Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):452-457
To detect depression during pregnancy and in the immediate postpartum period using the Edinburgh postpartum depression scale (EPDS).
Cross sectional study of 315 women, aged between 14 and 44 years, who received perinatal care at the Leonor Mendes de Barros Hospital, in São Paulo, between July 1st, 2019 and October 30th, 2020. The cutoff point suggesting depression was ≥ 12.
The screening indicated 62 (19.7%) patients experiencing depression. Low family income, multiparity, fewer prenatal appointments, antecedents of emotional disorders, dissatisfaction with the pregnancy, poor relationship with the partner, and psychological aggression were all risk factors associated with depression in pregnancy or in the immediate postpartum period. Antecedents of depression and psychology aggression during pregnancy were significant variables for predicting perinatal depression in the multivariate analysis.
There is a significant association between the occurrence of perinatal depression and the aforementioned psychosocial factors. Screening patients with the EPDS during perinatal and postpartum care could facilitate establishing a line of care to improve the wellbeing of mother and infant.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):47-54
To evaluate the assistance provided to women victims of sexual violence and their participation in the follow-up treatment after the traumatic event, presenting a sociodemographic profile, gynecological background, and circumstances of the event, and reporting the results, acceptance, and side effects of prophylaxis for sexually transmitted infections (STIs) and pregnancy.
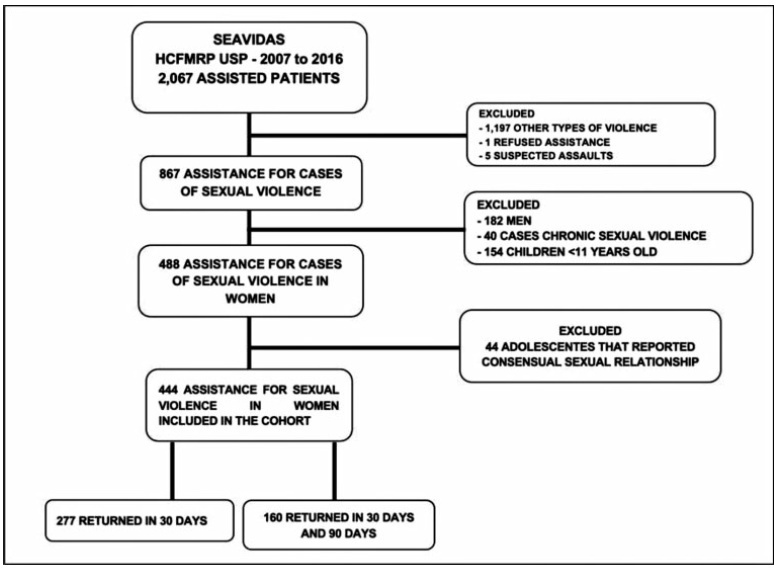
A retrospective cohort study comprising the period between 2007 and 2016. All women receiving medical care and clinical follow-up after a severe episode of sexual violence were included. Records of domestic violence, male victims, children, and adolescents who reported consensual sexual activity were excluded. The present study included descriptive statistics as frequencies and percentages.
A total of 867medical records were reviewed and 444 cases of sexual violence were included. The age of the victims ranged from10 to 77 years old, most of them selfdeclared white, with between 4 and 8 years of education, and denying having a sexual partner. Sexual violence occurred predominantly at night, on public thoroughfare, being committed by an unknown offender. Most victims were assisted at the referral service center within 72 hours after the violence, enabling the recommended prophylaxis. There was high acceptance of antiretroviral therapy (ART), although half of the users reported side effects. Seroconversion to human immunodeficiency virus (HIV) or to hepatitis B virus (HBV) was not detected in women undergoing prophylaxis.
In the present cohort, the profile of victims of sexual violence was loweducated, young, white women. The traumatic event occurred predominantly at night, on public thoroughfare, being committed by an unknown offender. Assistance within the first 72 hours after sexual violence enables the healthcare center to provide prophylactic interventions against STIs and unwanted pregnancies.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):40-46
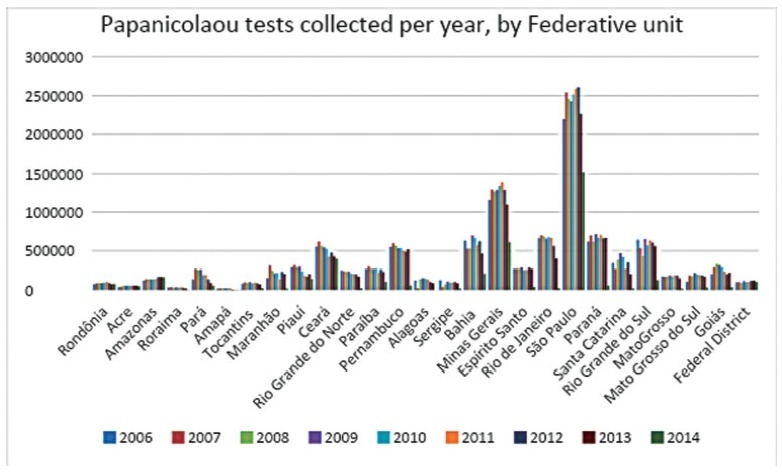
To analyze the quantity of cervical smears, also designated Papanicolaou tests, between 2006 and 2015 in all the Federal units of Brazil, as well as to verify the quantity of exams collected outside the recommended age range and the economic impact of such excess.
