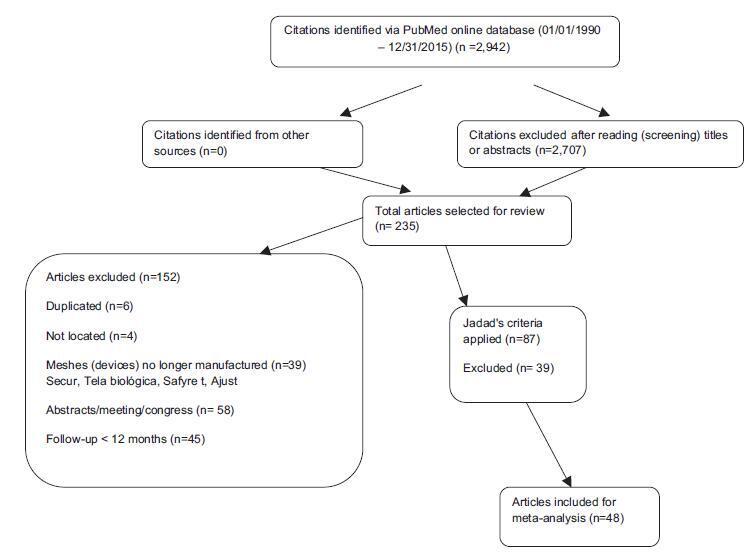
Views1See morePURPOSE: To evaluate the effects of electrical stimulation (ES) of the pelvic floor on the urethra of female rats. METHODS: Forty adult rats were divided at random into four groups of ten animals each: Ctrl – without intervention; Sham – not submitted to ES, but with an electrode inserted into the vagina; Exp6 – submitted to six sessions of ES of the pelvic floor, and Exp12 – submitted to 12 sessions of ES of the pelvic floor. At the end of the experiment, all animals were anesthetized and the middle third of the urethra was removed, fixed in Bouin’s fluid and processed for histomorphometric study. Sections were stained with hematoxylin and eosin for morphological and morphometric description, and others were stained with picrosirius red for the quantitation of total collagen. The thicknesses of the muscle layer and of the epithelium were determined, in 4 quadrants of the urethra, by performing 20 measurements per animal. The number of blood vessels present in the lamina propria was counted in the four quadrants over an area of 10³ µm² per quadrant and the images were obtained using the image analysis program AxioVision® REL 4.3 (Carl Zeiss). The collagen and muscle fiber ratios in the urethrae were calculated from two images per quadrant of every slice stained with picrosirius red, employing the Imagelab® Program. Data were subjected to analysis of variance (ANOVA) and the Tukey-Kramer multiple comparison test (p<0.05). RESULTS: The morphometry of the collagen, number of blood vessels and thickness of the epithelium showed no significant changes; however, the thickness of the periurethral muscle tissue increased significantly in Exp12 group, compared to the other groups (Exp12*>Exp6==Ctrl==Sham; *p<0.05). CONCLUSION: Prolonged functional electric stimulation of the pelvic floor induced an increase in periurethral muscle thickness in rats.
-
Original Article
Collagen histomorphometric evaluation in uterin tissue samples before and after treatment of uterine fibroids with arterial embolization
Rev Bras Ginecol Obstet. 2009;31(12):598-603
Summary
Original ArticleCollagen histomorphometric evaluation in uterin tissue samples before and after treatment of uterine fibroids with arterial embolization
Rev Bras Ginecol Obstet. 2009;31(12):598-603
DOI 10.1590/S0100-72032009001200004
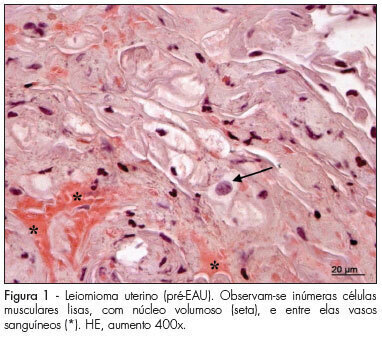
Views0See morePURPOSE: to analyze histomorphometric consequences of the uterine arteries embolization (UAE) in the uterine tissue, especially by collagen tissue quantification through uterine biopsy, before and after treatment of uterine leiomyoma. METHODS: 15 patients with symptomatic leyomioma and/or infertility, submitted to UAE, participated in the study according to the study exclusion criteria, after having signed an informed consent. Uterine biopsy was performed in the secretory phase of the menstrual cycle, before and three months after the procedure, to evaluate the collagen. After the histological processing of the material, 3 µ slices were prepared, some of them dyed with hematoxiline-eosin (HE) and others with the specific dye for collagen fibers (Picrosirius red). Then, the slides were examined and interpreted, and the collagen quantified. The amount was calculated as the percent of the area composed by collagen, and the result expressed in mean±standard deviation (SD). Data has then been submitted to statistical analysis by Student’s paired t test (p<0.05). RESULTS: the presence of smooth muscle cells was observed in the biopsies performed before the treatment, surrounded by a rich network of collagen fibers, which are part of the tumor, blood vessels and fibroblast nuclei. On the slides of biopsies performed after the treatment, it was observed the presence of widespread coagulation necrosis, vascular thrombosis, calcification and lymphoplasmocitary infiltration areas and clear reduction of the collagen component. The percentage of collagen fibers was higher in the pre-UAE group (84.07±1.41), than in the post-UAE (81.05±1.50) group, with p<0.0001, and 95% confidence interval (CI95%) from 2.080 to 3.827. CONCLUSION: the quantitative and qualitative collagen reduction clearly shows that the proposed treatment is efficient in reducing the tumoral mass, composed mainly by collagen fibers intermingled with neoplasic smooth muscle cells. Nevertheless, complementary studies are needed to investigate the functional and biological consequences of these histological changes.
