Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(9):573-577
DOI 10.1590/S0100-72032002000900002
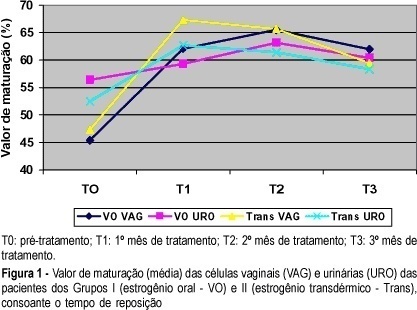
Objective: to study the effects of oral or transdermal estrogen replacement on the lower urinary tract and vagina in postmenopausal women. Methods: we studied 25 postmenopausal women evaluating the oral or transdermic estrogen replacement effects on the vaginal cells and urinary sediment during 3 months. The patients were randomly distributed into 2 groups: Group I, n = 14, treated orally with 0.625 mg equine conjugated estrogen plus 5 mg medroxyprogesterone acetate, daily for 3 months; Group II, n = 11, treated transdermally with 50 mug 17-ß-estradiol, once a week, plus 5 mg medroxyprogesterone. Daily, for 3 months, urinary samples were collected from the first miction in the morning after urogenital antisepsis into sterile tubes. The sample was centrifuged and the sediment was smeared. Vaginal and urinary smears were then fixed in absoluted alcohol and stained by the method of Shorr. Results: the patients who used the oral route presented maturation of the vaginal cells (from 45.4 to 65.5% after 2 months of treatment, maintaing 62% afterwards) but this did not occur with urinary cells (56.4 before treatment versus 60.4% at the end of the period). The transdermal route promoted maturation of vaginal and urinary cells. Conclusion: we have concluded that transdermal estrogens have satisfactory effects both on vaginal and urethral sites. However, with the oral route we did not find the expected results in the urinary tract in all cases.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(9):579-584
DOI 10.1590/S0100-72032002000900003
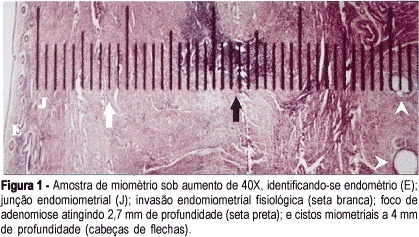
Purpose: to evaluate the sensitivity, specificity, positive and negative predictive values of a clinical and an ecographic method for adenomyosis diagnosis. Methods: a transversal study of validation of the diagnostic method was done, including 95 women in menacme submitted to hysterectomy for various causes. Adenomyosis was diagnosed through a clinical method in women aged 40 years or older, with 2 or more deliveries, increased menstrual bleeding associated with dysmenorrhea. The ecographic diagnosis was established if at least one myometrial ill defined area of abnormal ecotexture was found, which could be hypoechoic, hyperchoic, heterogeneous or cystic. Gold standard was histopathology, defined as the finding of endometrial glands or stroma more than 2.5 cm above the endomiometrial junction. Results: the clinical method had 68.2% sensitivity, 78.1% specificity, 48.4% positive predictive value and 89.1% negative predictive value. For the echographic method this figures were, respectively, 45.5%, 84.9%, 47.6% and 83.8%. Likelihood ratio was 3.11 for the clinical and 3.03 for the echographic method. Considering only those simultaneously positive cases by both methods, sensitivity was below 30% and specificity was near 100%. Considering all positive cases by one or the other method or concomitanty by both, the sensitivity reached 86% and specificity was 60%. Conclusion: the echographic method was not better than the clinical for the diagnosis of adenomyosis.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(9):585-591
DOI 10.1590/S0100-72032002000900004
Purpose: to report 15 breast cancer cases associated with pregnancy and to compare to a control group with breast ductal infiltrating carcinoma, evaluating clinical staging, metastatic axillary lymph node involvement, histopathologic aspects related to nuclear grade, histology grade and estrogen and progesterone hormonal receptors. Method: a retrospective study of 15 cases of patients with breast cancer associated with pregnancy, attended at Mastology Department in the Woman Health Reference Center, Pérola Byington Hospital, São Paulo, was done between September 1996 and April 2001. The evaluation of clinical staging, time of diagnosis and involved axillary lymph nodes was the main study basis. Also age, parity, histologic type, applied treatment, histologic characteristics regarding nuclear grade and histologic grade and the presence of hormonal receptors in the tumors were analyzed. Results: we observed that 7 patients (46.7%) presented a locally advanced breast cancer (clinical stage IIIA and IIIB) and that 3 patients (20%) presented a disseminated disease at the moment of diagnosis. The patients presented on average 2.4 involved axillary lymph nodes and in only one patient the lymph nodes were free of disease (6.6%). Regarding time of diagnosis, 40% of the tumors were diagnosed