Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo5
This study aims to correlate pelvic ultrasound with female puberty and evaluate the usual ultrasound parameters as diagnostic tests for the onset of puberty and, in particular, a less studied parameter: the Doppler evaluation of the uterine arteries.
Cross-sectional study with girls aged from one to less than eighteen years old, with normal pubertal development, who underwent pelvic ultrasound examination from November 2020 to December 2021. The presence of thelarche was the clinical criterion to distinguish pubescent from non-pubescent girls. The sonographic parameters were evaluated using the ROC curve and the cutoff point defined through the Youden index (J).
60 girls were included in the study. Uterine volume ≥ 2.45mL had a sensitivity of 93%, specificity of 90%, PPV of 90%, NPV of 93% and accuracy of 91% (AUC 0.972) for predicting the onset of puberty. Mean ovarian volume ≥ 1.48mL had a sensitivity of 96%, specificity of 90%, PPV of 90%, NPV of 97% and accuracy of 93% (AUC 0.966). Mean PI ≤ 2.75 had 100% sensitivity, 48% specificity, 62% PPV, 100% NPV and 72% accuracy (AUC 0.756) for predicting the onset of puberty.
Pelvic ultrasound proved to be an excellent tool for female pubertal assessment and uterine and ovarian volume, the best ultrasound parameters for detecting the onset of puberty. The PI of the uterine arteries, in this study, although useful in the pubertal evaluation, showed lower accuracy in relation to the uterine and ovarian volume.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo10
To analyze data of patients with symptomatic pelvic organ prolapse evaluated with PFDI20 and its subscales to report the prevalence of lower gastrointestinal symptoms and anal incontinence in the population of a public hospital and analyze its impact on quality of life.
Cross-sectional study of patients with symptomatic POP. Patients were evaluated with demographic data, POP-Q, pelvic floor ultrasonography, urological parameters, and pelvic floor symptoms (PFDI-20), and quality of life (P-QoL) surveys. Patients were classified as CRADI-8 "positive" for colorectal symptoms, with responses "moderate" in at least 3 and/or "severe" in at least 2 of the items in the CRADI-8 questionnaires.
One hundred thirteen patients were included. 42.5% (48) were considered positive for colorectal symptoms on CRADI-8. 53.4% presented anal incontinence. No significant differences were found in sociodemographic variables, POP-Q stage, ultrasound parameters, or urological parameters. Positive patients had a significantly worse result in PFDI-20, POPDI (48 vs 28; p<0.001), UDI6 (51 vs 24; p<0.001), and in the areas of social limitation (44.4 vs 22.2; p = 0.045), sleep- energy (61.5 vs 44.4; p = 0.08), and severity (56.8 vs 43.7, p=0.015) according to P-QoL.
Moderate or severe colorectal symptoms are seen in 40% of patients with symptomatic POP in our unit. Full evaluation of pelvic floor dysfunction symptoms should be performed routinely in urogynecology units.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo11
To show the experience of a Latin American public hospital, with SNM in the management of either OAB, NOUR or FI, reporting feasibility, short to medium-term success rates, and complications.
A retrospective cohort was conducted using data collected prospectively from patients with urogynecological conditions and referred from colorectal surgery and urology services between 2015 and 2022.
Advanced or basic trial phases were performed on 35 patients, 33 (94%) of which were successful and opted to move on Implantable Pulse Generator (GG) implantation. The average follow-up time after definitive implantation was 82 months (SD 59). Of the 33 patients undergoing, 27 (81%)reported an improvement of 50% or more in their symptoms at last follow-up. Moreover, 30 patients (90%) with a definitive implant reported subjective improvement, with an average PGI-I "much better" and 9 of them reporting to be "excellent" on PGI-I.
SNM is a feasible and effective treatment for pelvic floor dysfunction. Its implementation requires highly trained groups and innovative leadership. At a nation-wide level, greater diffusion of this therapy among professionals is needed to achieve timely referral of patients who require it.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo13
The purpose of this study was to compare postoperative pain between SF flap and serratus anterior muscle (SM) in direct-to-implant breast reconstruction.
This is a prospective cohort study that included 53 women diagnosed with breast cancer who underwent mastectomy and one-stage implant-based breast reconstruction from January 2020 to March 2021. Twenty-nine patients (54.7%) had SF elevation, and 24 patients (45.3%) underwent SM elevation. We evaluated patient-reported early postoperative pain on the first day after surgery. Also, it was reported that all surgical complications in the first month and patient reported outcomes (PROs) were measured with the BRECON 23 questionnaire.