-
Original Article
Risk factors for genital prolapse in a Brazilian population
Rev Bras Ginecol Obstet. 2009;31(1):17-21
Summary
Original ArticleRisk factors for genital prolapse in a Brazilian population
Rev Bras Ginecol Obstet. 2009;31(1):17-21
DOI 10.1590/S0100-72032009000100004
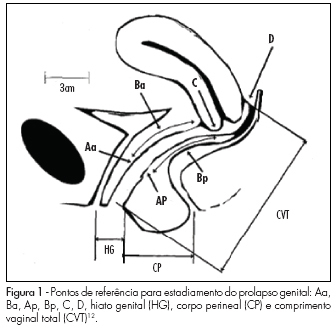
Views3See morePURPOSE: to evaluate risk factors for the development of genital prolapse in the Brazilian population. METHODS: case-control study involving 316 patients submitted to prolapse staging, according to the pelvic organ prolapse quantification system. The patients were divided into two groups: in the Case Group there were 107 patients with prolapse at stage III or IV, and in the Control Group, 209 women at stage 0 or I. In the anamnesis, the selected women have been questioned about the presence of possible risk factors for genital prolapse, such as: age, menopause age, parturition, delivery type (vaginal, caesarean section or forceps), occurrence of fetal macrosomia, family history of genital dystopia in first degree relatives, chronic cough and intestinal constipation. RESULTS: The variables that were different between the groups were: age, body mass index, parturition, number of vaginal, caesarean section or forceps deliveries, newborn weight and positive family history for prolapse. Race, menopause age, chronic cough and intestinal constipation did not present differences between the groups. After logistic regression, only three variables have been shown to be independent risk factors: presence of at least one vaginal delivery, fetal macrosomia and positive family history for dystopia. Cesarean section was shown to be a protective factor. CONCLUSION: in the Brazilian population, the independent risk factor for genital prolapse were: personal antecedent of at least one vaginal delivery, fetal macrosomia and family history of dystopia.
-
Original Article
Pubovaginal sling and tension-free vaginal tape for surgical treatment of stress urinary incontinence in women
Rev Bras Ginecol Obstet. 2008;30(3):127-134
Summary
Original ArticlePubovaginal sling and tension-free vaginal tape for surgical treatment of stress urinary incontinence in women
Rev Bras Ginecol Obstet. 2008;30(3):127-134
DOI 10.1590/S0100-72032008000300005
Views0PURPOSE: to compare sling operations of aponeurosis and tension-free vaginal tape (TVT) for the correction of stress urinary incontinence (SUI) regarding: the rates of subjective and objective healing, the mobility of the bladder neck with ultrasonography, the variation of the absorbent test, the urodynamic alterations and the incidence of complications. METHODS: eighty patients with SUI were selected. Among them, 61 underwent a TVT surgery and 19, an abdominal rectum sling operation of aponeurosis. Average age, index of body mass and parity were 50.1 years old, 29.7 kg/m² and 4.1 deliveries (median=3) for the patients with aponeurosis sling, and 51.7 years old, 28.1 kg/m² and 4.1 deliveries (median=3) for the ones with TVT. All of them have undergone anamnesis, physical examination, bladder neck ultrasonography, absorbent test and urodynamic evaluation before and at least six months after the surgery. After 15 or 19 months and after about four or five years, they were again interviewed concerning the surgery results. RESULTS: after six months, 96.7% of the women with TVT and 89.5% of the ones with sling thought they were healed in the subjective evaluation. Nevertheless, after 15 to 19 months, the TVT Group kept the same subjective healing rate, while among the Sling Group the rate decreased to 77.8%. There was a significant decrease in the mobility of the neck bladder that was similar in both groups and an improvement in the absorbent test. At the end of the urodynamic study, 93.4% of the women from the TVT Group and 78.9% of the ones from the Sling Group were classified as having an objective healing. The average time of bladder probing was higher in the Sling Group. Urinary retention was observed in 42.1% of the sling cases and in 9.8% of the TVT’s. The rates of late healing were 90% for TVT and 55.6% for sling. CONCLUSIONS: TVT surgery provided better subjective healing after 15 or 19 months, but the rate of objective healing was the same in both techniques at that time. Among the complications detected, the urinary retention was higher in the Sling Group, in the post-surgery period.
Key-words Suburethral slingsSurgical procedures, minimally invasiveUrinary incontinence, stressUrologic surgical proceduresSee more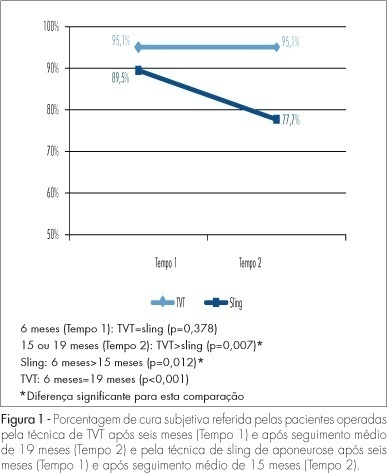
Search
Search in:
Tag Cloud
breast (42) breast cancer (42) breast neoplasms (95) Cesarean section (72) endometriosis (66) infertility (56) Maternal mortality (43) menopause (82) obesity (58) postpartum period (40) pregnancy (225) Pregnancy complications (99) Prenatal care (68) prenatal diagnosis (50) Prevalence (41) Quality of life (51) risk factors (94) ultrasonography (79) urinary incontinence (40) women's health (48)