The data was collected from the Ministry of Health’s database called Sistema de Informação do Câncer do Colo de Útero (SISCOLO), which contains all the test results collected nationwide by the Unified Health System (SUS, in the Portuguese acronym). From that, the number of exams and the age range of thewomen who underwent them were analyzed; besides, these numbers were stratified according to the state of where the exam was performed. The quantity of exams collected outside the recommended age range was verified, and, so, the economic impact generated was noted.
Between 2006and2015, 87,425,549Papanicolaoutestswere collected in Brazil. Of these, 20,215,052 testswere collected outside the age range recommended by the Brazilian Ministry of Health; this number corresponded to 23.12% of all exams. From such data, considering that each Pap smear collected by SUS generates a cost of BRL 7.30 to the government, according to the information in the Tabela SUS dated September 2018, there was a total charge of BRL 147,569,880 for tests collected outside the protocol.
In Brazil, according to the Ministry of Health’s protocol about the recommended practices on collecting Pap smears, whose newest edition dates of 2016, it is recommended that Pap smears are collected inwomen from a specific age range, inwhom the potential diagnosing advantages overcome the onus of overdiagnosis or of a lesion with great regression potential. However, such protocols have not been correctly followed, promoting more than 20 million tests in excess, and an exorbitant cost for the Brazilian public health system. It is relevant to take measures to correctly use the official protocol, reducing the patients risks, as well as the economic impact for SUS.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):32-39
To evaluate the improvement in screening accuracy of the Fracture Risk Assessment Tool (FRAX) for the risk of developing osteoporosis among young postmenopausal women by associating with it clinical muscle mass measures.
A sample of postmenopausal women was submitted to calcaneal quantitative ultrasound (QUS), application of the FRAX questionnaire, and screening for the risk of developing sarcopenia at a health fair held in the city of São Bernardo do Campo in 2019. The sample also underwent anthropometric measurements, muscle mass, walking speed and handgrip tests. A major osteoporotic fracture (MOF) risk ≥ 8.5% on the FRAX, a classification of medium risk on the clinical guideline of the National Osteoporosis Guideline Group (NOGG), and a QUS T-score ≤ -1.8 sd were considered risks of having low bone mass, and QUS T-score ≤ -2.5sd, risk of having fractures.
In total, 198 women were evaluated, with a median age of 64±7.7 years, median body mass index (BMI) of 27.3±5.3 kg/m2 and median QUS T-score of -1.3±1.3 sd. The accuracy of the FRAX with a MOF risk ≥ 8.5% to identify women with T-scores ≤ -1.8 sd was poor, with an area under the curve (AUC) of 0.604 (95% confidence interval [95%CI]: 0.509-0.694) for women under 65 years of age, and of 0.642 (95%CI: 0.571-0.709) when age was not considered. Including data on muscle mass in the statistical analysis led to a significant improvement for the group of women under 65 years of age, with an AUC of 0,705 (95%CI: 0.612-0.786). The ability of the high-risk NOGG tool to identify T-scores ≤ -1.8 sd was limited.
Clinical muscle mass measurements increased the accuracy of the FRAX to screen for osteoporosis in women aged under 65 years.

Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):3-9
To compare the outcomes of emergency and planned peripartum hysterectomies.
The present retrospective cross-sectional study was conducted in two hospitals. Maternal and neonatal outcomes were compared according to emergency and planned peripartum hysterectomies.
A total of 34,020 deliveries were evaluated retrospectively, and 66 cases of peripartum hysterectomy were analyzed. Of these, 31 were cases of planned surgery, and 35 were cases of emergency surgery. The patients who underwent planned peripartum hysterectomy had a lower rate of blood transfusion (83.9% versus 100%; p=0.014), and higher postoperative hemoglobin levels (9.9±1.3 versus 8.3±1.3; p<0.001) compared with the emergency hysterectomy group. The birth weight was lower, although the appearance, pulse, grimace, activity, and respiration (Apgar) scores were higher in the planned surgery group compared with the emergency cases.