during the lactational period, 46.7% during the second trimester and 13.3% during the third trimester. The pregnant patients were compared to a control group of non-pregnant patients in the same age range, all of them with infiltrating breast carcinoma, and clinical staging, axillary lymph node involvement, nuclear grade, histologic grade and estrogen and progesterone hormonal receptors were evaluated. There was a statistically significant difference (p=0.0022) regarding clinical staging and axillary lymph node involvement (p=0.0017), and no statistically significant difference as concerns the remaining parameters. Conclusion: breast cancer associated with pregnancy is a neoplasia with a bad prognosis. There is no difference when comparing pregnant patients with non-pregnant patients in the same age range, the advanced clinical staging at the moment of diagnosis being the determinant factor for survival.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(9):601-608
DOI 10.1590/S0100-72032002000900006
Purpose: to appraise the value of ultrasonographic parameters for the diagnosis of fetal Down syndrome (T21), in order to permit its use in routine clinical practice. Methods: this is a prospective cohort study using various ultrasonographic parameters for the prediction of T21. A total of 1662 scans were evaluated in the cohort study and 289 examinations were analyzed as a differential sample to test the normality curve from October 1993 to November 2000. The statistical analysis was based on the calculation of intra- and interobserver variations, the construction of normality curves for the studied parameters, as well as their validity tests, and the calculation of sensitivity, specificity, relative risk, likelyhood ratio and posttest predictive values. Results: among 1662 cases, 22 fetuses (1.32%) with T21 were identified. The normality curves were built for nucal fold thickness, femur/foot ratio and nasal bone length. Renal pelvis had a semiquantitative distribution and the proposed cutoff level was 4.0 mm. Sensitivity, specificity, false positive rate, relative risk and likelyhood ratio for nucal fold measurements above the 95th percentile were 54.5%, 95.2%, 4.9%, 20.2 and 11, respectively. For nasal bone measurements below the 5th percentile, 59.0%, 90.1%, 9.0%, 13.4 and 6.5. For femur/foot ratio below the 5th percentile, 45.5%, 84.4%, 15.6%, 3.7 and 2,6. For renal pelvis greater than 4.0 mm, 36.4%, 89.2%, 10.9%, 4.5 and 3.4. For absent fifth finger middle phalanx, 22.7%, 98.1%, 1.9%, 13.2 and 11.9. For the presence of major malformations, 31.8%, 98.7%, 1.3%, 27.2 and 24,8. After calculating the probability rates and the incidence of T21 in different maternal ages, a table for posttest risk using ultrasonographic parameters was set up. Conclusions: normality curves and indices for the assessment of risk for fetal Down syndrome on a population basis were established by the utilization of different maternal ages and by multiplying factors proposed by the authors. It was not possible to establish a normality curve for renal pelvis measurements, because of their semiquantitative distribution.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(9):609-614
DOI 10.1590/S0100-72032002000900007
Purpose: the objective of the present study was to determine the number and type of deliveries, category of admission to the hospital, occupation and obstetrical diagnosis for adolescents from the municipality of Ribeirão Preto, from January 1992 to December 1996. Methods: the information obtained from hospital discharge forms was analyzed at the Hospital Data Processing Center. The 6.04a-text processor Epi-Info System, a data bank and statistics for epidemiology produced by the Centers of Disease Control and Prevention (Atlanta, GA, USA), and Dbase IV were used to process the information. The association between variables was tested by the chi² test, with the level of significance set at 5%. The analyzed parameters were: number and type of delivery, category of hospital admission, occupation and obstetric diagnosis. Results: a total of 42,969 deliveries occurred during the study period, among which 7,134 (16.6%) corresponded to adolescent deliveries. An increase in the number of deliveries by girls in this age range occurred over the years, from 1,225 in 1992 to 1,538 in 1996. Deliveries were reported starting from 12 years of age, with a gradual increase in this number, especially after 14 years of age, when a 104.2% increase occurred for deliveries at this age, followed by 48.8% at 15 years, 36.1% at 16 years, 14.0% at 17 years, 52.8% at 18 years, and with