The serratus fascia group used implants with larger volumes, 407.6 ± 98.9 cc (p < 0.01). There was no significant difference between the fascial and muscular groups regarding the postoperative pain score reported by the patients (2 versus 3; p = 0.30). Also, there was no difference between the groups regarding early surgical complications and PROs after breast reconstruction.
The use of SF seems to cause less morbidity, which makes the technique an alternative to be considered in breast reconstruction. Although there was no statistical difference in postoperative pain scores between the fascia and serratus muscle groups.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo14
Postpartum hemorrhage (PPH) is the leading cause of maternal death globally. Therefore, prevention strategies have been created. The study aimed to evaluate the occurrence of PPH and its risk factors after implementing a risk stratification at admission in a teaching hospital.
A retrospective cohort involving a database of SISMATER® electronic medical record. Classification in low, medium, or high risk for PPH was performed through data filled out by the obstetrician-assistant. PPH frequency was calculated, compared among these groups and associated with the risk factors.
The prevalence of PPH was 6.8%, 131 among 1,936 women. Sixty-eight (51.9%) of them occurred in the high-risk group, 30 (22.9%) in the medium-risk and 33 (25.2%) in the low-risk group. The adjusted-odds ratio (OR) for PPH were analyzed using a confidence interval (95% CI) and was significantly higher in who presented multiple pregnancy (OR 2.88, 95% CI 1.28 to 6.49), active bleeding on admission (OR 6.12, 95% CI 1.20 to 4.65), non-cephalic presentation (OR 2.36, 95% CI 1.20 to 4.65), retained placenta (OR 9.39, 95% CI 2.90 to 30.46) and placental abruption (OR 6.95, 95% CI 2.06 to 23.48). Vaginal delivery figured out as a protective factor (OR 0.58, 95% CI 0.34 to 0.98).
Prediction of PPH is still a challenge since its unpredictable factor arrangements. The fact that the analysis did not demonstrate a relationship between risk category and frequency of PPH could be attributable to the efficacy of the strategy: Women classified as "high-risk" received adequate medical care, consequently.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo15
To compare the medical image interpretation's time between the conventional and automated methods of breast ultrasound in patients with breast lesions. Secondarily, to evaluate the agreement between the two methods and interobservers.
This is a cross-sectional study with prospective data collection. The agreement's degrees were established in relation to the breast lesions's ultrasound descriptors. To determine the accuracy of each method, a biopsy of suspicious lesions was performed, considering the histopathological result as the diagnostic gold standard.
We evaluated 27 women. Conventional ultrasound used an average medical time of 10.77 minutes (± 2.55) greater than the average of 7.38 minutes (± 2.06) for automated ultrasound (p<0.001). The degrees of agreement between the methods ranged from 0.75 to 0.95 for researcher 1 and from 0.71 to 0.98 for researcher 2. Among the researchers, the degrees of agreement were between 0.63 and 1 for automated ultrasound and between 0.68 and 1 for conventional ultrasound. The area of the ROC curve for the conventional method was 0.67 (p=0.003) for researcher 1 and 0.72 (p<0.001) for researcher 2. The area of the ROC curve for the automated method was 0. 69 (p=0.001) for researcher 1 and 0.78 (p<0.001) for researcher 2.