Planned peripartum hysterectomy with an experienced team results in less need for transfusion and improved neonatal outcomes compared with emergency peripartum hysterectomy.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(1):19-24
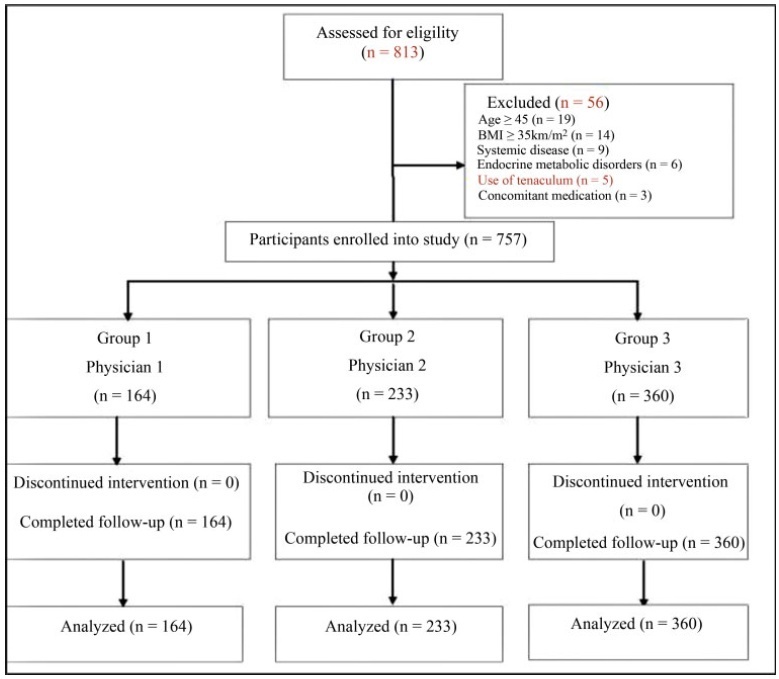
To evaluate whether there is an effect of the physician who transfers the embryos on pregnancy rates in in vitro fertilization-intracytoplasmic sperm injection (IVF-ICSI) treatment.
A total of 757 participants were analyzed between 2012 and 2017. Participants were classified according to 3 physicians who transferred the embryos: ([group 1=164 patients]; [group 2=233 patients]; [group 3=360 patients]). Baseline parameters and IVF-ICSI outcomes were compared between the groups.
No differences were determined between the groups regarding the baseline parameters (age, age subgroups [20-29, 30-39, and ≥ 40 years old)], body mass index (BMI), smoking status, infertility period, cause of infertility, baseline follicle stimulating hormone, luteinizing hormone, estradiol (E2), thyroid stimulating hormone, prolactin levels, antral follicle count, duration of stimulation, stimulation protocol, gonadotropin dose required, maximum E2 levels, progesterone levels, endometrial thickness on human chorionic gonadotropin (hCG) administration and transfer days (p>0.05). The numbers of oocytes retrieved,metaphase II (MII), 2 pronucleus (2PN), transferred embryo, fertilization rate, day ofembryo transfer, the catheter effect and embryo transfer technique, and clinical pregnancy rates (CPRs) were also comparable between the groups (p>0.05).
Our data suggests that the physician who transfers the embryos has no impact on CPRs in patients who have undergone IVF-ICSI, but further studies with more participants are required to elucidate this situation.
Summary
Revista Brasileira de Ginecologia e Obstetrícia. 2022;44(5):489-496
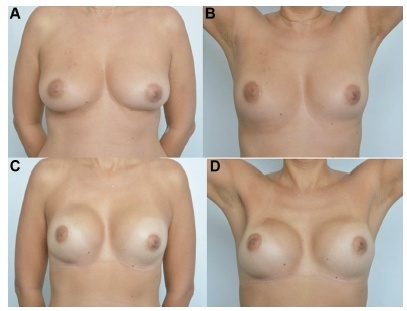
Few studies analyzed the safety of salvage nipple-sparing mastectomy (NSM) for local relapse treatment. We evaluated the outcomes of patients with indications for mastectomy who chose to undergo NSM for ipsilateral breast tumor recurrence (IBTR).
Between January 2001 and December 2018, we evaluated 24 women who underwent NSM for local relapse after conservative surgery.
Thepatientswere followedupfor amean time of132months since thefirst surgery. After the NSM, 5 (20.8%) patients were diagnosed with local recurrence and only 1 (4.2%) patient died. The patients presented 4.8% (2) of partial and 2.4% (1) of total nipple necrosis.
In this long-term follow-up since the first surgery, we observed low rates of complication and good survival, although associated with high local recurrence in patients diagnosed with IBTR undergoing NSM as salvage surgery.We demonstrated that NSMmay be considered after IBTR for patients who did not want to undergo total mastectomy.