practically no increase among 19-year-old girls. The highest number of deliveries (5,709) was recorded for the unified health system category of admission, followed by 1,277 deliveries for the prepaid category and 148 deliveries for the private category. With respect to occupation, 14.1% of the patients belonged to the economically active population, while 85.8% did not. Of the total deliveries, 59.2% were normal, 5.6% were forceps deliveries, and 35.2% were cesarean sections. The most frequent obstetrical diagnoses were: problems of fetus or placenta affecting maternal management (7.9%), fetus-pelvis disproportion (6.0%), problems with the amniotic cavity and membranes (5.0%), hypertension complicating delivery and puerperium (3.5%), and premature or false labor (3.4%). Conclusions: most deliveries were normal and occurred more frequently at the end of adolescence, especially among girls belonging to the unified health system. There was a predominance of adolescents not belonging to the economically active population. Some obstetrical complications were diagnosed at the time of resolution of pregnancy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(9):617-622
DOI 10.1590/S0100-72032002000900008
Purpose: to study the influence of the prenatal care, fetal and maternal factors on the stillbirth rates of a university hospital from the south of Brazil. Methods :a case-control study of the cases of stillbirth occurred before the beginning of labor, from March 1998 to June 2001, at the Hospital Geral of Caxias do Sul University. The controls were selected among live newborns. The analysis of the quality of the prenatal care was based on the criteria established by the Programa de Humanização do Pré-natal e Nascimento of the Brazilian Health Ministry (2000). To evaluate possible risk factors for stillbirth we used the odds ratio (OR). Other confounding factors were evaluated by logistic regression. Results: preterm delivery was more prevalent in the cases of stillbirth (31.7+4.7 vs 38.6+0.9). The average birth weight among the stillborns was 1,705 g (+837 g), while in the controls it was 3,080 g (+576 g). Prenatal care was observed in 81.5% of the stillbirths and in 91.6% of the control group. The initial analysis showed that three factors were associated with stillbirth: inadequate prenatal care (43.6 vs 23.4%), history of previous stillbirth (6.6 vs 0.9%) and maternal age (27+7.9 years vs 24+6.4 years). Nevertheless, after adjustment of these variables through logistic regression, only the maternal age maintained its association with the stillbirth rates. Conclusions: in the present study, the strongest factor associated with the occurrence of stillbirth was the increase in maternal age.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2002;24(8):505-510
DOI 10.1590/S0100-72032002000800002
Purpose: to evaluate if multiple courses of antenatal corticosteroids are more effective than single ones to reduce morbidity and mortality of preterm infants. Methods: retrospective study of 184 newborns with gestational age less than 34 weeks from a tertiary-level hospital in São Paulo from January 1988 to December 1998. The patients were divided into two groups: single course (n=135) - newborns whose mothers were exposed to a complete single course (2 doses of betamethasone or 4 doses of dexamethasone between 24 h and 7 days prior to delivery); multiple courses (n=49) - newborns whose mothers were exposed to two or more complete courses. The primary clinical outcomes for the two groups were: frequency of respiratory distress syndrome (RDS), intra-hospital mortality and combined neonatal morbidity (including the presence of the following: RDS, peri-intraventricular hemorrhage, bronchopulmonary dysplasia, necrotizing enterocolitis, sepsis or intra-hospital death). Numerical data were compared by Student's t test or Mann-Whitney test and categorical data by chi² or Fisher exact test, with the odds ratio and its confidence interval. Results: there were no differences between the groups that received single or multiple courses of antenatal corticosteroids in regard to the occurrence of RDS (single course: 22% and multiple course: 18%), intra-hospital mortality (single course 18% and multiple 12%) and combined neonatal morbidity (single course 62% and multiple 63%). Conclusions: multiple courses of antenatal corticosteroids did not reduce the morbidity and mortality of preterm infants. This study emphasizes the present guidelines that recommend the use of one single course of corticosteroid for fetal maturation in pregnant women at risk for preterm delivery.