We observed less time devoted by the physician to automated ultrasound compared to conventional ultrasound, maintaining accuracy. There was substantial or strong to perfect interobserver agreement and substantial or strong to almost perfect agreement between the methods.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo16
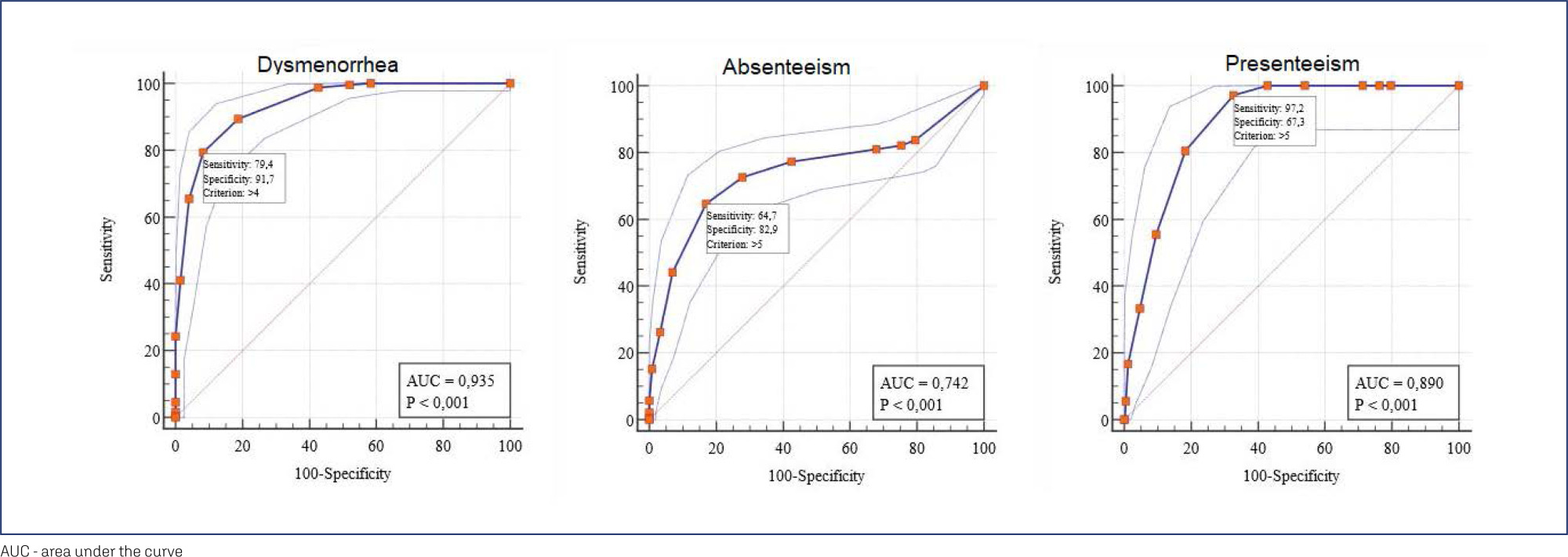
Dysmenorrhea is the pain related to menstruation; to screen for the symptoms, a working ability, location, intensity of days of pain, and dysmenorrhea (WaLIDD) score was created. The purpose of this work was to culturally adapt and assess the measurement properties of the WaLIDD score for dysmenorrhea in Brazilian women.
In this cross-sectional online study, we evaluated women with and without dysmenorrhea. Criterion validity and construct validity were assessed, respectively, by the Receiver Operator Characteristic (ROC) curve and correlations with the bodily pain and social functioning domains of medical outcomes study 36-item short-form health survey (SF-36), self-report of absenteeism and Stanford Presenteeism Scale for presenteeism. Test-retest reliability and measurement errors were assessed, respectively, by intraclass correlation coefficient (ICC) and Bland and Altman Graph.
430 women completed the test, 238 (55.4%) women had dysmenorrhea, and 199 (46.3%) answered the questionnaire twice for the retest. The cutoff points ≥4, ≥5, and ≥5 could discriminate between women with and without dysmenorrhea, absenteeism, and presenteeism related to dysmenorrhea, respectively. Correlations between SF-36 – pain and social functioning domains and WaLIDD score were weak to strong and negative. For WaLIDD total Score, ICC was 0.95 and the limits of agreement were −1.54 and 1.62.
WaLIDD score is a short, valid and reliable instrument to screen and predict dysmenorrhea and could predict absenteeism and presenteeism related to dysmenorrhea in Brazilian women.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2024;46:e-rbgo17
To determine the prevalence of anxiety, depression and burnout in residents of Gynecology and Obstetrics during COVID-19 pandemic in Brazil and its associated factors.
Cross-sectional study involving all regions of Brazil, through the application of a sociodemographic questionnaire, the Hospital Anxiety and Depression Scale (HAD) and the Maslach Burnout Inventory (MBI-HSS) instrument. Multivariate analysis was performed after adjusting the Poisson model.
Among the 719 participating medical residents, screening was positive for anxiety in 75.7% and for depression in 49.8% of cases. Burnout syndrome was evidenced in 41.3% of the physicians studied. Those with depression are more likely to have anxiety (OR 0.797; 95%CI 0.687 - 0.925) and burnout syndrome (OR 0.847 95%CI 0.74 - 0.97). Residents with anxiety (OR 0.805; 95%CI 0.699 - 0.928) and burnout (OR 0.841; 95%CI 0.734 - 0.963) are more likely to have depression.
High prevalence of anxiety, depression and burnout were found in residents of Gynecology and Obstetrics in Brazil, in addition to important correlations between anxiety-depression and depression-burnout.